What Nerve Exits the Sacral Plexus?
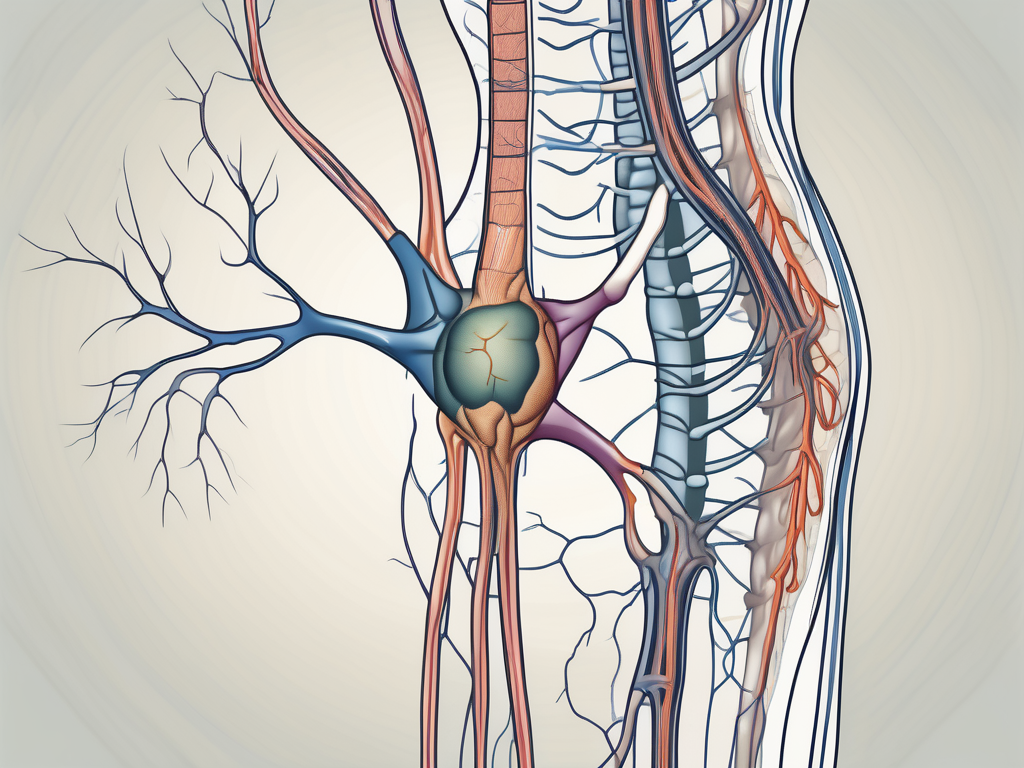
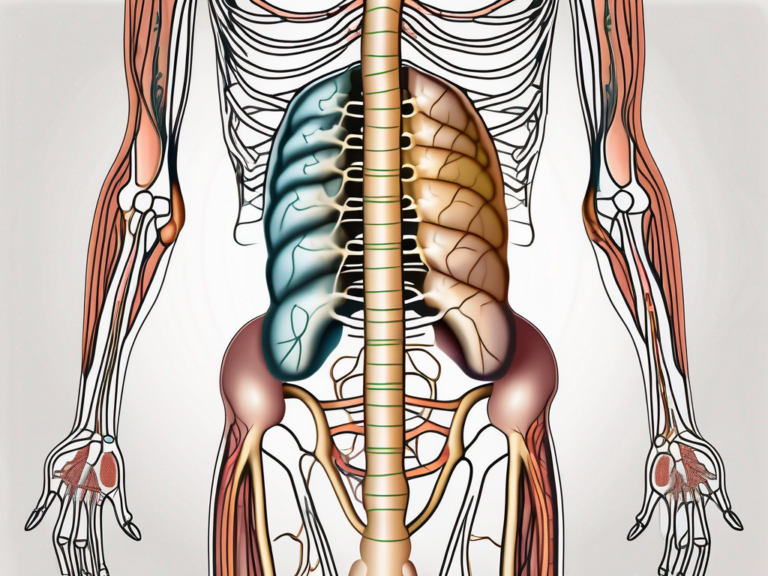
The sacral plexus is a complex network of nerve fibers located in the lower back region of the body. It is responsible for innervating the pelvic area, as well as the lower extremities. Understanding the sacral plexus and its associated nerves is crucial for comprehending the various functions and potential disorders of this intricate system.
Understanding the Sacral Plexus
The sacral plexus is formed by the fusion of the ventral rami of the fourth and fifth lumbar nerves, as well as the first, second, third, and fourth sacral nerves. This merging of nerve fibers results in the formation of several major nerves, each responsible for specific functions within the body. Two of the most vital nerves originating from the sacral plexus are the sciatic nerve and the pudendal nerve.
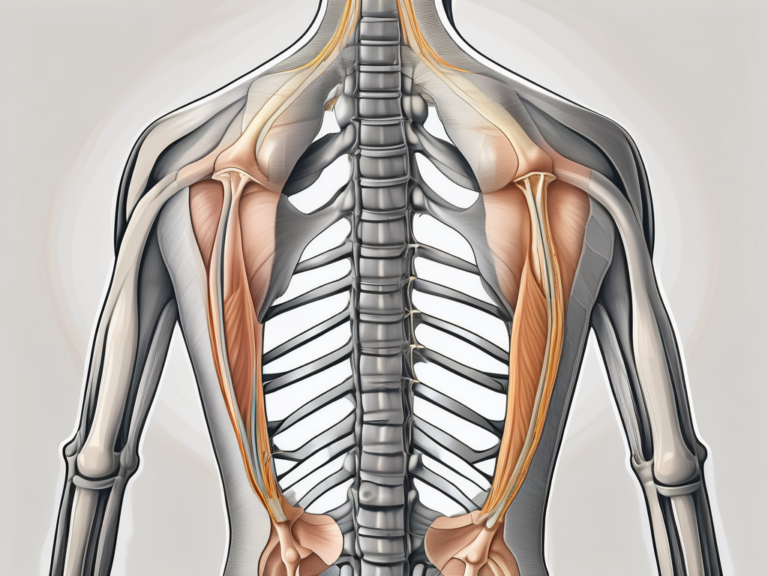
The sciatic nerve, originating from the sacral plexus, is the longest and thickest nerve in the human body. It extends from the lower back, through the buttocks, and down the back of each leg. The sciatic nerve provides motor and sensory innervation to the muscles of the thigh, leg, and foot, as well as sensation to the skin of the lower extremities. It plays a crucial role in enabling movements such as walking, running, and jumping.
The pudendal nerve, also arising from the sacral plexus, is responsible for innervating the perineum, which includes the external genitalia and the anal region. This nerve controls the muscles of the pelvic floor, allowing for voluntary control over urination, defecation, and sexual function. It also provides sensory perception to the genital area, contributing to sexual pleasure and arousal.
Anatomy of the Sacral Plexus
The sacral plexus lies in close proximity to the sacrum, a triangular bone situated at the base of the spine. It is a complex network of nerve fibers that courses through the pelvic region, branching out to provide innervation to various structures, including the muscles, skin, and organs in the lower extremities and pelvis.
Within the sacral plexus, the nerve fibers intertwine and form intricate connections, allowing for efficient communication between the central nervous system and the lower body. These connections ensure coordinated movements and sensory perception, enabling individuals to perform daily activities with ease.
As the nerve fibers extend from the sacral plexus, they divide into smaller branches that target specific regions of the lower limbs and pelvis. These branches include the superior gluteal nerve, inferior gluteal nerve, posterior femoral cutaneous nerve, and the perforating cutaneous nerve. Each of these branches has a unique role in providing motor and sensory innervation to specific muscles and areas of the lower body.
Functions of the Sacral Plexus
The sacral plexus plays a critical role in mobilizing the lower limbs and controlling bodily functions related to the pelvic region. It facilitates movements such as walking, running, and standing, while also overseeing essential functions like bowel and bladder control, sexual function, and sensory perception in the pelvic area.
Through its extensive network of nerves, the sacral plexus coordinates the contraction and relaxation of muscles in the lower limbs, allowing for smooth and coordinated movements. It ensures the proper functioning of the muscles involved in walking, maintaining balance, and performing various physical activities.
In addition to motor control, the sacral plexus also regulates important bodily functions related to the pelvic region. It controls the muscles responsible for bowel and bladder control, allowing individuals to voluntarily initiate and control the release of urine and feces. The sacral plexus also plays a crucial role in sexual function, providing innervation to the genitalia and facilitating sexual arousal and orgasm.
Furthermore, the sacral plexus contributes to sensory perception in the pelvic area. It enables individuals to perceive sensations such as touch, pressure, and temperature in the lower extremities and pelvic region, ensuring a comprehensive awareness of the surrounding environment.
In summary, the sacral plexus is a complex network of nerves that plays a vital role in the functioning of the lower limbs and the regulation of bodily functions in the pelvic region. Its intricate anatomy and diverse functions make it an essential component of the human nervous system, enabling individuals to perform daily activities and maintain overall well-being.
The Sciatic Nerve: The Main Nerve Exiting the Sacral Plexus
Among the major nerves originating from the sacral plexus, the sciatic nerve reigns supreme. This long and thick nerve travels down the back of the thigh, branching out to supply the muscles of the leg and foot.
The sciatic nerve, also known as the ischiadic nerve, is a vital component of the human body’s nervous system. It plays a crucial role in facilitating movement and transmitting sensory information from the lower extremities to the brain.
Anatomy of the Sciatic Nerve
The sciatic nerve is formed by the combination of nerve fibers from the fourth and fifth lumbar nerves and the first, second, and third sacral nerves. It is the largest nerve in the human body and is composed of two distinct components – the tibial nerve and the common fibular (peroneal) nerve.
The tibial nerve, a branch of the sciatic nerve, is responsible for innervating the posterior compartment of the leg and the sole of the foot. It controls important muscles such as the gastrocnemius, soleus, and tibialis posterior, which are essential for walking, running, and maintaining balance.
On the other hand, the common fibular nerve, another branch of the sciatic nerve, supplies the anterior and lateral compartments of the leg. It controls muscles like the tibialis anterior, extensor hallucis longus, and fibularis tertius, which are involved in dorsiflexion and eversion of the foot.
Functions of the Sciatic Nerve
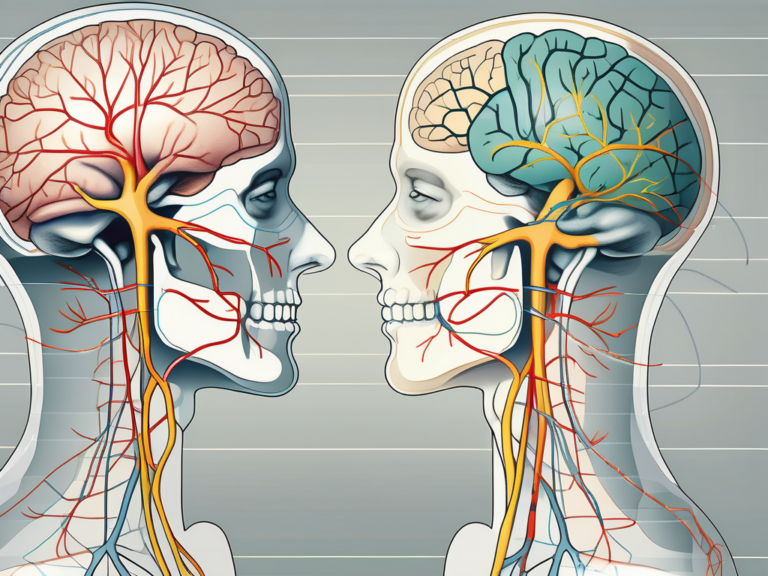
The sciatic nerve is responsible for providing both motor and sensory functions to the lower extremities. In addition to controlling the muscles of the leg and foot, it also conveys sensory information, enabling us to perceive sensations such as touch, pain, and temperature in the lower limbs.
Motor function-wise, the sciatic nerve allows for the flexion and extension of the knee joint, as well as the plantar flexion and dorsiflexion of the ankle joint. Without the sciatic nerve, these movements would be severely compromised, affecting our ability to walk, run, or even stand.
Furthermore, the sciatic nerve plays a crucial role in sensory perception. It carries sensory information from the skin, joints, and muscles of the lower extremities back to the brain, allowing us to feel sensations such as pressure, vibration, and temperature. This sensory feedback is essential for maintaining balance, avoiding injury, and responding to external stimuli.
In conclusion, the sciatic nerve is a remarkable structure that serves as the main nerve exiting the sacral plexus. Its intricate anatomy and multifaceted functions make it a vital component of the human body, enabling us to perform complex movements and perceive the world around us.
Other Nerves Associated with the Sacral Plexus
While the sciatic nerve takes center stage, there are additional nerves that arise from the sacral plexus and contribute to the overall function of the pelvic region.
Pudendal Nerve
The pudendal nerve originates from the sacral plexus and supplies the perineum, an area between the anus and the external genitalia. It plays a crucial role in controlling the muscles of the pelvic floor, including those responsible for bowel and bladder function, as well as sexual sensations.
Within the perineum, the pudendal nerve branches out to innervate various structures. It provides sensory innervation to the external genitalia, including the clitoris, labia, and penis. Additionally, it supplies the muscles of the perineum, such as the bulbospongiosus and ischiocavernosus muscles, which play a role in sexual function and maintaining erectile rigidity.
Furthermore, the pudendal nerve also contributes to the innervation of the anal sphincter muscles, aiding in the control of bowel movements. Dysfunction of the pudendal nerve can lead to conditions such as urinary and fecal incontinence, as well as sexual dysfunction.
Superior Gluteal Nerve
The superior gluteal nerve is also derived from the sacral plexus and supplies the gluteus medius, gluteus minimus, and tensor fascia lata muscles. These muscles are essential for maintaining stability and control of movements in the hip and pelvis region.
The gluteus medius and gluteus minimus muscles are responsible for abduction and rotation of the thigh, as well as maintaining balance while standing or walking. They play a crucial role in stabilizing the pelvis during activities such as running and climbing stairs.
The tensor fascia lata muscle, on the other hand, is involved in flexion, abduction, and internal rotation of the hip joint. It also helps to stabilize the knee joint during activities such as walking or running.
Damage or dysfunction of the superior gluteal nerve can result in weakness or paralysis of these muscles, leading to difficulties in walking, maintaining balance, and performing daily activities that require lower limb movement.
Common Disorders of the Sacral Plexus and Sciatic Nerve
As with any intricate system in the human body, the sacral plexus and its associated nerves are susceptible to certain disorders that can cause pain and dysfunction. Understanding these disorders is crucial in order to provide effective treatment and management. Two common issues affecting this region are sciatica and pudendal neuralgia.
Sciatica: Causes and Symptoms
Sciatica refers to pain that radiates along the path of the sciatic nerve, typically affecting one side of the body. The most common cause of sciatica is a herniated disc in the lumbar spine, which can compress the nerve roots that contribute to the sciatic nerve. However, there are other potential causes as well, such as spinal stenosis, spondylolisthesis, or even muscle imbalances that put pressure on the nerve.
The symptoms of sciatica can vary from person to person, but they often include pain, tingling, and numbness that can extend from the lower back through the buttocks and down the leg. The severity of the symptoms can also vary, ranging from mild discomfort to debilitating pain that affects daily activities and quality of life.
It is important to note that while sciatica is commonly associated with lower back pain, not all cases of lower back pain are caused by sciatica. Proper diagnosis by a healthcare professional is essential to determine the underlying cause and develop an appropriate treatment plan.
Pudendal Neuralgia: An Overview
Pudendal neuralgia is a condition characterized by chronic pain in the perineum, often aggravated by sitting or activities that put pressure on the area. The perineum is the region between the anus and the genitals, and the pudendal nerve is responsible for providing sensation to this area.
The exact cause of pudendal neuralgia can be challenging to determine, as it can result from various factors. It may be caused by direct injury or trauma to the nerve, such as during childbirth or prolonged sitting on hard surfaces. In some cases, it may be associated with pelvic floor dysfunction or compression of the nerve due to anatomical abnormalities.
Individuals with pudendal neuralgia may experience a range of symptoms, including pelvic pain, discomfort during intercourse, and urinary or bowel dysfunction. The pain can be sharp, burning, or throbbing, and it may radiate to the buttocks, thighs, or lower back. The intensity of the pain can vary, and it may worsen with certain activities or prolonged sitting.
Diagnosing pudendal neuralgia can be challenging, as the symptoms can overlap with other pelvic pain conditions. A comprehensive evaluation by a healthcare professional, including a thorough medical history, physical examination, and possibly imaging or nerve conduction studies, is necessary to reach an accurate diagnosis.
Once diagnosed, treatment for pudendal neuralgia may involve a multidisciplinary approach. This can include medications to manage pain, physical therapy to address muscle imbalances or pelvic floor dysfunction, nerve blocks to provide temporary relief, and in some cases, surgical interventions to decompress the nerve.
It is important for individuals experiencing symptoms related to the sacral plexus and sciatic nerve to seek medical attention for proper diagnosis and treatment. Early intervention can lead to better outcomes and improved quality of life for those affected by these disorders.
Treatment and Management of Sacral Plexus Disorders
If you suspect you may be experiencing pain or dysfunction related to the sacral plexus or its associated nerves, it is crucial to seek appropriate medical evaluation and guidance. The sacral plexus is a complex network of nerves located in the lower back and pelvis, responsible for innervating the lower extremities and pelvic organs. Disorders of the sacral plexus can cause a range of symptoms, including pain, weakness, numbness, and bladder or bowel dysfunction.
When it comes to the treatment of sacral plexus disorders, a multidisciplinary approach is often necessary to address the various aspects of the condition. Treatment options generally include both non-surgical and surgical interventions, depending on the underlying cause and severity of symptoms.
Non-Surgical Treatments for Sacral Plexus Disorders
Non-surgical treatment approaches may include physical therapy, medications to manage pain and inflammation, nerve blocks or injections, and lifestyle modifications. Physical therapy plays a crucial role in the management of sacral plexus disorders, as it focuses on strengthening the muscles surrounding the affected nerves, improving range of motion, and promoting overall functional recovery.
In addition to physical therapy, medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, and neuropathic pain medications may be prescribed to manage pain and inflammation associated with sacral plexus disorders. These medications work by reducing pain signals and improving overall comfort.
Nerve blocks or injections may also be utilized as a non-surgical treatment option for sacral plexus disorders. These procedures involve the targeted injection of medication, such as corticosteroids or local anesthetics, into the affected nerves or surrounding tissues. Nerve blocks can help alleviate pain and reduce inflammation, providing temporary relief for individuals with sacral plexus disorders.
Furthermore, lifestyle modifications can play a significant role in managing sacral plexus disorders. These modifications may include weight management, regular exercise, and ergonomic adjustments to minimize pressure on the affected nerves. Additionally, alternative therapies such as acupuncture or biofeedback may be considered to complement traditional treatment approaches.
Your healthcare provider will assess your specific condition and develop a comprehensive treatment plan tailored to your needs, which may involve a combination of different strategies. It is important to follow your healthcare provider’s recommendations and actively participate in your treatment plan to optimize outcomes.
Surgical Interventions for Sacral Plexus Disorders
In cases where conservative measures are not effective in relieving pain or restoring function, surgical intervention may be considered. Surgical procedures for sacral plexus disorders aim to address the underlying cause of nerve compression or damage, with the goal of alleviating symptoms and improving quality of life.
There are various surgical options available for sacral plexus disorders, depending on the specific condition and individual patient factors. These may include nerve decompression, nerve grafting, nerve transfer, or even spinal fusion in severe cases. The choice of surgical intervention will depend on factors such as the location and severity of nerve compression, the presence of scar tissue, and the overall health and goals of the patient.
It is important to consult with a qualified healthcare professional, such as a neurosurgeon or orthopedic surgeon specializing in spine disorders, to determine the most appropriate course of action. They will thoroughly evaluate your condition, review imaging studies, and discuss the potential risks and benefits of surgical intervention.
In conclusion, the treatment and management of sacral plexus disorders require a comprehensive approach that may involve both non-surgical and surgical interventions. Non-surgical treatments, such as physical therapy, medications, nerve blocks, and lifestyle modifications, aim to alleviate symptoms and improve overall function. Surgical interventions, on the other hand, target the underlying cause of nerve compression or damage to provide long-lasting relief. Working closely with a healthcare professional will ensure an individualized treatment plan that addresses your specific needs and goals.
Prevention and Maintenance of Sacral Plexus Health
While not all sacral plexus disorders can be prevented, certain lifestyle choices and habits can help maintain overall nerve health and minimize the risk of developing issues in this region.
Exercises for Sacral Plexus Health
Regular exercise, incorporating specific stretches and strengthening exercises targeting the lower back, hips, and pelvic region, can help improve flexibility, stability, and posture, reducing the likelihood of nerve impingement or compression. However, it is important to consult with a healthcare professional or a certified physical therapist before starting any new exercise regimen.
Lifestyle Changes to Support Sacral Plexus Health
Adopting a healthy lifestyle that includes maintaining a balanced diet, managing stress levels, practicing good posture, and avoiding prolonged periods of sitting can contribute to the overall well-being of the sacral plexus and its associated nerves. Remember to listen to your body and seek medical advice if you experience any persistent pain, numbness, or other unusual sensations in the lower back, hips, or pelvic region.
Conclusion
Understanding the complex network of nerves within the sacral plexus, particularly the sciatic nerve, is essential for comprehending the functions, disorders, and treatment options associated with this region. It is important to prioritize the health of the sacral plexus through exercise, lifestyle changes, and seeking appropriate medical assistance when necessary. By doing so, you can promote the optimal functioning of this intricate nerve network, ensuring a better quality of life and overall well-being.