What Would Damage to the Sacral Nerve Plexus Cause?
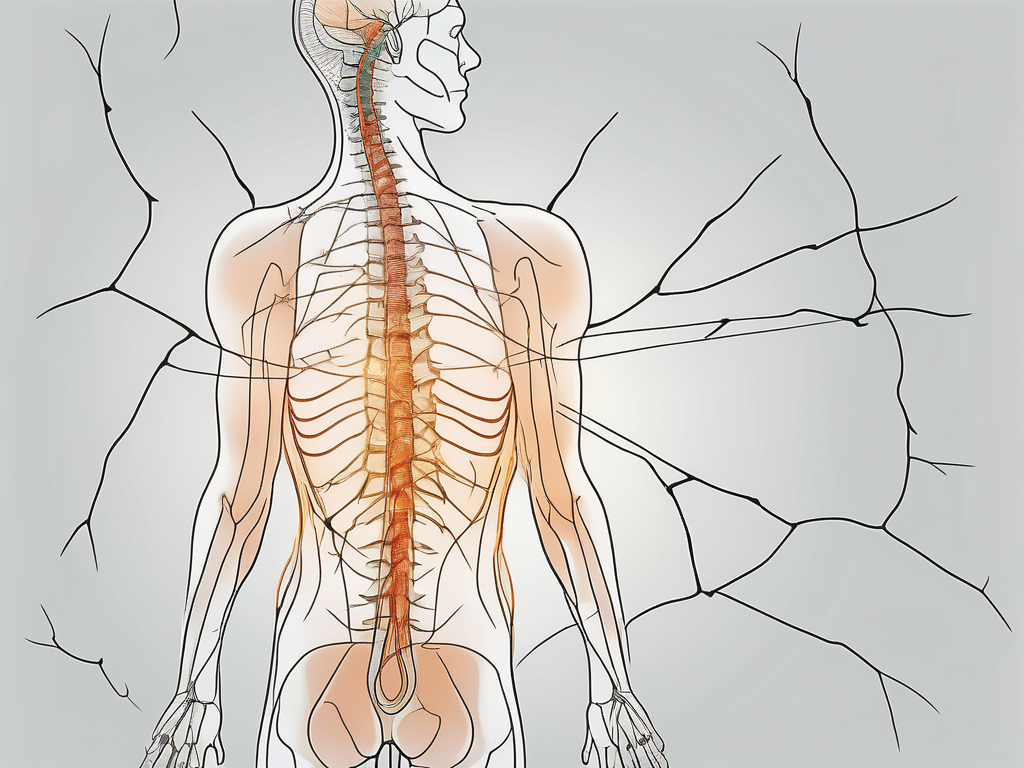
The sacral nerve plexus is a complex network of nerves that plays a crucial role in the functioning of the lower body. Comprised of a group of nerves originating from the sacral region of the spine, the sacral nerve plexus supplies motor and sensory signals to the pelvic area, lower extremities, and certain organs. Damage to the sacral nerve plexus can have a significant impact on a person’s quality of life, causing a range of symptoms and impairments.
Understanding the Sacral Nerve Plexus
Before delving into the consequences of sacral nerve plexus damage, it is essential to understand the anatomy and function of this intricate network. The sacral nerve plexus consists of five separate nerves: the sciatic nerve, the superior gluteal nerve, the inferior gluteal nerve, the posterior femoral cutaneous nerve, and the pudendal nerve.
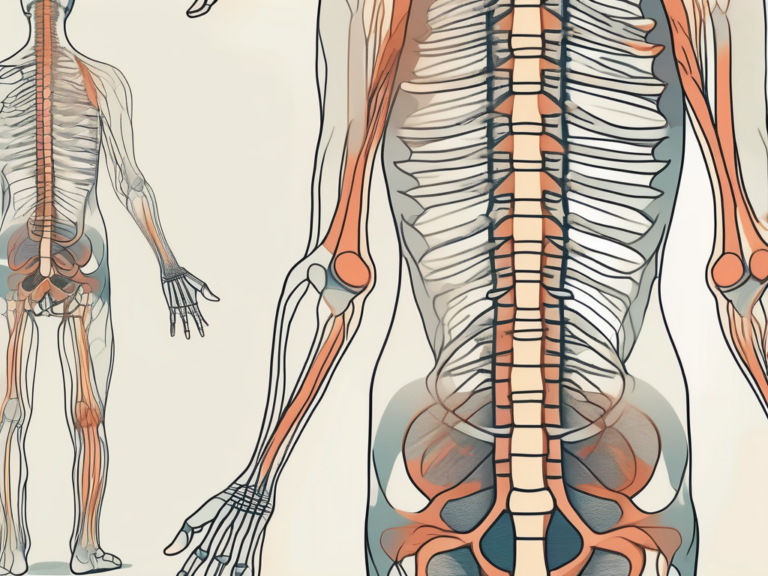
The sciatic nerve is the largest nerve in the body and is formed by the merging of the ventral rami of the fourth and fifth lumbar nerves and the first three sacral nerves. It runs from the lower back down the back of the thigh, branching out to provide motor control and sensation to the muscles of the thigh, leg, and foot.
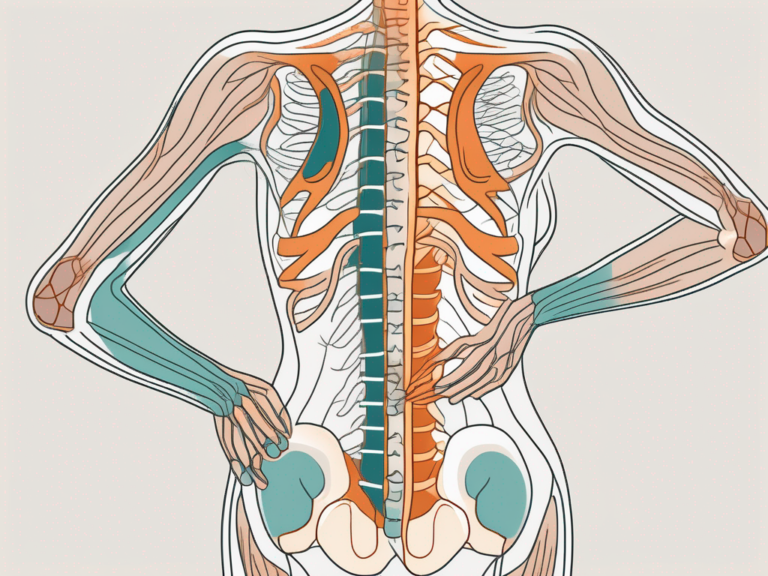
The superior gluteal nerve arises from the sacral plexus and innervates the gluteus medius, gluteus minimus, and tensor fasciae latae muscles. It is responsible for the abduction and medial rotation of the hip joint.
The inferior gluteal nerve also originates from the sacral plexus and supplies the gluteus maximus muscle, which is responsible for extending and laterally rotating the hip joint.
The posterior femoral cutaneous nerve is a sensory nerve that arises from the sacral plexus and provides sensation to the skin of the posterior thigh and the lower part of the buttocks.
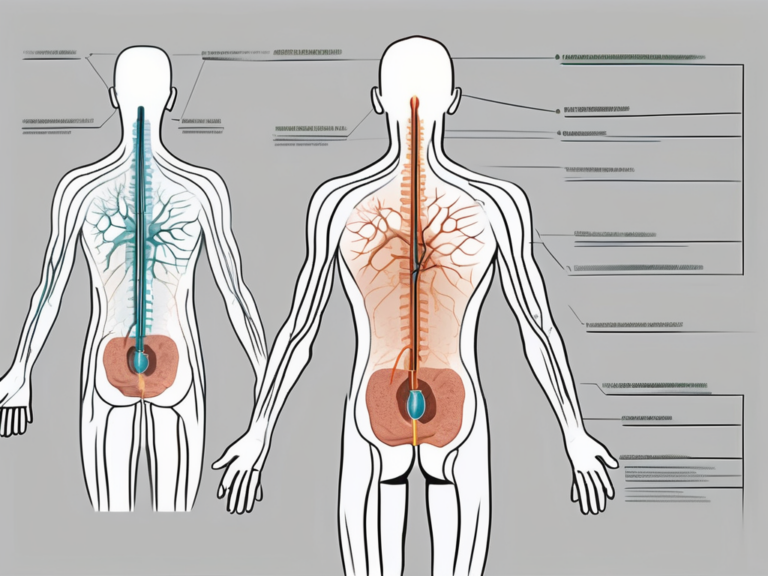
The pudendal nerve is another important nerve of the sacral plexus. It innervates the perineum, which includes the external genitalia and the muscles of the pelvic floor. The pudendal nerve plays a crucial role in controlling bowel and bladder function, as well as sexual function.
Anatomy of the Sacral Nerve Plexus
The sacral nerve plexus originates from the anterior rami of the spinal nerves L4 to S4. These nerves converge and form the sacral plexus, which lies in the posterior pelvic cavity, behind the piriformis muscle. The piriformis muscle is a small, pear-shaped muscle located deep in the buttock region. It plays a role in stabilizing the hip joint and rotating the thigh outward.
From the sacral plexus, the individual nerves branch out and travel along specific paths, innervating various muscles and tissues in the lower body. The sciatic nerve, for example, splits into two main branches: the tibial nerve and the common fibular (peroneal) nerve. The tibial nerve continues down the back of the leg, while the common fibular nerve wraps around the head of the fibula bone and divides into the superficial fibular nerve and the deep fibular nerve.
The tibial nerve supplies the muscles of the calf and the sole of the foot, while the common fibular nerve innervates the muscles of the anterior and lateral compartments of the leg. The superficial fibular nerve provides sensation to the skin on the top of the foot, while the deep fibular nerve supplies sensation to the skin between the first and second toes.
The superior gluteal nerve, inferior gluteal nerve, posterior femoral cutaneous nerve, and pudendal nerve also follow specific paths to reach their respective target muscles and tissues.
Function of the Sacral Nerve Plexus
The sacral nerve plexus is responsible for the motor control and sensation of the lower extremities, including the buttocks, hips, thighs, and legs. The sciatic nerve, being the largest nerve in the body, plays a significant role in this function by providing innervation to a wide range of muscles in the lower limb.
The superior gluteal nerve, inferior gluteal nerve, and posterior femoral cutaneous nerve contribute to the movement and sensation of the gluteal region and the back of the thigh. These nerves work together to ensure proper functioning and coordination of the muscles involved in walking, running, and other lower body movements.
The pudendal nerve, on the other hand, plays a crucial role in maintaining bowel and bladder function, as well as sexual function. It innervates the muscles of the pelvic floor, which are responsible for controlling urination, defecation, and sexual activity. Damage to the pudendal nerve can lead to various pelvic floor disorders, such as urinary and fecal incontinence, as well as sexual dysfunction.
Additionally, the sacral nerve plexus plays a vital role in maintaining balance and stability during movement. The muscles innervated by the nerves of the sacral plexus work together to provide stability to the hip joint, allowing for smooth and coordinated movement of the lower body.
In conclusion, the sacral nerve plexus is a complex network of nerves that plays a crucial role in the motor control and sensation of the lower extremities, as well as the function of the pelvic floor. Understanding the anatomy and function of this intricate network is essential in comprehending the consequences of sacral nerve plexus damage.
Causes of Sacral Nerve Plexus Damage
There are several potential causes of sacral nerve plexus damage, ranging from traumatic injuries to underlying medical conditions and diseases.
Trauma and Injuries
One common cause of sacral nerve plexus damage is trauma or injury to the pelvic region. The sacral nerve plexus, which is a network of nerves located in the lower back, can be affected by various accidents and incidents. For instance, car accidents can result in severe pelvic fractures, causing the nerves to become compressed or stretched. Falls, especially from significant heights, can also lead to trauma in the pelvic area, potentially damaging the sacral nerve plexus.
Sports-related accidents can also contribute to sacral nerve plexus damage. Athletes participating in contact sports like football or rugby are at a higher risk of experiencing injuries to the pelvic region. Impactful tackles or collisions can exert significant force on the nerves, leading to functional impairments. Additionally, childbirth complications can cause trauma to the sacral nerve plexus. The pressure exerted during labor and delivery can result in nerve compression or even nerve severance, affecting the functionality of the nerves.
Medical Conditions and Diseases
Certain medical conditions and diseases can contribute to sacral nerve plexus damage. Tumors, for example, can grow in the pelvic region and put pressure on the nerves. These tumors can be benign or malignant and may require surgical intervention to alleviate the compression on the sacral nerve plexus.
Infections can also play a role in sacral nerve plexus damage. Conditions such as pelvic inflammatory disease or sexually transmitted infections can cause inflammation in the pelvic region, leading to nerve irritation and potential damage. In some cases, prompt treatment of the underlying infection can help prevent long-term nerve damage.
Inflammation and degenerative disorders can also contribute to sacral nerve plexus damage. Conditions like disc herniation or spinal stenosis can cause the nerves to become compressed or pinched, resulting in pain, numbness, and weakness. These degenerative conditions often develop gradually over time, and early intervention is crucial to prevent further damage to the sacral nerve plexus.
Understanding the various causes of sacral nerve plexus damage is essential for accurate diagnosis and effective treatment. Whether it is trauma, medical conditions, or diseases, prompt medical attention and appropriate interventions can help alleviate symptoms and improve overall quality of life.
Symptoms of Sacral Nerve Plexus Damage
Signs and symptoms of sacral nerve plexus damage can vary depending on the location and severity of the nerve injury. They can manifest as physical symptoms and may even affect a person’s emotional and cognitive well-being.
The sacral nerve plexus is a complex network of nerves that originates from the lower spinal cord and innervates the pelvic region, including the buttocks, genitals, and lower limbs. When this network is damaged, it can lead to a range of symptoms that can significantly impact a person’s daily life.
Physical Symptoms
The physical symptoms of sacral nerve plexus damage can include pain, weakness, numbness or tingling, muscle atrophy, difficulty walking or maintaining balance, and issues with bowel or bladder control. These symptoms can vary in severity, depending on the extent of the nerve damage.
Pain is a common symptom experienced by individuals with sacral nerve plexus damage. It can range from a dull ache to sharp, shooting pains that radiate down the legs. This pain can significantly affect mobility and overall quality of life.
Weakness and muscle atrophy are also common physical symptoms. When the nerves in the sacral plexus are damaged, they may no longer be able to effectively transmit signals to the muscles in the pelvic region and lower limbs. This can result in muscle weakness and wasting, making it difficult to perform everyday tasks such as walking or standing for extended periods.
In addition to weakness, individuals with sacral nerve plexus damage may experience numbness or tingling sensations in the affected areas. This can lead to a loss of sensation and a decreased ability to detect pain or temperature changes.
Furthermore, damage to the sacral nerve plexus can affect bowel and bladder control. This can result in urinary or fecal incontinence, making it challenging to maintain personal hygiene and causing significant distress for the individual.
Some individuals may also experience sexual dysfunction as a result of sacral nerve plexus damage. The nerves in this region play a crucial role in sexual function, and any disruption can lead to difficulties with arousal, orgasm, or erectile dysfunction.
Emotional and Cognitive Symptoms
In addition to the physical impact, damage to the sacral nerve plexus can have emotional and cognitive consequences. Chronic pain, loss of independence, and physical limitations can contribute to depression, anxiety, frustration, and a diminished quality of life.
Living with chronic pain can be emotionally and mentally draining. It can lead to feelings of hopelessness, irritability, and a decreased ability to concentrate or engage in daily activities. The constant presence of pain can also disrupt sleep patterns, leading to fatigue and further exacerbating emotional distress.
Loss of independence is another significant emotional challenge faced by individuals with sacral nerve plexus damage. The inability to perform simple tasks independently, such as walking or using the bathroom, can lead to feelings of frustration, helplessness, and a loss of self-esteem.
Physical limitations resulting from sacral nerve plexus damage can also impact a person’s social life and relationships. The inability to participate in activities or hobbies they once enjoyed can lead to feelings of isolation and loneliness.
Furthermore, the emotional and cognitive impact of sacral nerve plexus damage can extend beyond the individual to their loved ones. Family members and caregivers may experience stress and emotional strain as they navigate the challenges of supporting someone with this condition.
In conclusion, sacral nerve plexus damage can have a wide range of physical, emotional, and cognitive symptoms. It is essential for individuals experiencing these symptoms to seek medical attention to receive an accurate diagnosis and appropriate treatment. With proper care and support, individuals with sacral nerve plexus damage can manage their symptoms and improve their overall quality of life.
Diagnosing Sacral Nerve Plexus Damage
Diagnosing sacral nerve plexus damage typically involves a comprehensive approach, including a medical history review, physical examination, and various imaging and laboratory tests.
The sacral nerve plexus is a complex network of nerves located in the lower back and pelvis. It plays a crucial role in the functioning of the lower limbs, pelvic organs, and lower abdominal muscles. When this nerve plexus is damaged, it can lead to a range of symptoms, including pain, weakness, numbness, and difficulty with mobility.
Medical History and Physical Examination
During the medical history review, the healthcare provider will ask about any symptoms, potential causes of injury, and previous medical conditions. This information helps to establish a baseline understanding of the patient’s overall health and identify any potential risk factors for sacral nerve plexus damage.
The physical examination will focus on assessing strength, reflexes, sensation, and mobility in the affected areas. The healthcare provider may perform specific tests, such as checking the patient’s ability to walk, stand on tiptoes, or perform certain movements that involve the lower limbs. These tests help to evaluate the extent of the damage and determine the specific nerves that may be affected.
Imaging and Laboratory Tests
To further evaluate the extent of the damage, imaging tests such as magnetic resonance imaging (MRI), computed tomography (CT) scan, or electromyography (EMG) may be ordered. These tests provide detailed information about the nerves, muscles, and surrounding tissues, helping to identify any abnormalities or areas of concern.
An MRI uses powerful magnets and radio waves to create detailed images of the internal structures of the body. It can help visualize the sacral nerve plexus and identify any signs of compression, inflammation, or structural abnormalities.
A CT scan, on the other hand, uses a series of X-ray images taken from different angles to create cross-sectional images of the body. This imaging technique can provide valuable information about the bones, muscles, and other tissues surrounding the sacral nerve plexus.
Electromyography (EMG) is a diagnostic test that measures the electrical activity of muscles and the nerves controlling them. It involves the insertion of small, thin needles into the muscles to record the electrical signals. This test can help determine the extent of nerve damage and differentiate between nerve and muscle disorders.
In addition to imaging tests, laboratory tests may also be conducted to rule out other possible causes of symptoms, such as infections or metabolic disorders. These tests may include blood tests, urine tests, or cerebrospinal fluid analysis, depending on the suspected underlying cause.
Overall, the diagnosis of sacral nerve plexus damage requires a thorough evaluation of the patient’s medical history, a comprehensive physical examination, and the use of various imaging and laboratory tests. This multidisciplinary approach helps healthcare providers accurately assess the extent of the damage and develop an appropriate treatment plan tailored to the individual patient’s needs.
Treatment Options for Sacral Nerve Plexus Damage
The treatment approach for sacral nerve plexus damage depends on various factors, including the severity of the injury, underlying causes, and individual circumstances.
Non-Surgical Treatments
In less severe cases, non-surgical interventions may be recommended. These can include physical therapy, medication management for pain and inflammation, assistive devices to aid mobility, and lifestyle modifications. It is crucial for individuals to follow their healthcare provider’s recommendations and regularly attend therapy sessions to maximize their recovery potential.
Surgical Treatments
In more severe cases, surgical intervention may be necessary to repair or restore damaged nerves or address any compressions or obstructions affecting the sacral nerve plexus. Surgical options can vary depending on the specific condition and may involve nerve grafting, decompressive procedures, or tumor removal, among others.
Prognosis and Recovery from Sacral Nerve Plexus Damage
The outlook for individuals with sacral nerve plexus damage depends on multiple factors, and the recovery process can differ significantly from person to person.
Factors Influencing Recovery
Factors that may influence the recovery process include the severity of the damage, the individual’s overall health and age, their adherence to treatment and rehabilitation plans, and the underlying cause of the injury. It is crucial for individuals to maintain realistic expectations and actively participate in their recovery journey.
Coping and Rehabilitation Strategies
The emotional and physical challenges associated with sacral nerve plexus damage can be overwhelming. It is essential to seek support from healthcare professionals, counselors, or support groups to address any mental health concerns, learn coping strategies, and adapt to the changes in daily life. Rehabilitation programs, including physical and occupational therapy, can also play a vital role in maximizing functional recovery and enhancing overall well-being.
Ultimately, damage to the sacral nerve plexus can significantly impact an individual’s life, causing a range of physical and emotional symptoms. Seeking timely medical evaluation and appropriate treatment is crucial to address the underlying causes and manage the consequences effectively. If you suspect that you may have sacral nerve plexus damage, it is essential to consult with a healthcare professional or neurologist for a proper diagnosis and personalized treatment plan.