Why Sacral Nerve Stimulation Removal: Exploring the Procedure and Benefits
Sacral Nerve Stimulation Removal is a procedure that involves the removal of a sacral nerve stimulation device. In this article, we will delve into the different aspects of this procedure, including its understanding, reasons for removal, the removal process itself, post-procedure care and recovery, as well as the benefits and risks associated with it.
Understanding Sacral Nerve Stimulation
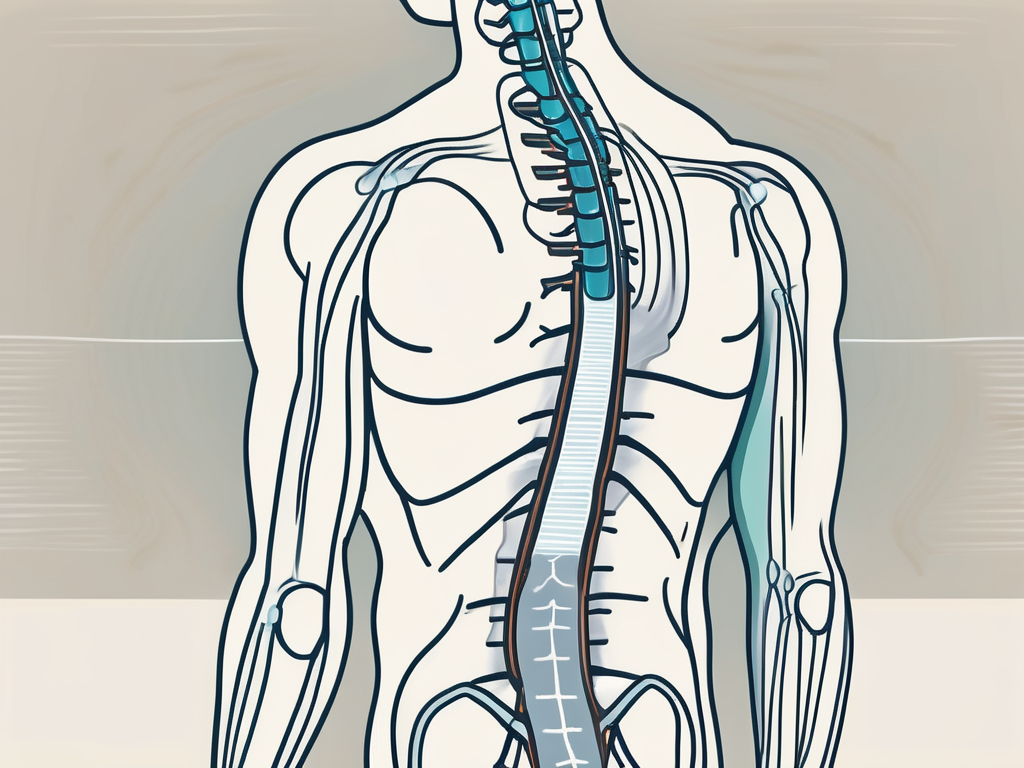
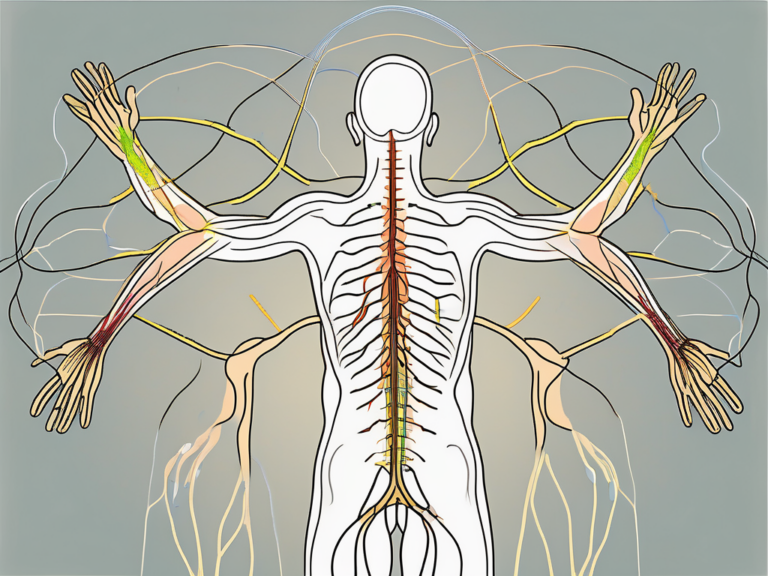
Sacral nerve stimulation (SNS) is a therapy that involves the use of a small device, similar to a pacemaker, to send mild electrical impulses to the sacral nerves. These nerves, located in the lower back, play a crucial role in controlling the bladder, bowel, and pelvic floor muscles. SNS therapy is primarily used to manage symptoms of certain urinary and bowel disorders, such as overactive bladder and fecal incontinence.
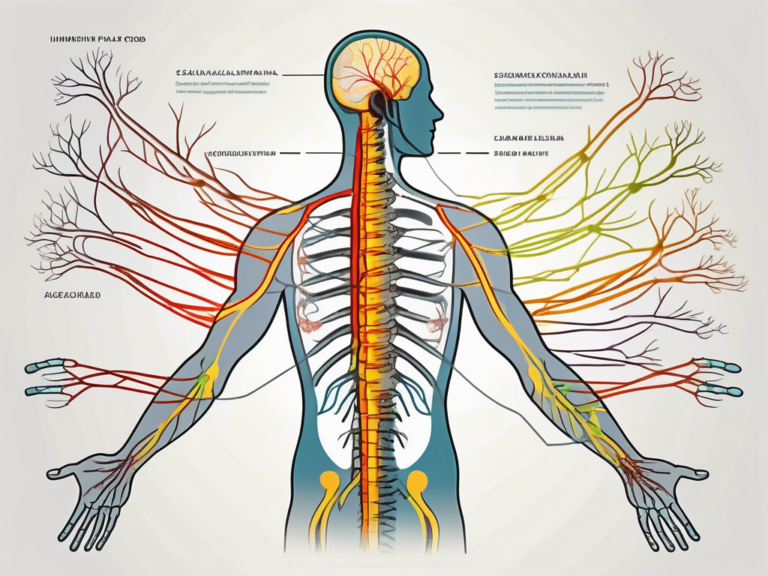
The Role of Sacral Nerve in the Body
The sacral nerve is responsible for transmitting signals between the brain and the muscles and organs in the pelvic region. It helps regulate bladder and bowel function, as well as sexual function. When the sacral nerve is not functioning optimally, it can result in various urinary and bowel problems.
For instance, a malfunctioning sacral nerve can lead to overactive bladder, a condition characterized by a sudden and uncontrollable urge to urinate. This can cause frequent trips to the bathroom, disrupting daily activities and impacting quality of life. Additionally, the sacral nerve plays a vital role in bowel control. When it is not functioning properly, fecal incontinence may occur, causing the involuntary leakage of stool.
Moreover, the sacral nerve is involved in sexual function. It helps coordinate the muscles involved in sexual activity and plays a role in achieving and maintaining an erection in men. Dysfunction of the sacral nerve can lead to sexual problems, such as erectile dysfunction or difficulty reaching orgasm.
The Basics of Sacral Nerve Stimulation Therapy
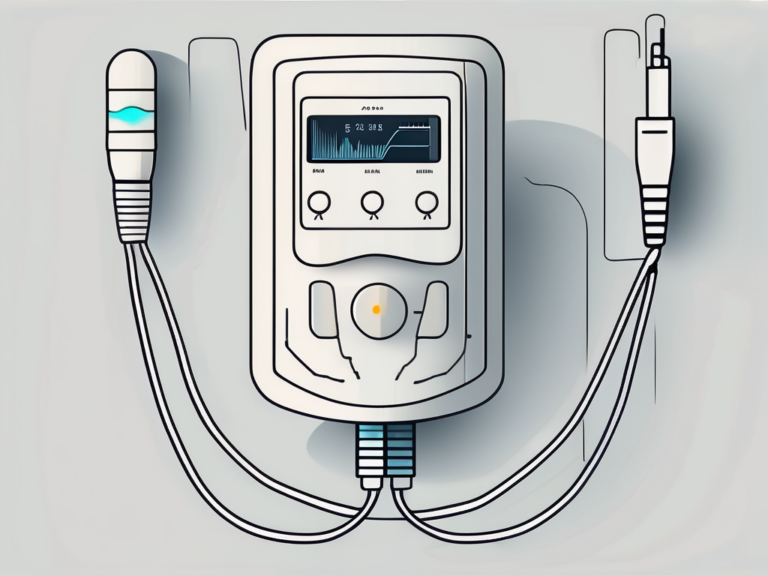
Sacral nerve stimulation therapy involves the implantation of a small device, often called a neurostimulator, under the skin typically in the buttock or lower abdomen. This neurostimulator sends electrical impulses to the sacral nerves, helping to restore normal function and alleviate symptoms associated with urinary and bowel disorders. Generally, SNS therapy is recommended when other conservative treatments have been unsuccessful.
During the SNS procedure, a thin wire, called a lead, is inserted near the sacral nerves. This lead is then connected to the neurostimulator, which is programmed to deliver electrical impulses at specific intervals and strengths. The electrical impulses generated by the neurostimulator modulate the activity of the sacral nerves, improving their function and reducing symptoms.
It is important to note that SNS therapy is reversible and adjustable. If the therapy does not provide the desired results or if side effects occur, the neurostimulator can be turned off or removed. Additionally, the strength and frequency of the electrical impulses can be adjusted to optimize the therapy’s effectiveness for each individual patient.
SNS therapy has been shown to be effective in managing symptoms of overactive bladder and fecal incontinence. Clinical studies have demonstrated significant improvements in urinary urgency, frequency, and incontinence episodes in patients receiving SNS therapy. Similarly, SNS therapy has been found to reduce episodes of fecal incontinence and improve bowel control.
Overall, sacral nerve stimulation is a promising therapy for individuals suffering from urinary and bowel disorders. By targeting the sacral nerves, SNS therapy aims to restore normal function and improve quality of life for patients experiencing these conditions.
Reasons for Sacral Nerve Stimulation Removal
While sacral nerve stimulation therapy can be highly effective for many individuals, there may be instances when removal of the device becomes necessary. These reasons can be categorized into medical indications for removal and patient-driven reasons for removal.
Medical Indications for Removal
There are specific medical indications that may require the removal of the sacral nerve stimulation device. One possible reason for removal is when the therapy is no longer providing the desired benefits. Over time, the body may develop a tolerance to the stimulation, resulting in a decrease in effectiveness. In such cases, the removal of the device may be recommended by a healthcare professional to explore alternative treatment options.
In addition, complications such as infection or erosion of the device can also necessitate its removal. Infections can occur when bacteria enter the body through the incision site or migrate from other areas. If left untreated, these infections can lead to serious health issues. Erosion of the device refers to the gradual wearing away of the materials used in its construction, which can cause discomfort and potential damage to surrounding tissues. In such situations, removal of the device is often necessary to prevent further complications and ensure the well-being of the patient.
It is crucial to consult with a doctor to assess the individual circumstances and determine the best course of action. The healthcare provider will consider the patient’s medical history, current symptoms, and the potential risks and benefits of removal before making a recommendation.
Patient-Driven Reasons for Removal
Patients may also choose to have the sacral nerve stimulation device removed for personal reasons. One common reason is a change in symptoms or lifestyle. As individuals progress through different stages of their lives, their symptoms and needs may evolve. What was once an effective treatment may no longer align with their current situation. For example, a patient who initially sought sacral nerve stimulation for urinary incontinence may find that their symptoms have improved over time, making the device unnecessary.
Another patient-driven reason for removal is a desire to explore alternative treatment options. While sacral nerve stimulation can be highly effective, it is not the only treatment available for certain conditions. Some individuals may wish to try different therapies or interventions to find the one that best suits their needs and preferences. In such cases, removal of the device allows for the exploration of alternative treatments under the guidance of a healthcare professional.
Lastly, some patients may simply have a personal preference to discontinue the therapy. They may find the device uncomfortable or inconvenient, or they may have personal reasons unrelated to their medical condition. It is essential for patients to engage in candid discussions with their healthcare provider to fully understand the implications of removal and explore alternative treatments that may suit their individual needs.
The Procedure of Sacral Nerve Stimulation Removal
The removal of a sacral nerve stimulation device is typically performed as a surgical procedure. This section will guide you through the pre-procedure preparations and the step-by-step process of the removal process itself.
Pre-Procedure Preparations
Prior to the removal procedure, your healthcare provider will conduct a thorough evaluation to ensure that removal is the appropriate course of action. This may involve a physical examination, review of medical history, and potentially additional tests or imaging studies. It is important to follow any specific instructions provided by your healthcare team, such as discontinuing certain medications or fasting before the procedure.
During the evaluation, your healthcare provider will discuss the reasons for removing the sacral nerve stimulation device. This may include factors such as the device no longer providing effective symptom relief, the development of complications, or the completion of a predetermined treatment duration. They will also explain the potential risks and benefits of the removal procedure, as well as any alternative treatment options available.
If you have any concerns or questions about the procedure, this is the time to address them with your healthcare provider. They will be able to provide you with the necessary information and reassurance to help you make an informed decision.
Step-by-Step Guide to the Removal Process
The removal process typically involves several steps. First, you will be placed under anesthesia to ensure a painless procedure. An anesthesiologist will carefully monitor your vital signs throughout the surgery to ensure your safety and comfort.
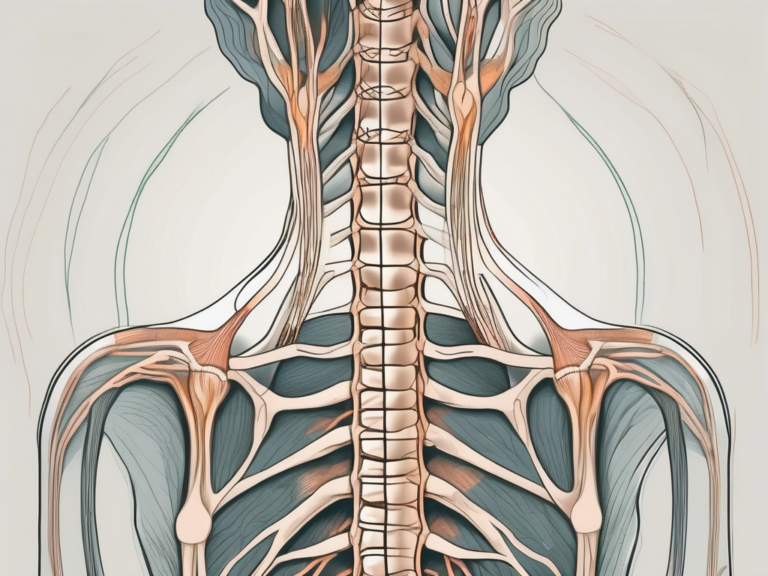
Once you are unconscious, the surgeon will make a small incision near the location of the implanted device. The incision site will be carefully chosen to minimize scarring and optimize access to the device. The surgeon will use sterile techniques to maintain a clean surgical field and reduce the risk of infection.
Using specialized surgical instruments, the surgeon will carefully dissect the tissue surrounding the device. This is done with precision and caution to avoid any damage to the surrounding nerves, blood vessels, or organs. The surgeon will then disconnect the device from any accompanying leads and gently remove it from the body.
After the device and leads have been removed, the surgeon will inspect the area to ensure that no fragments or debris remain. Any bleeding will be controlled, and the incision will be closed using either stitches or surgical adhesive. The choice of closure method will depend on factors such as the size and location of the incision, as well as the surgeon’s preference.
Finally, a sterile dressing will be applied to the incision site to protect it and promote proper healing. The dressing may need to be changed periodically in the days following the procedure, and your healthcare provider will provide you with instructions on how to care for the incision at home.
It is important to follow all post-operative instructions provided by your healthcare team, including any restrictions on physical activity, wound care, and medication usage. This will help ensure a smooth recovery and minimize the risk of complications.
Remember, every patient’s experience may vary, and it is essential to consult with your healthcare provider for personalized information and guidance regarding your specific situation.
Post-Procedure Care and Recovery
Following sacral nerve stimulation removal, proper care and recovery measures are essential to optimize healing and minimize discomfort. This section will discuss immediate aftercare and hospital stay, as well as long-term recovery and lifestyle adjustments.
After the procedure, you will likely be monitored in a recovery area until the anesthesia wears off and your vital signs stabilize. This is done to ensure your safety and well-being as you wake up from the effects of the anesthesia. Your healthcare team will be by your side, closely observing your condition and providing any necessary assistance.
Once you are fully awake and your vital signs are stable, your healthcare team will provide instructions for post-procedure care. These instructions may include information on discomfort management strategies and wound care procedures. It is important to follow these instructions carefully to promote proper healing and minimize the risk of complications.
In some cases, overnight hospital stays may be necessary for observation and further care. This is especially true if you have any underlying health conditions or if the procedure was particularly complex. Staying in the hospital allows your healthcare team to closely monitor your progress and provide any additional treatments or interventions that may be needed.
During the recovery period, it is important to follow your healthcare provider’s guidance regarding physical activity. Depending on your specific situation, you may be advised to limit certain activities or avoid them altogether for a certain period of time. This is to allow your body to heal properly and prevent any strain or injury to the surgical site.
In addition to physical activity, wound care is also an important aspect of post-procedure recovery. Your healthcare team will provide specific instructions on how to care for your wound, including how to clean it, dress it, and change the dressing. It is crucial to follow these instructions diligently to prevent infection and promote proper healing.
Some individuals may require physical therapy or additional support during their recovery phase. Physical therapy can help improve strength, flexibility, and mobility, and may be particularly beneficial if the sacral nerve stimulation removal was performed to address issues related to bladder or bowel control. Your healthcare team will determine if physical therapy is necessary and provide you with appropriate referrals and recommendations.
Additionally, adjustments to lifestyle, such as modifications to diet or exercise routines, may be necessary to optimize recovery and overall well-being. Your healthcare provider may recommend dietary changes to support healing and prevent constipation or other digestive issues. They may also provide guidance on gradually resuming exercise and physical activity, taking into consideration your specific needs and limitations.
Throughout the recovery process, it is important to attend any necessary follow-up appointments with your healthcare provider. These appointments allow your healthcare team to monitor your progress, address any concerns or complications, and make any necessary adjustments to your treatment plan. It is crucial to communicate openly and honestly with your healthcare provider during these appointments, as they rely on your feedback to ensure the best possible outcome.
The Benefits of Sacral Nerve Stimulation Removal
While sacral nerve stimulation therapy can provide significant relief for individuals with urinary and bowel disorders, there may be potential benefits associated with the removal of the device as well.
Potential Health Benefits
For some individuals, the removal of the sacral nerve stimulation device may result in a resolution or improvement of certain symptoms. This can be attributed to various factors such as the body’s natural healing process or the resolution of the underlying condition that necessitated the device in the first place. It is important to discuss any changes in symptoms with your healthcare provider to determine if removal is a suitable option.
Upon removal, some individuals may experience a decrease in urinary urgency, frequency, or incontinence. This can lead to a significant improvement in their overall bladder function and a reduction in related discomfort or embarrassment. In addition, removal may alleviate bowel dysfunction symptoms such as constipation or fecal incontinence, allowing individuals to regain control over their bowel movements and experience a greater sense of comfort and well-being.
Furthermore, the removal of the sacral nerve stimulation device can potentially reduce the risk of certain complications associated with long-term device usage. These complications may include infection, erosion, or discomfort at the site of the implanted device. By removing the device, individuals can minimize the likelihood of encountering such issues and promote their overall health and well-being.
Quality of Life Improvements
The decision to undergo sacral nerve stimulation removal may be driven by personal preferences or a desire for a different treatment approach. For those who opt for removal, it can result in improved quality of life, allowing individuals to explore alternative therapies or regain a sense of normalcy without relying on neurostimulation.
Without the presence of the sacral nerve stimulation device, individuals may have the opportunity to pursue other treatment options that were previously not feasible. This could include physical therapy, behavioral modifications, or medication adjustments. By exploring these alternatives, individuals can potentially find a treatment plan that better suits their needs and preferences, leading to enhanced overall well-being.
Moreover, the removal of the device can alleviate the burden of ongoing maintenance and potential complications associated with its use. This can reduce the need for frequent medical appointments, device adjustments, or troubleshooting, allowing individuals to focus on other aspects of their lives and potentially reducing stress levels associated with device management.
Additionally, some individuals may experience an improvement in their emotional well-being after the removal of the sacral nerve stimulation device. This can be attributed to a sense of freedom from the constant reminder of their condition and the associated limitations. It can also contribute to an increased sense of body confidence and self-esteem, as individuals regain control over their bodily functions without the aid of a device.
In conclusion, while sacral nerve stimulation therapy can be highly beneficial, the removal of the device may offer potential health benefits and improvements in quality of life. It is crucial to consult with healthcare professionals to assess individual circumstances and determine the most suitable course of action.
Risks and Considerations of Sacral Nerve Stimulation Removal
As with any medical procedure, sacral nerve stimulation removal carries certain risks and considerations that should be thoroughly understood before making a decision.
Possible Complications and How to Mitigate Them
Although uncommon, complications associated with sacral nerve stimulation removal can include infection, bleeding, or damage to surrounding tissues. To mitigate these risks, it is essential to choose an experienced surgeon and follow all pre-and post-procedure instructions provided by your healthcare team. Regular follow-up appointments will allow your doctor to monitor your progress and address any concerns.
Making an Informed Decision: Factors to Consider
When considering sacral nerve stimulation removal, it is crucial to engage in open and honest discussions with your healthcare provider. Factors to consider may include your overall health, the severity of symptoms, the potential benefits, alternatives, and any personal preferences or lifestyle considerations. Your healthcare team is best equipped to guide you through this decision-making process and provide the information necessary for an informed decision.
In conclusion, sacral nerve stimulation removal is a procedure that may be considered for various medical and patient-driven reasons. It involves a surgical process and necessitates proper care and recovery measures. While there may be potential benefits associated with its removal, it is essential to thoroughly understand the risks and considerations involved. Consultation with a healthcare provider is crucial for individualized assessment and guidance regarding sacral nerve stimulation removal.