Which Sacral Nerve Controls the Bladder?
The control and functioning of the bladder are vital aspects of our everyday lives. Many people are unaware of the intricate neural connections responsible for bladder control. Specifically, the sacral nerves play a significant role in regulating bladder function. Understanding the anatomy and function of the sacral nerves is crucial in comprehending the complexities of bladder control.
Understanding the Sacral Nerves
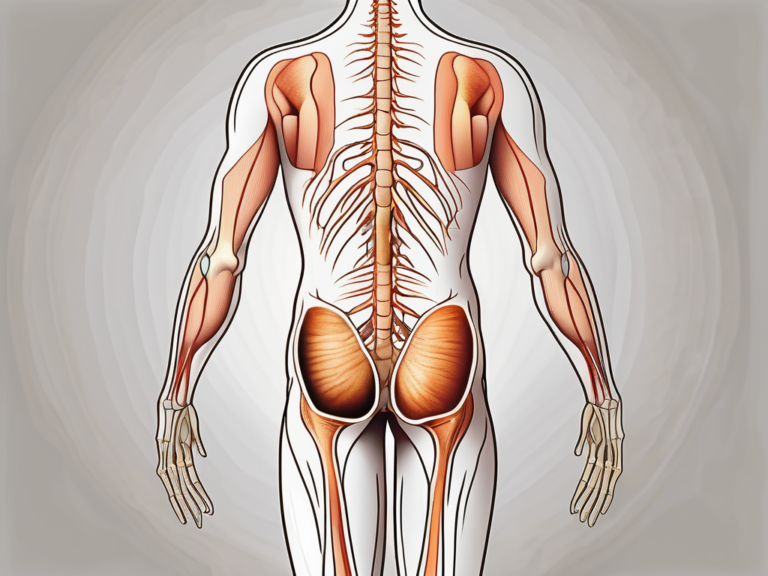
Anatomy of the Sacral Nerves
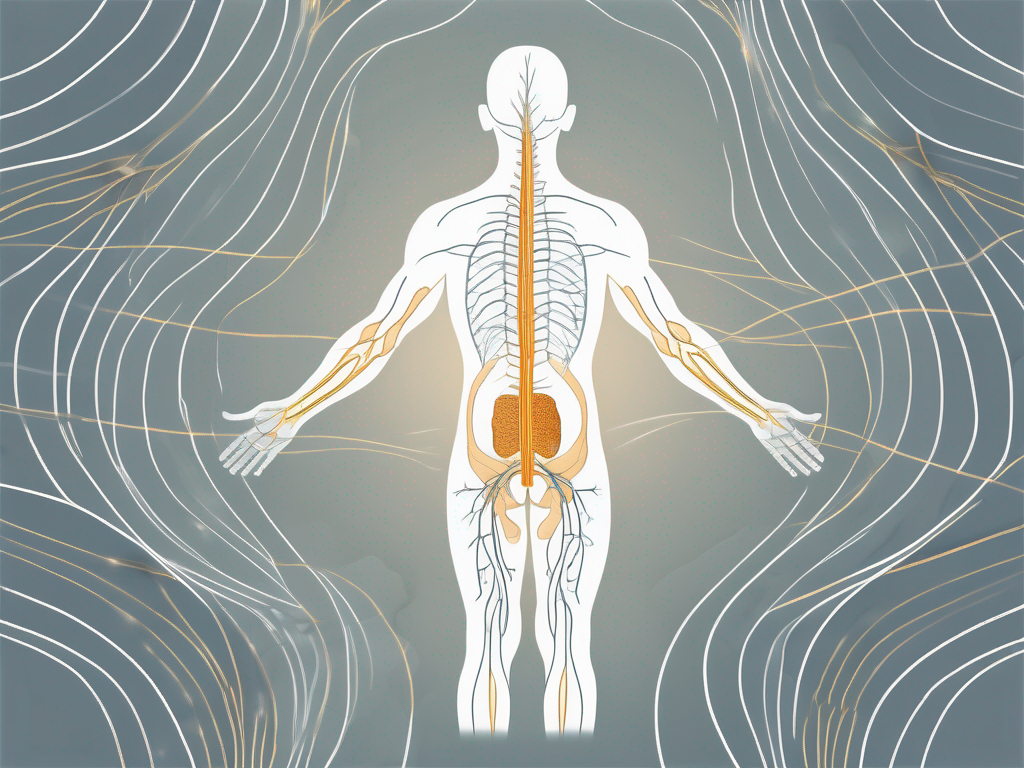
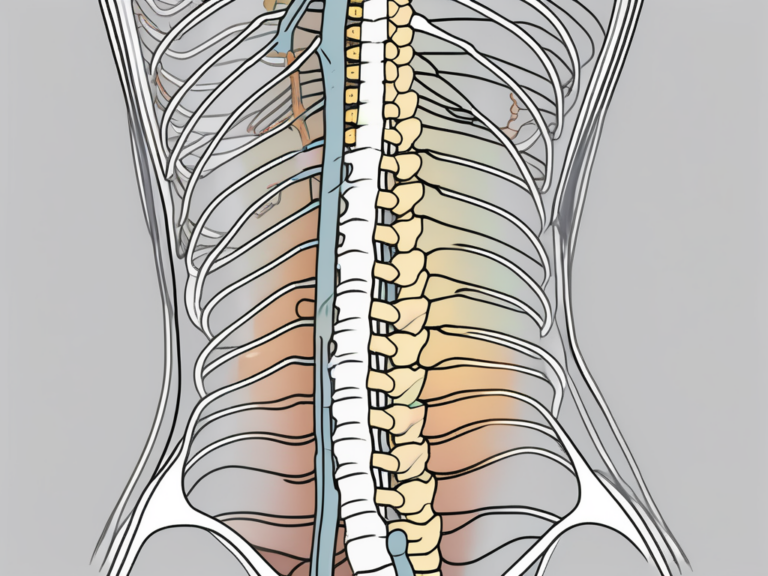
The sacral nerves are a set of nerves originating from the lower section of the spinal cord. They are part of the peripheral nervous system and play a vital role in transmitting signals between the bladder and the brain. The sacral nerves are specifically located in the sacral region of the spine, commonly referred to as the “S2-S4” region. These nerves are responsible for controlling various bodily functions, including bladder control.
The sacral nerves consist of a complex network of nerve fibers that branch out from the spinal cord. These fibers extend downwards, forming a bundle known as the sacral plexus. The sacral plexus is a crucial junction where the nerves from the spinal cord merge and divide, creating a network that connects to different parts of the body.
Within the sacral plexus, the sacral nerves receive sensory information from the bladder, rectum, and genitalia. This information is then transmitted to the brain, allowing us to perceive sensations such as fullness of the bladder or the need for a bowel movement.
Functions of the Sacral Nerves
In addition to controlling bladder function, the sacral nerves also influence other essential physiological processes. These include the regulation of bowel movements and the sexual response. The sacral nerves coordinate with the brain to ensure the correct timing and coordination of these functions. Any disruption in the sacral nerves’ normal functioning can result in bladder control issues.
When it comes to bowel movements, the sacral nerves play a crucial role in regulating the movement of the intestines. These nerves send signals to the muscles in the rectum, allowing for the coordinated contraction and relaxation necessary for proper bowel movements. Without the proper functioning of the sacral nerves, individuals may experience difficulties in emptying their bowels or suffer from constipation.
Furthermore, the sacral nerves are involved in the sexual response. They play a vital role in transmitting sensory information from the genitalia to the brain, allowing for sexual arousal and pleasure. The sacral nerves are responsible for the release of neurotransmitters that facilitate the relaxation of blood vessels in the genital area, leading to increased blood flow and the ability to achieve and maintain an erection in males.
In females, the sacral nerves are involved in the coordination of muscle contractions during orgasm. These contractions are necessary for the release of sexual tension and the overall pleasurable experience. Any disruption in the sacral nerves’ function can lead to sexual dysfunction, affecting both the physical and emotional well-being of individuals.
Overall, the sacral nerves are a crucial component of the peripheral nervous system, responsible for controlling various bodily functions. From bladder control to bowel movements and sexual response, these nerves play a vital role in maintaining our overall health and well-being. Understanding the anatomy and functions of the sacral nerves can help us appreciate the complexity of our bodies and the importance of proper nerve function.
The Nervous System and Bladder Control
The nervous system plays a significant role in controlling urination. It is a complex network of signals and pathways that allow for the coordination of bladder activity. When the bladder is full, sensory nerves in the bladder wall send signals to the brain, alerting it of the need to empty the bladder. This communication between the bladder and the brain is crucial for maintaining proper bladder control.
Role of the Nervous System in Urination
The process of urination involves a series of coordinated actions that are controlled by the nervous system. When the bladder is full, sensory nerves in the bladder wall detect the stretch and send signals to the brain. These signals travel along the spinal cord to the brain, where they are processed and interpreted. The brain then initiates a coordinated response by sending signals to the appropriate muscles, including those surrounding the bladder and the urethra, facilitating urine release.
It is fascinating to think about how the nervous system can accurately detect the level of bladder fullness and initiate the appropriate response. This intricate system ensures that we are aware of our body’s needs and can respond accordingly.
How Nerve Signals Control the Bladder
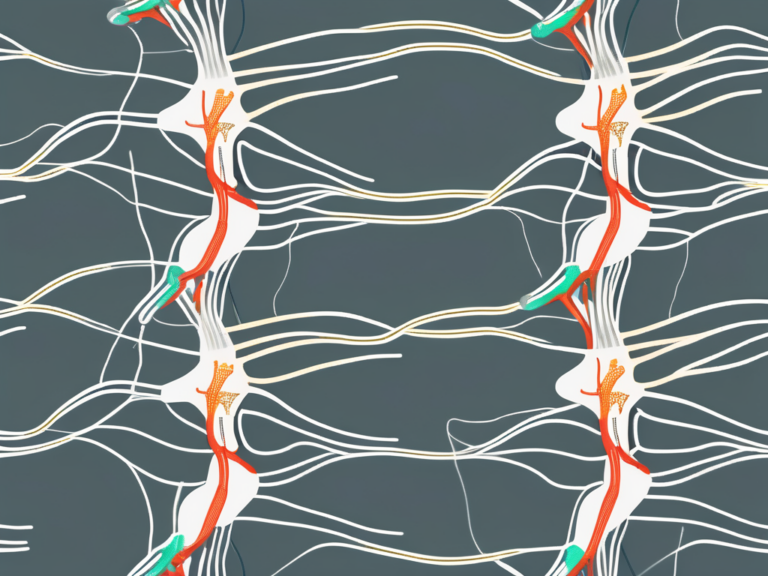
The nervous system uses a complex network of signals to regulate bladder activity. The sacral nerves, located at the base of the spine, play a crucial role in this process. These nerves transmit signals between the bladder muscles and the brain, allowing for the coordination of bladder contractions during urination.
When the brain receives the signals from the sacral nerves indicating that the bladder is full, it sends commands to the detrusor muscle, which is responsible for contracting and emptying the bladder. At the same time, the brain sends signals to the external sphincter muscles, which surround the urethra, instructing them to relax and allow urine to pass through.
This intricate dance of nerve signals ensures that the bladder contracts at the right time and the sphincter muscles relax appropriately, allowing for the smooth and efficient release of urine. Without this precise coordination, bladder control would be compromised, leading to problems such as urinary incontinence or retention.
Understanding how nerve signals control the bladder is not only fascinating but also essential for diagnosing and treating various bladder-related conditions. By studying the intricate mechanisms involved, researchers and healthcare professionals can develop targeted therapies to restore or improve bladder control in individuals with neurological disorders or other urinary dysfunctions.
The Sacral Nerves and the Bladder
Identifying the Specific Sacral Nerve
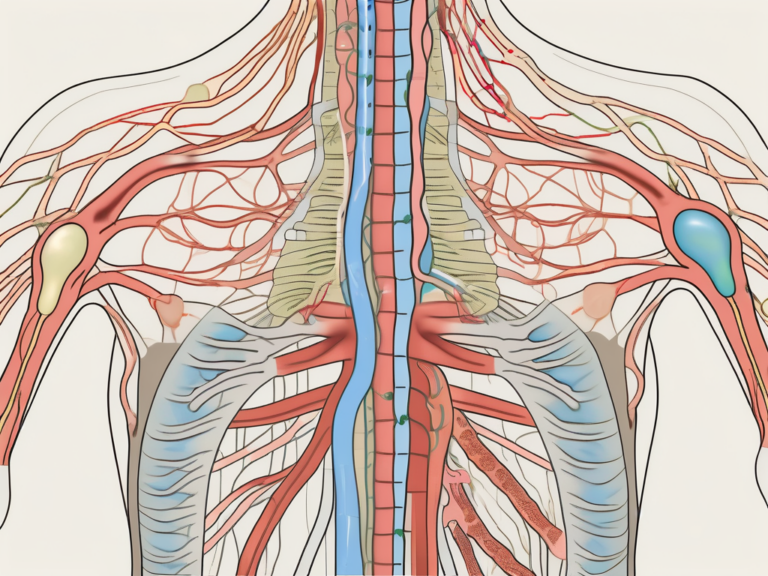
While the sacral nerves collectively contribute to bladder control, a specific sacral nerve, known as the pudendal nerve, plays a crucial role. The pudendal nerve, a branch of the sacral nerves, innervates the muscles around the urethra and facilitates voluntary control of urine flow. Any disruption or damage to this nerve can lead to urinary incontinence or difficulties in maintaining bladder control.
The pudendal nerve, originating from the sacral plexus, emerges from the sacral foramen and courses through the pelvis. It supplies motor fibers to the external urethral sphincter, which is responsible for maintaining continence by keeping the urethra closed. Additionally, the pudendal nerve provides sensory innervation to the perineum, including the external genitalia and the skin around the anus.
When the pudendal nerve is intact and functioning properly, it allows for the conscious control of urination. This means that an individual can voluntarily initiate or suppress the urge to urinate. The coordination between the pudendal nerve and the bladder muscles is essential for maintaining continence and preventing involuntary leakage.
How the Sacral Nerve Influences Bladder Function
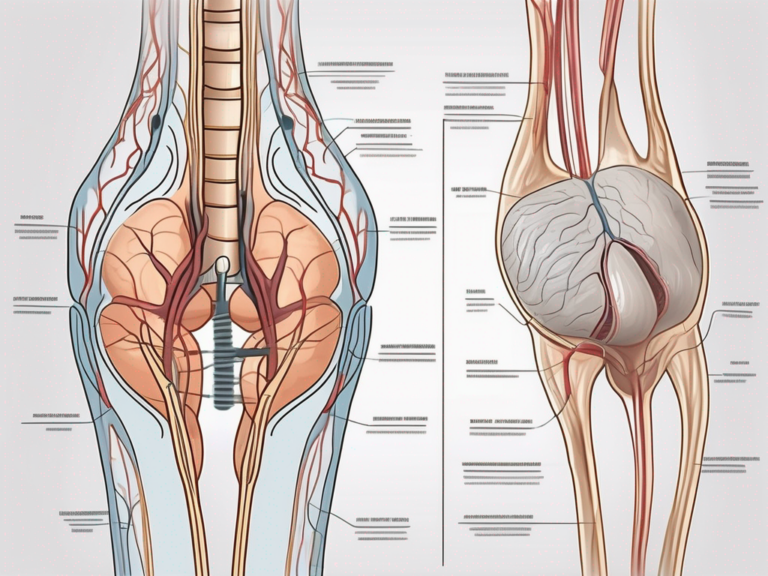
The sacral nerves communicate with the bladder muscles, allowing for coordinated contractions and relaxation necessary for proper urine storage and release. When the bladder is full, the sacral nerves signal the bladder muscles to contract, indicating the need for urination. This contraction is known as the detrusor muscle contraction. Simultaneously, the pudendal nerve sends signals to the external urethral sphincter, instructing it to relax and allow the passage of urine.
Conversely, when the bladder is empty, the sacral nerves help relax the bladder muscles, preventing involuntary leakage. The relaxation of the detrusor muscle allows the bladder to remain in a state of rest until it fills up again. At the same time, the pudendal nerve contracts the external urethral sphincter, maintaining its closure and preventing any accidental urine leakage.
It is important to note that the sacral nerves not only control bladder function but also play a role in other pelvic organs’ regulation, such as the rectum and sexual organs. The complex interplay between the sacral nerves, including the pudendal nerve, and these organs ensures proper functioning and coordination within the pelvic region.
In summary, the sacral nerves, with the pudendal nerve as a key player, are responsible for maintaining bladder control. Their communication with the bladder muscles allows for coordinated contractions and relaxation, ensuring proper urine storage and release. Any disruption or damage to these nerves can lead to urinary incontinence or difficulties in maintaining bladder control, highlighting the importance of understanding their role in bladder function.
Conditions Affecting the Sacral Nerves and Bladder Control
Neurological Disorders and Bladder Control
Various neurological disorders can affect the sacral nerves’ ability to control the bladder effectively. Conditions such as multiple sclerosis, spinal cord injuries, and stroke can disrupt the normal functioning of the sacral nerves, leading to bladder control problems. It is important for individuals with these conditions to consult with a healthcare professional to manage and address any bladder-related issues they may experience.
Multiple sclerosis (MS) is a chronic autoimmune disease that affects the central nervous system, including the brain and spinal cord. In MS, the immune system mistakenly attacks the protective covering of nerve fibers, causing communication problems between the brain and the rest of the body. As a result, the sacral nerves, responsible for bladder control, may not receive proper signals, leading to urinary incontinence or difficulty in emptying the bladder.
Spinal cord injuries can occur due to accidents, falls, or other traumatic events that damage the spinal cord. Depending on the severity and location of the injury, the sacral nerves may be affected, resulting in bladder control problems. The extent of the impairment can vary, ranging from mild urinary urgency to complete loss of bladder control. Rehabilitation and specialized medical care are crucial in managing bladder function after a spinal cord injury.
Stroke, also known as a cerebrovascular accident, happens when the blood supply to the brain is interrupted, either by a blood clot or a ruptured blood vessel. Depending on the area of the brain affected, stroke can disrupt the signals sent to the sacral nerves, leading to bladder control difficulties. In some cases, individuals may experience urinary retention, while others may have urinary incontinence. Rehabilitation and therapy are essential in helping stroke survivors regain bladder control and improve their quality of life.
Injury and Damage to the Sacral Nerves
Physical injury or damage to the sacral nerves can also result in bladder control difficulties. Trauma, accidents, or surgical procedures involving the sacral region may impact the nerves’ functioning, leading to urinary incontinence or other related problems. Seeking medical advice from a healthcare professional is critical in managing and treating such issues effectively.
Accidents, such as falls or car crashes, can cause direct trauma to the sacral nerves, resulting in immediate bladder control problems. The severity of the injury will determine the extent of the bladder dysfunction. In some cases, the nerves may be partially damaged, leading to intermittent bladder control issues, while in others, complete loss of bladder control may occur. Prompt medical attention and appropriate treatment can help individuals regain bladder function and minimize the impact on their daily lives.
Surgical procedures involving the sacral region, such as spinal surgeries or pelvic surgeries, carry the risk of damaging the sacral nerves. Surgeons take precautions to minimize nerve damage, but in some cases, it may still occur. Postoperative bladder control problems can range from temporary urinary retention to long-term urinary incontinence. Rehabilitation and specialized care are essential in managing and improving bladder function after surgery.
Treatment and Management for Sacral Nerve-Related Bladder Issues
Bladder issues related to sacral nerve damage can be challenging to manage, but with the right treatment and lifestyle changes, individuals can experience significant improvement in bladder control. Medical interventions and lifestyle modifications play a crucial role in addressing this condition.
Medical Interventions for Sacral Nerve Damage
When sacral nerve damage causes bladder control problems, various medical interventions can help manage the condition effectively. The treatment options depend on the severity and nature of the damage, and it is essential to consult with a healthcare professional to determine the most suitable treatment plan tailored to individual needs.
One common medical intervention for sacral nerve-related bladder issues is medication. Medications can help regulate bladder function and reduce symptoms such as urgency, frequency, and incontinence. Healthcare professionals may prescribe specific medications that target the sacral nerve pathways, helping to restore proper communication between the bladder and the brain.
In some cases, bladder retraining exercises may be recommended. Bladder retraining involves gradually increasing the time between bathroom visits to train the bladder to hold urine for longer periods. This technique can help improve bladder capacity and reduce the frequency of bathroom trips. A healthcare professional can provide guidance on the appropriate bladder retraining program based on individual needs.
For severe cases of sacral nerve damage, surgical options may be considered. Surgical interventions aim to repair or bypass the damaged nerves, restoring normal bladder function. These procedures are typically performed by urologists or neurosurgeons with expertise in treating sacral nerve-related bladder issues.
Lifestyle Changes and Bladder Control
In addition to medical interventions, certain lifestyle changes can contribute to improved bladder control for individuals with sacral nerve-related bladder issues. These changes focus on promoting overall bladder health and strengthening the muscles involved in bladder control.
Maintaining a healthy weight is crucial for bladder control. Excess weight can put additional pressure on the bladder, leading to increased urgency and leakage. By adopting a balanced diet and engaging in regular exercise, individuals can achieve and maintain a healthy weight, reducing the strain on the bladder and improving overall bladder function.
Practicing pelvic floor exercises, also known as Kegel exercises, can significantly strengthen the muscles responsible for bladder control. These exercises involve contracting and relaxing the pelvic floor muscles, which support the bladder and other pelvic organs. Regular practice of pelvic floor exercises can enhance muscle tone and improve bladder control.
Furthermore, individuals with sacral nerve-related bladder issues should avoid or limit the consumption of bladder irritants such as caffeine, alcohol, and spicy foods. These substances can irritate the bladder lining, leading to increased urgency and frequency of urination. By making conscious choices to reduce or eliminate these irritants from their diet, individuals can experience a noticeable improvement in bladder control.
Adopting healthy habits and implementing lifestyle changes, under the guidance of a healthcare professional, can significantly impact bladder control improvement. It is essential to work closely with a healthcare team to develop a comprehensive treatment plan that addresses both the medical and lifestyle aspects of managing sacral nerve-related bladder issues.
Future Research on Sacral Nerves and Bladder Control
Emerging Techniques in Neurology
Ongoing research in the field of neurology continues to explore innovative techniques and technologies to better understand and address bladder control issues related to the sacral nerves. Promising approaches, such as neuromodulation and nerve stimulation, show potential for improving bladder control and quality of life for individuals with sacral nerve-related bladder problems. However, it is essential to consult with healthcare professionals and stay informed about the latest advancements in this field.
Potential Breakthroughs in Bladder Control Treatment
Advancements in the understanding of sacral nerves and their role in bladder control provide hope for future breakthroughs in treatment options. Researchers are exploring new avenues, including gene therapy and regenerative medicine, that may revolutionize the management and treatment of bladder control issues. Stay informed about the latest scientific discoveries and inquire with healthcare professionals about potential options relevant to individual situations.
In conclusion, the sacral nerves play a crucial role in controlling bladder function. From the complex coordination of nerve signals to the specific influence of the pudendal nerve, understanding the intricate connections involved is key to addressing bladder control issues. If experiencing any bladder-related concerns, consulting with a healthcare professional is strongly recommended. With ongoing research and advancements, there remains hope for improved treatment options and a brighter future for those affected by sacral nerve-related bladder problems.