Why Is Sacral Nerve Pain Worse While Sleeping?
If you suffer from sacral nerve pain, you may have noticed that it tends to worsen while you are sleeping. This can be quite frustrating, as sleep is supposed to be a time for rest and rejuvenation. In this article, we will explore the reasons why sacral nerve pain intensifies at night and discuss strategies for managing pain to improve your sleep quality.
Understanding Sacral Nerve Pain
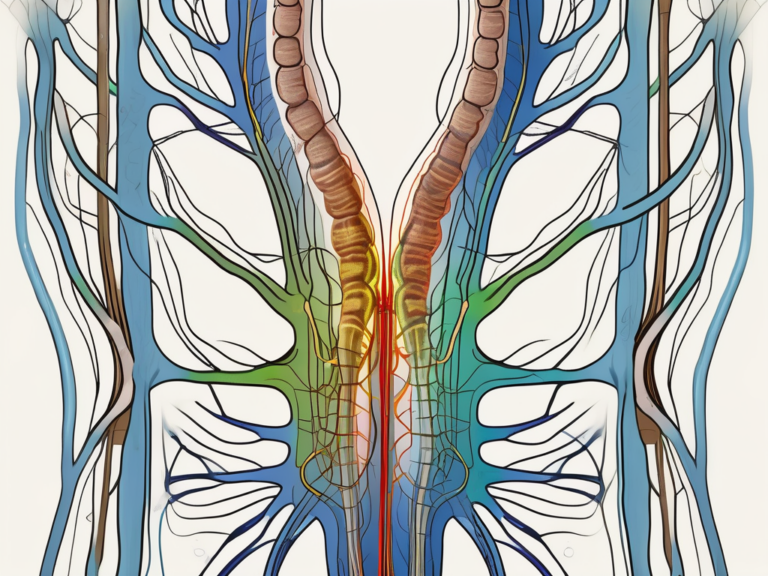
Sacral nerve pain refers to discomfort that originates from the sacral nerves, which are located in the lower back and pelvic region. These nerves play a crucial role in transmitting sensory information and controlling the function of various muscles in the lower body. When these nerves become irritated or compressed, it can lead to pain, numbness, and tingling sensations.
The Anatomy of the Sacral Nerve
The sacral nerve is comprised of a network of nerves that branch off from the spinal cord. It extends down through the pelvis and innervates the lower back, buttocks, and legs. The sacral nerve is responsible for transmitting signals between the brain and the lower body, allowing for movement, sensation, and control of bodily functions.
Common Causes of Sacral Nerve Pain
There are several factors that can contribute to sacral nerve pain. These include:
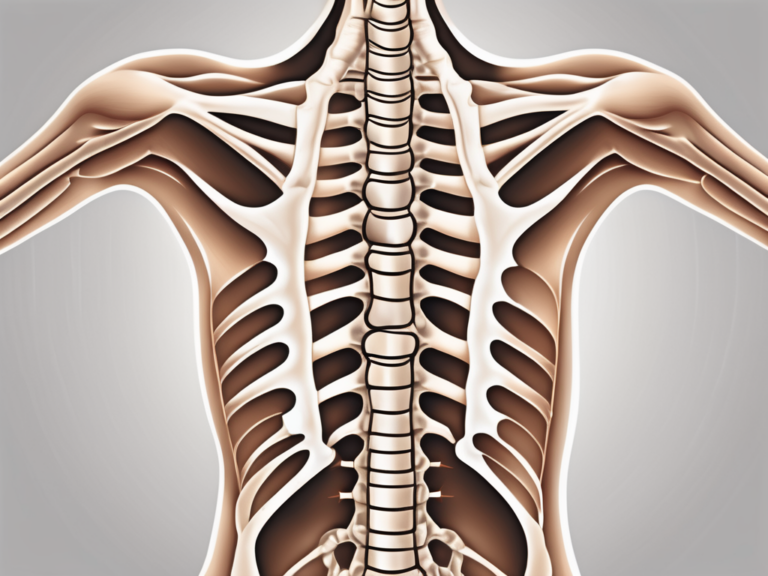
- Herniated discs: When the cushioning discs between the vertebrae in the lower back become damaged or ruptured, they can put pressure on the sacral nerves.
- Sciatica: This condition occurs when the sciatic nerve, which is the largest nerve in the body, becomes compressed or irritated. It can cause pain that radiates down the buttocks and legs.
- Spinal stenosis: This is a narrowing of the spinal canal, which can result in pressure on the sacral nerves.
If you are experiencing sacral nerve pain, it is important to consult with a healthcare professional for an accurate diagnosis and appropriate treatment plan.
Sacral nerve pain can have a significant impact on a person’s daily life. The discomfort and limitations it causes can make it difficult to perform simple tasks, such as sitting, standing, or walking. Additionally, the pain can interfere with sleep and overall quality of life.
One of the most common causes of sacral nerve pain is a herniated disc. This occurs when the soft, jelly-like center of a spinal disc pushes through a crack in the tougher exterior. When this happens in the lower back, it can put pressure on the sacral nerves, leading to pain and other symptoms. Herniated discs can be caused by age-related wear and tear, injury, or improper lifting techniques.
Another condition that can cause sacral nerve pain is sciatica. The sciatic nerve is the longest and widest nerve in the body, running from the lower back down through the buttocks and into the legs. When this nerve becomes compressed or irritated, it can cause pain that radiates down the back of the leg. This pain can be sharp, shooting, or burning in nature and may be accompanied by numbness, tingling, or muscle weakness.
Spinal stenosis is another common cause of sacral nerve pain. This condition occurs when the spinal canal narrows, putting pressure on the nerves within the spine. As the sacral nerves pass through the spinal canal, any narrowing can lead to irritation and pain. Spinal stenosis can be caused by age-related changes in the spine, such as the formation of bone spurs or thickening of ligaments.
It is important to seek medical attention if you are experiencing sacral nerve pain. A healthcare professional can perform a thorough evaluation, including a physical examination and imaging tests, to determine the underlying cause of your symptoms. Treatment options may include medication, physical therapy, injections, or in some cases, surgery.
The Relationship Between Sleep and Pain
Sleep plays a crucial role in our overall health and well-being. It allows our bodies to rest and repair, and it contributes to our cognitive function and emotional well-being. However, sleep disturbance is common among individuals with chronic pain conditions, including sacral nerve pain.
When we think about sleep, it’s not just a simple state of unconsciousness. It’s a complex process that involves different stages and cycles. During sleep, our bodies go through different cycles, including rapid eye movement (REM) sleep and non-REM sleep. These cycles are important for restorative processes, such as tissue repair, hormone regulation, and memory consolidation.
Disruptions to these sleep cycles can impact pain perception and our ability to cope with discomfort. Poor sleep quality has been associated with increased sensitivity to pain and a higher likelihood of experiencing pain flare-ups. It’s like a vicious cycle – pain disrupts sleep, and lack of sleep worsens pain.
The Science of Sleep
Let’s dive deeper into the science of sleep. During non-REM sleep, our bodies experience slow-wave sleep (SWS) and light sleep. SWS is the deepest stage of sleep, where our brain waves slow down, and our bodies enter a state of relaxation. This stage is crucial for physical restoration, as it promotes the release of growth hormone, repairs tissues, and strengthens the immune system.
On the other hand, REM sleep is the stage where most dreaming occurs. It is characterized by rapid eye movements, increased brain activity, and temporary paralysis of the muscles. REM sleep is essential for cognitive processes, emotional regulation, and memory consolidation. It’s like a mental workout for our brains, helping us process and make sense of the information we encountered during the day.
Now, imagine the impact of disrupted sleep on these important processes. When we can’t achieve deep, restorative sleep due to pain, our bodies miss out on the opportunity to repair and rejuvenate. Our hormone levels may become imbalanced, affecting our mood and overall well-being. Additionally, the lack of REM sleep can impair our cognitive function, making it harder to concentrate and remember things.
How Pain Affects Sleep Quality
Experiencing pain can make it challenging to fall asleep and stay asleep throughout the night. The discomfort and sensations associated with sacral nerve pain can cause restlessness and frequent awakenings. It’s like a constant battle between finding a comfortable position and trying to ignore the pain signals.
Furthermore, pain can lead to increased muscle tension and stress, further contributing to sleep disturbances. When we’re in pain, our bodies naturally tense up as a protective mechanism. This muscle tension can make it difficult to relax and drift off into a peaceful slumber. The stress caused by chronic pain can also activate our body’s fight-or-flight response, releasing stress hormones that keep us alert and on edge.
It is important to address both pain management and sleep hygiene to improve your sleep quality and overall well-being. Seeking appropriate medical treatment for your sacral nerve pain and implementing healthy sleep habits can make a significant difference in your sleep and pain levels. Remember, a good night’s sleep is not just a luxury; it’s a necessity for your physical and mental health.
Why Sacral Nerve Pain Intensifies at Night
Many individuals with sacral nerve pain report that their symptoms tend to worsen at night. There are several reasons why this may occur.
The Role of Body Position
When we lie down, particularly on our sides or on our back, the pressure on our lower back and pelvis increases. This can exacerbate the compression of the sacral nerves and intensify the pain. Additionally, certain sleeping positions may contribute to poor spinal alignment, further aggravating the symptoms.
Exploring different sleep positions and using supportive pillows or cushions may help alleviate some of the discomfort associated with sacral nerve pain.
For example, sleeping on your side with a pillow between your knees can help maintain proper spinal alignment and reduce pressure on the sacral nerves. Alternatively, sleeping on your back with a pillow under your knees can also help relieve the pressure on your lower back.
It is important to find a sleep position that works best for you and provides the most relief from sacral nerve pain. Experimenting with different positions and using supportive aids can make a significant difference in your comfort levels during sleep.
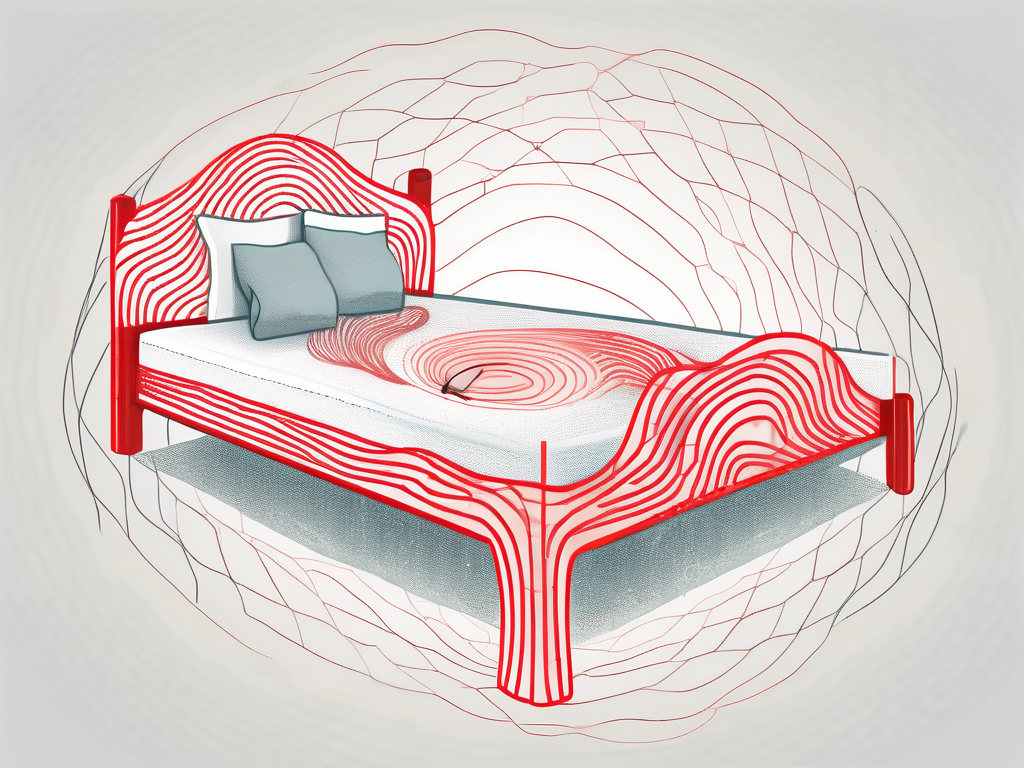
Impact of Sleep Environment
The quality of your sleep environment can significantly influence your sleep and pain levels. Factors such as mattress firmness, pillow support, and room temperature can all impact your comfort and overall sleep experience. If your sleep environment is not conducive to relaxation and support, it may contribute to increased sacral nerve pain at night.
Choosing the right mattress and pillows is crucial for individuals with sacral nerve pain. A mattress that is too firm or too soft can lead to improper spinal alignment and increased pressure on the sacral nerves. Opting for a medium-firm mattress that provides adequate support and cushioning can help alleviate pain during sleep.
Similarly, using pillows that provide proper support for your neck and back can help maintain spinal alignment and reduce pressure on the sacral nerves. Memory foam or contour pillows are often recommended for individuals with sacral nerve pain as they conform to the shape of your body and provide targeted support.
In addition to mattress and pillow selection, the temperature and overall ambiance of your sleep environment can also impact your pain levels. A cool and well-ventilated room can promote better sleep quality and reduce inflammation, which may help alleviate sacral nerve pain.
Creating a relaxing sleep environment can involve incorporating calming elements such as soft lighting, soothing scents, and noise reduction techniques. These can help promote a sense of tranquility and aid in pain management.
It is worth considering investing in a supportive mattress and pillows, as well as creating a sleep environment that promotes relaxation and restfulness. Taking steps to optimize your sleep environment can contribute to reducing sacral nerve pain and improving overall sleep quality.
Managing Sacral Nerve Pain for Better Sleep
Living with sacral nerve pain can be challenging, especially when it comes to getting a good night’s sleep. The discomfort and throbbing sensations can make it difficult to find a comfortable position and relax. However, there are various strategies that may help improve your sleep quality and alleviate sacral nerve pain. It is crucial to consult with a healthcare professional for personalized advice and guidance tailored to your specific needs.
Non-Medical Interventions
While medical interventions are available, there are also several non-medical interventions that may be beneficial in managing sacral nerve pain. These interventions focus on natural methods to alleviate pain and promote relaxation. Some of these non-medical interventions include:
- Physical therapy: A physical therapist can provide exercises and stretches to help strengthen the muscles supporting the lower back and pelvis, as well as improve flexibility and posture. These exercises can target specific areas affected by sacral nerve pain, providing relief and promoting better sleep.
- Heat and cold therapy: Applying heat or cold packs to the affected area can help alleviate pain and reduce inflammation. Heat therapy can relax the muscles and increase blood flow, while cold therapy can numb the area and reduce swelling. These simple yet effective techniques can be incorporated into your bedtime routine to help you find comfort and ease before sleep.
- Relaxation techniques: Engaging in relaxation techniques, such as deep breathing, meditation, and gentle stretches, can help reduce muscle tension and promote a sense of calm before bedtime. These techniques can help relax both the body and mind, creating an optimal environment for restful sleep.
It is important to approach these interventions with guidance from a healthcare professional to ensure safety and effectiveness. They can provide personalized recommendations and monitor your progress, making adjustments as needed to optimize your sleep and manage sacral nerve pain.
Medical Treatments for Sacral Nerve Pain
In some cases, non-medical interventions may not provide sufficient relief, and medical treatments may be necessary to manage sacral nerve pain. These medical interventions are aimed at addressing the underlying causes of the pain and providing targeted relief. Some of the medical treatments for sacral nerve pain include:
- Pain medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, and opioids may be prescribed to alleviate pain and reduce inflammation. These medications can help manage the symptoms of sacral nerve pain, allowing for better sleep and improved quality of life.
- Injections: Corticosteroid injections can help reduce inflammation and provide temporary relief from sacral nerve pain. These injections target the specific area of pain, providing targeted relief and reducing discomfort, which can significantly improve sleep quality.
- Surgical interventions: In severe cases, when other treatments have not been effective, surgery may be recommended to address the underlying cause of sacral nerve pain, such as a herniated disc or spinal stenosis. Surgical interventions aim to correct the structural issues causing the pain, offering long-term relief and improved sleep quality.
It is important to have a thorough discussion with your healthcare provider to weigh the potential risks and benefits of these medical treatments. They can provide you with the necessary information and guidance to make an informed decision about your treatment options.
Remember, managing sacral nerve pain is a journey, and finding the right combination of interventions may take time. By working closely with your healthcare provider and exploring both non-medical and medical treatments, you can take steps towards better sleep and improved overall well-being.
Preventing Future Sacral Nerve Pain
While it may not be possible to completely prevent sacral nerve pain, there are steps you can take to minimize the risk of future flare-ups.
Lifestyle Changes for Pain Prevention
Making certain lifestyle changes can contribute to the prevention of sacral nerve pain. These can include:
- Maintaining a healthy weight: Excess weight can put added stress on the lower back and pelvis, increasing the risk of sacral nerve pain.
- Practicing good posture: Maintaining proper posture while sitting, standing, and lifting can help reduce strain on the lower back and pelvis.
- Engaging in regular exercise: Regular physical activity, such as walking, swimming, and yoga, can help strengthen the muscles supporting the lower back and promote flexibility and range of motion.
Consulting with a healthcare professional or physical therapist can provide guidance on specific exercises and lifestyle modifications that may be most beneficial for you.
Exercises to Strengthen the Sacral Region
Specific exercises targeting the muscles supporting the sacral region can help improve stability, flexibility, and overall function. These exercises may include pelvic floor exercises, hip bridges, and gentle core strengthening exercises.
It is important to start slowly and gradually increase the intensity and duration of your exercise routine. Working with a physical therapist can ensure proper form and reduce the risk of further injury.
When to Seek Medical Help
While sacral nerve pain can often be managed with non-medical interventions, there are situations where medical intervention is necessary.
Recognizing Severe Sacral Nerve Pain
If you experience any of the following symptoms, it is important to seek medical help promptly:
- Severe, persistent pain that does not respond to self-care measures
- Loss of function or weakness in the lower back, pelvis, or legs
- Bowel or bladder dysfunction
- Numbness or tingling sensations in the genital area
- Fever or signs of infection
These symptoms may indicate a more serious underlying condition and require immediate medical attention.
Importance of Timely Medical Intervention
Timely medical intervention can help diagnose the underlying cause of your sacral nerve pain and provide appropriate treatment options. A healthcare professional can evaluate your symptoms, conduct necessary diagnostic tests, and develop an individualized care plan to help manage your pain and improve your sleep quality.
In conclusion, sacral nerve pain can be particularly troublesome during sleep, often interrupting your rest and making it difficult to find relief. By understanding the reasons why sacral nerve pain intensifies at night and implementing strategies for managing pain, you can improve your sleep quality and overall well-being. Remember to consult with a healthcare professional for accurate diagnosis and personalized treatment recommendations. With proper care and support, you can effectively manage your sacral nerve pain and enjoy restful nights of sleep.