When Would a Sacral Nerve Stimulator Need to Be Removed?
A sacral nerve stimulator is a medical device used to manage certain conditions such as overactive bladder and urinary incontinence. While it can be highly effective in providing relief and improving the quality of life for individuals suffering from these conditions, there are instances when the device may need to be removed. In this article, we will explore the reasons for sacral nerve stimulator removal, the removal process, alternatives to sacral nerve stimulation, and factors to consider when making the decision. It is important to note that this article is for informational purposes only and should not be considered as medical advice. If you are considering or have concerns about the removal of a sacral nerve stimulator, it is recommended that you consult with your healthcare provider for personalized guidance.
Understanding Sacral Nerve Stimulators
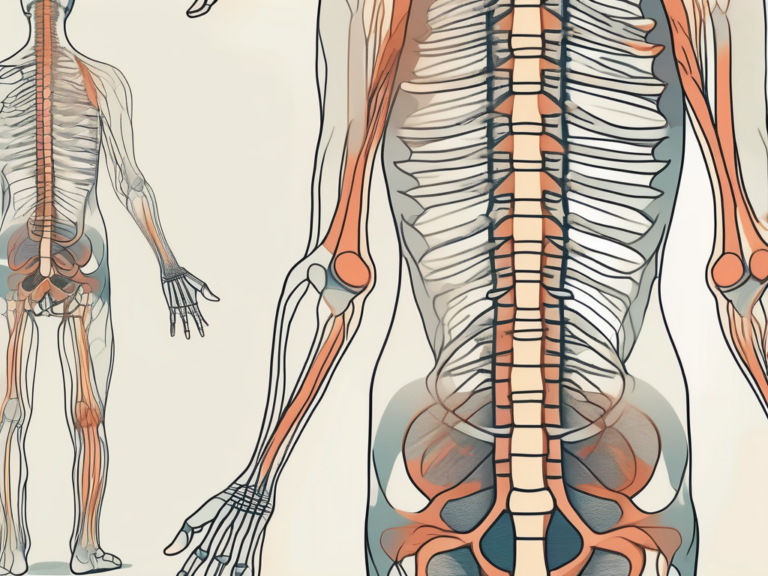
Sacral nerve stimulators are implantable devices that work by delivering electrical impulses to the sacral nerves, which are responsible for controlling the bladder and bowel function. These devices are typically recommended when conservative treatments have failed to provide adequate relief.
The sacral nerve stimulator is a remarkable medical device that has revolutionized the treatment of bladder and bowel dysfunction. By delivering precise electrical impulses to the sacral nerves, it helps restore normal function and improve the quality of life for many patients.
What is a Sacral Nerve Stimulator?
A sacral nerve stimulator is a small device that is surgically implanted under the skin in the buttock area. It consists of a generator, which produces the electrical impulses, and one or more thin wires, called leads, that are placed near the sacral nerves.
The generator of the sacral nerve stimulator is a sophisticated piece of technology that is designed to deliver the electrical impulses in a controlled and precise manner. It is powered by a long-lasting battery that ensures continuous stimulation for an extended period of time.
The leads of the sacral nerve stimulator are carefully positioned near the sacral nerves to ensure optimal stimulation. These leads are made of biocompatible materials that are safe for long-term implantation in the body. They are also designed to be flexible and durable, allowing for comfortable movement and minimal risk of damage.
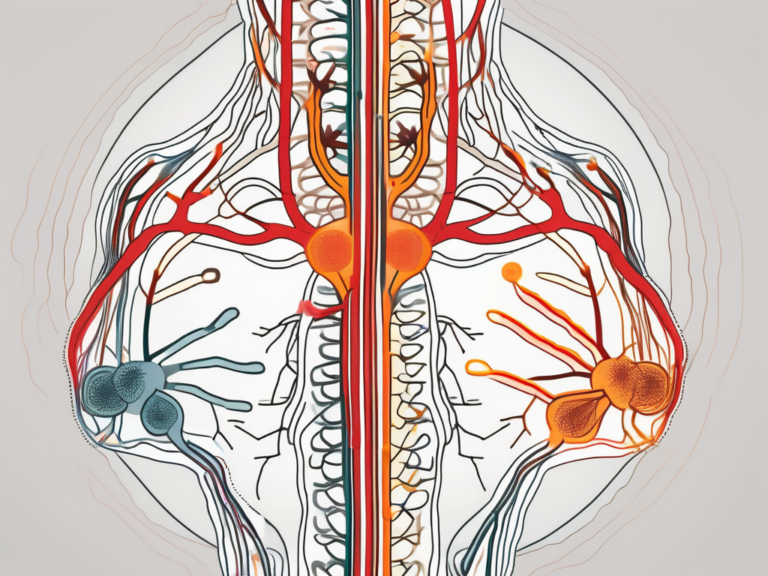
How Does a Sacral Nerve Stimulator Work?
When the device is activated, it generates mild electrical pulses that stimulate the sacral nerves, helping to regulate the bladder and bowel function. The level of stimulation can be adjusted based on individual needs and preferences.
The sacral nerve stimulator works by modulating the signals sent by the sacral nerves to the brain. By delivering precise electrical impulses, it can help restore the balance between the nerves and improve the communication between the bladder, bowel, and the brain.
One of the key advantages of the sacral nerve stimulator is its ability to be customized to each patient’s unique needs. The stimulation parameters, such as the frequency, intensity, and duration of the electrical pulses, can be adjusted by the healthcare provider to achieve the best possible outcomes.
Moreover, the sacral nerve stimulator is equipped with advanced programming options that allow for personalized therapy. It can be programmed to deliver different patterns of stimulation at different times of the day, depending on the patient’s specific requirements.
Overall, the sacral nerve stimulator is a remarkable medical device that has transformed the lives of many individuals suffering from bladder and bowel dysfunction. Its ability to restore normal function and improve quality of life has made it a valuable treatment option for those who have not found relief with conservative therapies.
Reasons for Sacral Nerve Stimulator Removal
While sacral nerve stimulators can provide significant benefits, there are certain situations where removal may be necessary. It is important to remember that these decisions are made on an individual basis in consultation with a healthcare provider. Some potential reasons for removal include:
Infection Risks and Complications
Although rare, infections can occur at the site of the device implantation. In some cases, these infections may not respond adequately to antibiotics and may require device removal. The risk of infection can be influenced by various factors, such as the patient’s overall health, the surgical technique used during implantation, and the presence of any pre-existing conditions that may compromise the immune system.
In addition to infections, complications such as erosion of the leads can also pose a risk. Over time, the constant stimulation of the sacral nerves may cause the leads to erode, leading to pain, discomfort, or even damage to surrounding tissues. In such cases, removal of the device may be necessary to address these complications and prevent further harm.
Device Malfunction or Failure
While sacral nerve stimulators are designed to be durable and reliable, there is a small risk of device malfunction or failure over time. This can occur due to various reasons, including mechanical issues, electrical problems, or damage to the device components. When a device malfunctions, it may not deliver the intended stimulation or may deliver it inconsistently, resulting in suboptimal symptom management. In such cases, the device may need to be removed and replaced with a new one to ensure optimal functioning and symptom control.
Changes in Medical Condition
Individuals with sacral nerve stimulators may experience changes in their medical condition that can make the ongoing use of the device unnecessary or less beneficial. For instance, if the underlying condition improves significantly, such as a reduction in symptoms or the resolution of the condition itself, the continued use of the device may no longer be required. In such cases, removal of the device can be considered to avoid unnecessary interventions and potential risks associated with long-term device use.
Furthermore, treatment goals may evolve over time, and the sacral nerve stimulator may no longer align with the new objectives. For example, if a patient’s treatment plan shifts towards a more conservative approach or if alternative therapies become available that offer better outcomes, removal of the device may be considered as part of the overall treatment strategy.
It is essential for individuals with sacral nerve stimulators to have regular follow-up appointments with their healthcare providers. These appointments allow for ongoing assessment of the device’s effectiveness, monitoring for any potential complications or changes in the patient’s medical condition, and discussion of the need for device removal if necessary. The decision to remove a sacral nerve stimulator is a complex one that requires careful consideration of the individual’s unique circumstances and goals.
The Removal Process of Sacral Nerve Stimulators
When the decision to remove a sacral nerve stimulator has been made, the process typically involves several steps, including preparation for the procedure, the removal itself, and post-removal care.
Preparing for the Procedure
Prior to removal, your healthcare provider will likely perform a thorough evaluation to assess your overall health and to ensure that it is safe to proceed with the removal process. This may involve a physical examination, review of medical history, and possibly diagnostic tests.
During the evaluation, your healthcare provider will discuss the reasons for removing the sacral nerve stimulator and address any concerns or questions you may have. They will explain the potential risks and benefits of the procedure, as well as any alternative treatment options that may be available.
Once it is determined that you are a suitable candidate for removal, your healthcare provider will provide you with detailed instructions on how to prepare for the procedure. This may include guidelines on fasting before the surgery, discontinuing certain medications, and arranging for transportation to and from the medical facility.
Additionally, your healthcare provider may recommend that you consult with a physical therapist or pain management specialist to develop a plan for managing your symptoms after the removal of the sacral nerve stimulator.
What to Expect During Removal
The removal procedure is usually performed in an outpatient setting under local or general anesthesia, depending on the individual circumstances. Prior to the procedure, you will be given specific instructions on what to do and what to expect.
Once you arrive at the medical facility, you will be taken to a preoperative area where you will meet with the surgical team. They will review your medical history, confirm the details of the procedure, and answer any last-minute questions you may have.
After the necessary preparations are made, you will be taken to the operating room. The anesthesia team will administer the chosen anesthesia, ensuring your comfort throughout the procedure. Once you are adequately sedated, the surgeon will begin the removal process.
The surgeon will carefully locate and remove the sacral nerve stimulator device and its leads from your body. This process requires precision and expertise to minimize any potential damage to surrounding tissues or structures. If any repairs or closures are necessary, they will be performed during the same procedure.
The duration of the removal procedure can vary depending on individual factors, such as the complexity of the device and the patient’s anatomy. Your healthcare team will keep you informed throughout the process, ensuring that you are comfortable and well-informed.
Recovery and Aftercare
Following device removal, your healthcare provider will provide instructions for post-removal care and will likely monitor your progress to ensure proper healing. It is essential to follow any provided guidance and to address any concerns or complications promptly.
After the procedure, you will be taken to a recovery area where you will be closely monitored by the nursing staff. They will assess your vital signs, manage any pain or discomfort, and provide you with instructions on how to care for the incision site.
Your healthcare provider may prescribe pain medications or recommend over-the-counter pain relievers to manage any post-procedure discomfort. They will also provide guidance on when you can resume normal activities, such as bathing, exercising, and returning to work.
During the recovery period, it is important to attend any scheduled follow-up appointments with your healthcare provider. These visits allow them to monitor your progress, address any concerns, and make any necessary adjustments to your treatment plan.
If you experience any unusual symptoms, such as excessive bleeding, infection, or worsening pain, it is crucial to contact your healthcare provider immediately. They will be able to evaluate your condition and provide appropriate guidance or intervention.
Remember, every individual’s recovery process is unique, and it is essential to be patient with yourself as you heal. With proper care and support from your healthcare team, you can navigate the removal process of sacral nerve stimulators and work towards finding the most effective treatment plan for your specific needs.
Alternatives to Sacral Nerve Stimulation
Sacral nerve stimulator removal does not mean the end of treatment options. There are alternative approaches that may be explored based on individual circumstances and the underlying condition being treated.
When it comes to managing symptoms, medication management is one alternative that can be considered. In some cases, medications may be used as an alternative or adjunctive treatment. Anticholinergic drugs, for example, can help relax the bladder muscles and reduce urinary urgency. Alpha-blockers, on the other hand, can help relax the muscles in the prostate and bladder neck, improving urine flow. Botulinum toxin injections, commonly known as Botox, can also be used to temporarily paralyze the bladder muscles and reduce overactive bladder symptoms. It is crucial to work closely with your healthcare provider to determine the most appropriate medication regimen for your specific situation.
Physical therapy approaches can also be effective in managing certain bladder and bowel dysfunctions. Pelvic floor muscle exercises, also known as Kegel exercises, are commonly recommended to strengthen the muscles that support the bladder and control urine flow. Biofeedback, another physical therapy technique, uses sensors to provide visual or auditory feedback on muscle activity, helping individuals learn how to control their pelvic floor muscles. Bladder retraining, on the other hand, focuses on establishing a regular voiding schedule and gradually increasing the time between bathroom visits. These approaches aim to strengthen muscles, improve coordination, and promote healthy habits.
In some cases, surgical interventions may be recommended as an alternative to sacral nerve stimulation. Procedures such as bladder augmentation, also known as cystoplasty, involve increasing the size of the bladder to improve its storage capacity. Urinary diversion, on the other hand, reroutes urine from the bladder to a different exit point, such as a stoma, bypassing the need for normal bladder function. Sling surgery, commonly used to treat stress urinary incontinence, involves placing a supportive sling around the urethra to provide better control over urine flow. These surgical options can be considered based on the underlying condition and individual needs, and should be thoroughly discussed with a healthcare provider.
Making the Decision to Remove a Sacral Nerve Stimulator
When considering the removal of a sacral nerve stimulator, it is crucial to approach the decision-making process thoughtfully and in collaboration with a healthcare provider. Several factors should be taken into account:
Consulting with Your Healthcare Provider
Discuss your concerns, symptoms, and treatment goals with your healthcare provider. They can provide valuable insights based on their clinical expertise and may be able to recommend alternatives or adjustments to your current treatment plan.
During the consultation, your healthcare provider will take into consideration various factors such as your medical history, the duration of the sacral nerve stimulator implantation, and any previous complications or side effects you may have experienced. They will also assess your current symptoms and evaluate the effectiveness of the device in managing your condition.
It is important to have an open and honest conversation with your healthcare provider, expressing any doubts or reservations you may have about the removal process. They will be able to address your concerns and provide you with the necessary information to make an informed decision.
Weighing the Risks and Benefits
Consider the potential risks and benefits of both continuing with the sacral nerve stimulator and exploring alternative options. Factors such as device-related complications, lifestyle considerations, and individual treatment goals should be carefully evaluated.
One of the primary risks associated with the continued use of a sacral nerve stimulator is the potential for device-related complications. These complications can include infection, device migration, or malfunction. It is important to discuss these risks with your healthcare provider and understand the likelihood of experiencing them based on your specific circumstances.
On the other hand, exploring alternative treatment options may offer potential benefits. These alternatives could include medication management, physical therapy approaches, or surgical interventions. Your healthcare provider can provide you with information about these options and help you understand how they may be beneficial in managing your condition.
Considering Your Quality of Life
Your quality of life is a crucial aspect to consider when making the decision to remove a sacral nerve stimulator. Assess how the device has impacted your daily activities, relationships, and overall well-being. It is essential to prioritize your comfort and satisfaction when making decisions about your healthcare.
Reflect on how the sacral nerve stimulator has affected your ability to engage in physical activities, work, or hobbies. Consider any limitations or restrictions you may have experienced and how they have influenced your overall quality of life. Additionally, evaluate the impact on your emotional well-being and relationships with others.
Discuss these aspects with your healthcare provider, as they can provide guidance on how the removal of the sacral nerve stimulator may impact your quality of life. They can also help you explore alternative treatment options that may better align with your goals and preferences.
In conclusion, there are various reasons why a sacral nerve stimulator may need to be removed, such as infection risks, device malfunction, or changes in medical condition. The removal process involves careful preparation, the actual removal procedure, and post-removal care. Alternative treatment options, including medication management, physical therapy approaches, and surgical interventions, can be explored based on individual needs. When making the decision to remove a sacral nerve stimulator, it is essential to consult with a healthcare provider, weigh the risks and benefits, and consider your quality of life. Remember to always seek personalized medical advice from a healthcare professional to guide your specific situation.