How Long Does Sacral Nerve Stimulation Take?
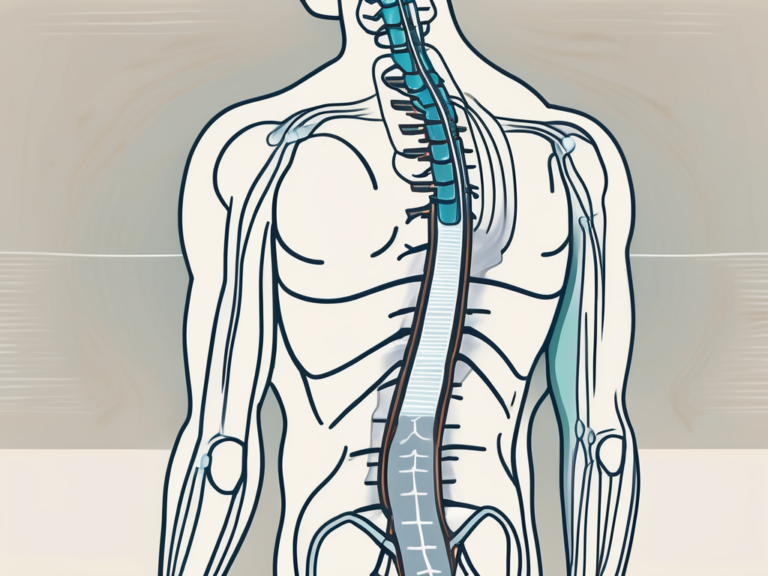
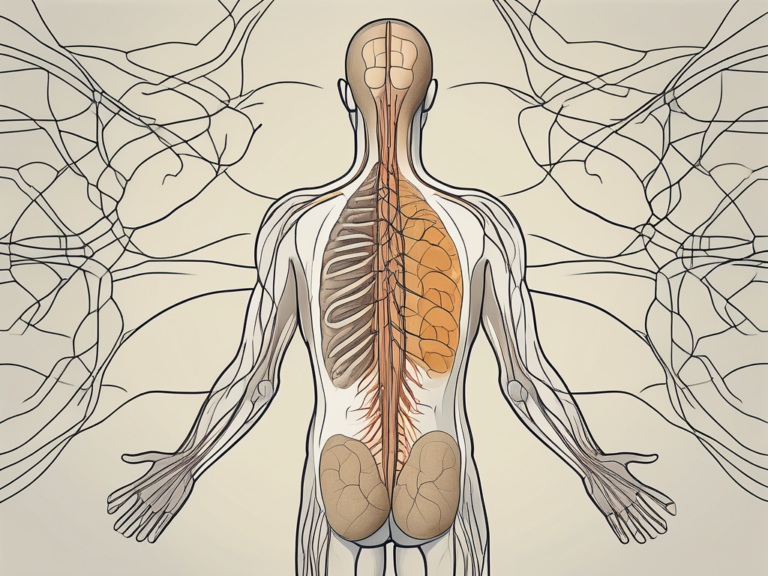
Sacral nerve stimulation is a medical procedure that aims to alleviate symptoms associated with various conditions such as overactive bladder, urinary and fecal incontinence, and chronic pelvic pain. It involves the use of a small device that delivers low-level electrical impulses to the sacral nerves, which are located near the lower back. This stimulation helps regulate the signals between the brain and the bladder or bowels, improving control and reducing symptoms.
Understanding Sacral Nerve Stimulation
Sacral nerve stimulation is a highly effective treatment option for individuals suffering from dysfunctional bladder or bowel control. This innovative approach aims to provide relief from the distressing symptoms that can significantly impact a person’s quality of life. When other conservative treatments have failed to provide adequate relief, sacral nerve stimulation offers hope and the possibility of a better life.
The Purpose of Sacral Nerve Stimulation
The main purpose of sacral nerve stimulation is to restore normal bladder and bowel function. This is achieved by modulating the nerve signals that control these bodily functions. By delivering precise electrical impulses to the sacral nerves, this treatment can effectively manage symptoms and improve the overall quality of life for individuals experiencing these conditions.
Imagine being able to regain control over your bladder and bowel, no longer living in fear of embarrassing accidents or constant discomfort. Sacral nerve stimulation offers this possibility, providing relief and restoring confidence to those who have been suffering for far too long.
The Process of Sacral Nerve Stimulation
Sacral nerve stimulation is typically performed in two stages, allowing for a thorough evaluation of its potential benefits before committing to a permanent implant.
The first stage involves a temporary trial period, during which a small wire called a lead is implanted near the sacral nerves. This temporary lead is connected to an external device that delivers electrical impulses. The patient is then encouraged to resume their normal activities and keep a diary to track changes in symptoms.
This trial period serves as a crucial step in determining the effectiveness of sacral nerve stimulation for each individual. It allows both the patient and the healthcare provider to assess the impact of the treatment on symptom improvement and overall well-being. It also provides an opportunity to fine-tune the settings of the electrical impulses to ensure optimal results.
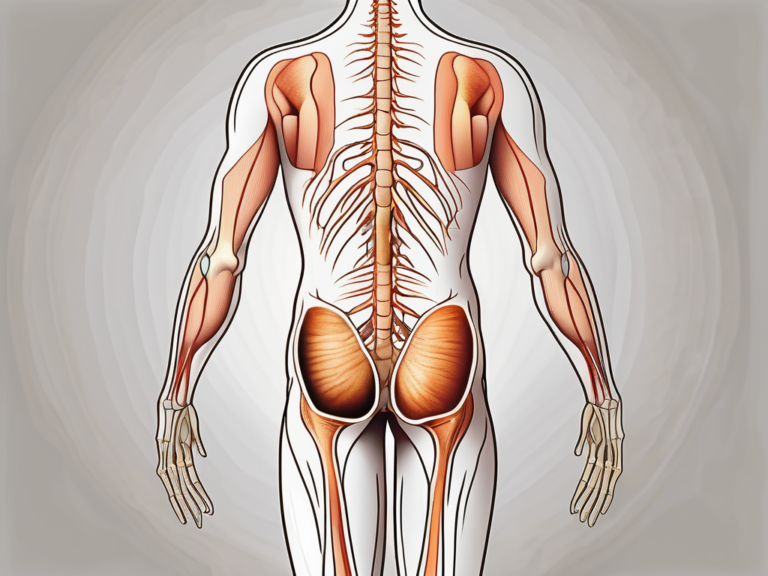
If the trial period is successful and significant symptom improvement is observed, the second stage of the procedure is pursued. This involves the placement of a permanent implant, also known as a neurostimulator.
The neurostimulator is surgically implanted under the skin, usually in the buttock area, and connected to the lead. This small device is programmable, allowing for adjustments to be made according to the patient’s specific needs. The programming can be done by the healthcare provider, ensuring that the treatment is tailored to each individual’s unique requirements.
Once the neurostimulator is in place, it works silently and discreetly, delivering electrical impulses to the sacral nerves. These impulses help regulate the bladder and bowel function, effectively managing symptoms and providing long-term relief.
It is important to note that sacral nerve stimulation is a well-established and safe procedure, with a high success rate and minimal risks. The benefits of this treatment extend beyond symptom relief, as many patients report an improvement in their overall quality of life, including increased confidence, social participation, and emotional well-being.
By understanding the process and purpose of sacral nerve stimulation, individuals can make informed decisions about their healthcare and explore this innovative treatment option with confidence. It is a remarkable advancement in medical science that has the potential to transform the lives of those suffering from bladder or bowel control issues.
Factors Influencing the Duration of Sacral Nerve Stimulation
Patient’s Health Condition
The duration of sacral nerve stimulation can vary depending on the patient’s health condition. Certain medical conditions or factors, such as obesity or the presence of other chronic illnesses, can affect the overall timeline of the procedure. It is important for patients to discuss their health history with their healthcare provider to ensure they have a clear understanding of how their specific circumstances may impact the duration of the treatment.
Obesity, for example, can pose challenges during the procedure. The excess weight may require additional time for positioning and securing the patient, as well as for accessing the sacral nerve area. Surgeons may need to take extra precautions to ensure the patient’s safety and optimize the effectiveness of the treatment.
In addition to obesity, the presence of other chronic illnesses can also impact the duration of sacral nerve stimulation. Patients with conditions such as diabetes or heart disease may require more time for pre-operative evaluations and monitoring during the procedure. This is done to ensure that their overall health is stable and that the risks associated with the treatment are minimized.
The Complexity of the Procedure
The complexity of the procedure can also influence the duration of sacral nerve stimulation. In some cases, additional steps or adjustments may be necessary to achieve optimal results. This can prolong the overall procedure time. Surgeons will evaluate each patient’s individual requirements to determine the most appropriate approach, which may involve additional steps or modifications to ensure the best possible outcome.
For instance, if the patient has previously undergone pelvic surgery or has anatomical variations, the surgeon may need to spend more time carefully navigating the pelvic area to access the sacral nerves. This requires precision and attention to detail to avoid any potential complications.
Furthermore, the complexity of the procedure may also be influenced by the specific condition being treated. Conditions such as urinary incontinence or fecal incontinence may require additional testing or evaluation during the procedure to accurately assess the functioning of the sacral nerves. This thorough evaluation ensures that the treatment plan is tailored to the patient’s needs and increases the chances of a successful outcome.
It is crucial for patients to have a comprehensive understanding of the factors that can influence the duration of sacral nerve stimulation. By discussing their health condition and concerns with their healthcare provider, patients can ensure that they are well-informed and prepared for the procedure. This open communication allows for personalized treatment planning and a smoother overall experience.
Preparing for Sacral Nerve Stimulation
Pre-procedure Check-ups and Tests
Prior to undergoing sacral nerve stimulation, patients will typically undergo various check-ups and tests to assess their overall health, identify any potential risks, and ensure the procedure is suitable for them. This pre-procedure evaluation is important not only to determine candidacy but also to provide healthcare professionals with valuable information to tailor the treatment plan to each patient’s needs.
During the pre-procedure check-ups, patients may undergo a series of tests, including blood tests, urine tests, and imaging studies. These tests help to evaluate the patient’s kidney function, liver function, and overall health status. Additionally, the healthcare provider may also assess the patient’s medical history, including any previous surgeries or medical conditions, to ensure the procedure is safe and appropriate.
Furthermore, patients may be required to undergo a physical examination to assess their current health status. This examination may include measuring vital signs such as blood pressure, heart rate, and temperature. The healthcare provider may also evaluate the patient’s general physical condition, including any signs of infection or inflammation that may affect the procedure’s outcome.
Mental and Physical Preparation
Mental and physical preparation are crucial before undergoing sacral nerve stimulation. Patients should consult with their healthcare provider to address any concerns or questions they may have regarding the procedure. Open communication with the healthcare team can help alleviate anxiety and ensure that the patient is well-informed about what to expect during the procedure and the recovery process.
In addition to addressing any mental concerns, patients should also focus on physical preparation. Maintaining a healthy lifestyle leading up to the procedure can contribute to a smoother recovery process. This includes following recommended dietary guidelines, such as consuming a balanced diet rich in nutrients and staying hydrated. Regular exercise, as advised by the healthcare provider, can also help improve overall physical fitness and promote better healing after the procedure.
Moreover, patients may be advised to refrain from certain medications or supplements in the days leading up to the procedure. This is to minimize the risk of complications and ensure the procedure’s success. It is important for patients to follow their healthcare provider’s instructions carefully and inform them of any medications or supplements they are currently taking.
Lastly, patients should make necessary arrangements for their post-procedure recovery. This may include arranging for transportation to and from the healthcare facility, as well as ensuring that they have a comfortable and supportive environment at home to aid in their recovery. It is important for patients to have a clear understanding of the post-procedure care instructions provided by their healthcare provider to promote optimal healing and minimize any potential complications.
The Procedure of Sacral Nerve Stimulation
Steps Involved in Sacral Nerve Stimulation
The procedure of sacral nerve stimulation involves several key steps. Firstly, the temporary lead is inserted near the sacral nerves during the trial period. This is typically done under local anesthesia, and patients are able to go home the same day. During this trial, healthcare providers closely monitor symptom improvements and patient feedback.
If the trial period is successful, the second stage involves the placement of the permanent neurostimulator implant. This is done under general anesthesia, and patients may need to stay in the hospital overnight for observation. The lead is attached to the neurostimulator, which is then implanted beneath the skin, usually in the upper buttock or lower back area.
After the procedure, healthcare professionals will program the neurostimulator to deliver the appropriate electrical impulses for each patient. This programming can be adjusted as needed during follow-up appointments to ensure optimal symptom control.
Sacral nerve stimulation is a minimally invasive procedure that offers hope to individuals suffering from a variety of conditions, including urinary and fecal incontinence, chronic pelvic pain, and overactive bladder. By targeting the sacral nerves, which play a crucial role in controlling bladder and bowel function, this treatment option aims to improve the quality of life for patients who have not responded to other conservative treatments.
During the trial period, patients may experience a range of sensations, including tingling, buzzing, or a mild pulsing feeling. These sensations are a result of the electrical impulses being delivered to the sacral nerves. It is important for patients to communicate any discomfort or concerns to their healthcare providers during this time.
The second stage of the procedure, involving the permanent neurostimulator implant, requires careful planning and precision. Surgeons must ensure that the lead is positioned correctly near the sacral nerves to achieve optimal results. The placement of the neurostimulator beneath the skin is done in a way that minimizes discomfort and maximizes the effectiveness of the treatment.
After the procedure, patients will have regular follow-up appointments to monitor their progress and make any necessary adjustments to the neurostimulator programming. These appointments provide an opportunity for healthcare professionals to address any concerns or questions that patients may have and to ensure that the treatment is providing the desired outcomes.
Time Taken for Each Step
The duration of each step in the sacral nerve stimulation process can vary. The temporary lead placement during the trial period usually takes around 30 minutes to an hour. The second stage, involving the permanent neurostimulator implant, typically takes about 1 to 2 hours. These time frames can differ based on individual patient needs and the complexity of each procedure.
It is important to note that the time taken for each step is just one aspect of the overall treatment process. The success of sacral nerve stimulation depends not only on the technical aspects of the procedure but also on the patient’s commitment to following post-operative instructions and actively participating in their own care. Adherence to a recommended post-operative care plan, including regular exercise, proper nutrition, and appropriate medication management, can greatly enhance the long-term effectiveness of the treatment.
Post-Procedure Expectations
Undergoing a medical procedure can be both a relief and a cause for concern. After the procedure, patients will need some time to recover and adjust to the changes in their body. The recovery time can vary depending on the individual and the specific procedure performed. Generally, it takes a few weeks for the body to heal and for the patient to regain their strength.
During this recovery period, it is essential to follow the instructions provided by the healthcare provider. These instructions may include guidelines for wound care, physical activity limitations, and any recommended lifestyle modifications. By adhering to these instructions, patients can ensure a successful recovery and minimize the risk of complications.
It is important to note that while improvement in symptoms may be observed shortly after the procedure, optimal results may take some time to materialize. The body needs time to adjust and heal, and the full benefits of the procedure may not be immediately apparent. Patients should communicate any concerns or questions they may have with their healthcare provider as they progress through the recovery process. Open and honest communication is crucial for both the patient and the healthcare provider to ensure the best possible outcome.
Follow-up Appointments and Check-ups
After the sacral nerve stimulation procedure, regular follow-up appointments and check-ups are necessary to monitor progress and ensure the neurostimulator is functioning correctly. These appointments provide an opportunity for the healthcare provider to assess the patient’s recovery and make any necessary adjustments to the treatment plan.
During these follow-up appointments, the healthcare provider will evaluate the patient’s overall well-being and the effectiveness of the neurostimulator. They may ask about any changes in symptoms, pain levels, or daily activities. This information helps the healthcare provider determine if any modifications to the electrical impulses delivered by the neurostimulator are needed to maximize the benefits of the treatment.
Attending and actively participating in these follow-up appointments is crucial for patients to achieve the best outcome. These appointments allow the healthcare provider to closely monitor the patient’s progress, address any concerns or questions, and provide ongoing support and guidance. By working together, the patient and the healthcare provider can ensure that the treatment is tailored to the patient’s specific needs and that any issues are promptly addressed.
It is normal to feel a mix of emotions during the recovery period and follow-up appointments. Patients may experience a range of feelings, including relief, anxiety, and hope. It is important to remember that healing takes time, and each individual’s journey is unique. By staying informed, following the healthcare provider’s instructions, and actively participating in the recovery process, patients can increase their chances of a successful outcome and a return to a fulfilling and healthy life.
Risks and Complications of Sacral Nerve Stimulation
Potential Short-term Complications
While sacral nerve stimulation is generally considered safe, as with any medical procedure, there are potential risks and complications. Some short-term complications can include infection, bleeding, and temporary discomfort or pain at the site of the implant. These risks are typically minimized by following proper post-operative care and guidelines provided by healthcare professionals.
Possible Long-term Risks
Long-term risks associated with sacral nerve stimulation are rare but can include device malfunction, discomfort, or the need for the device to be removed or replaced. It is important for patients to be aware of these risks and discuss them with their healthcare provider before undergoing the procedure. Regular follow-up appointments enable healthcare professionals to monitor and address any potential long-term issues.
Frequently Asked Questions about Sacral Nerve Stimulation
Can the Procedure be Expedited?
The duration of the sacral nerve stimulation procedure is based on various factors and individual patient needs. While it is natural to want expedited relief from symptoms, it is crucial to prioritize patient safety and optimize treatment outcomes. It is recommended to consult with a healthcare provider to determine the most appropriate and effective timeline for the procedure.
What if the Procedure Takes Longer than Expected?
If the sacral nerve stimulation procedure takes longer than initially expected, it could be due to various reasons such as anatomical complexities or unforeseen circumstances. In such cases, it is essential to trust the expertise of the medical team and allow them to perform the necessary steps to ensure the best possible outcome. Patients should remain in close communication with their healthcare provider to address any concerns or questions they may have along the way.
In conclusion, the duration of sacral nerve stimulation can vary depending on individual factors such as the patient’s health condition, the complexity of the procedure, and the recovery process. It is important for patients to consult with their healthcare provider to understand their specific circumstances and expectations. The ultimate goal of sacral nerve stimulation is to improve symptom control and enhance quality of life for individuals experiencing bladder or bowel control issues.