What Is the Largest Nerve of the Sacral Plexus?
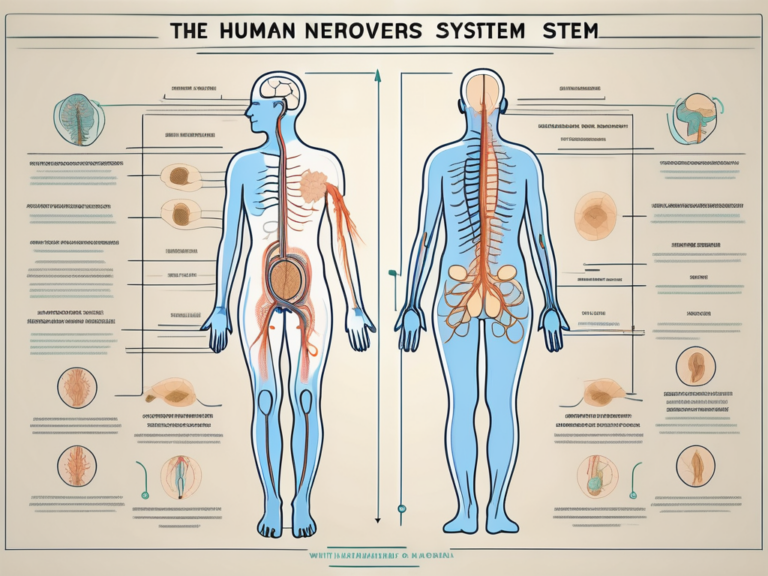
The largest nerve of the sacral plexus is the sciatic nerve. Understanding the sacral plexus and its intricate anatomy is crucial in comprehending the significance of the sciatic nerve and the conditions that can affect it.
Understanding the Sacral Plexus
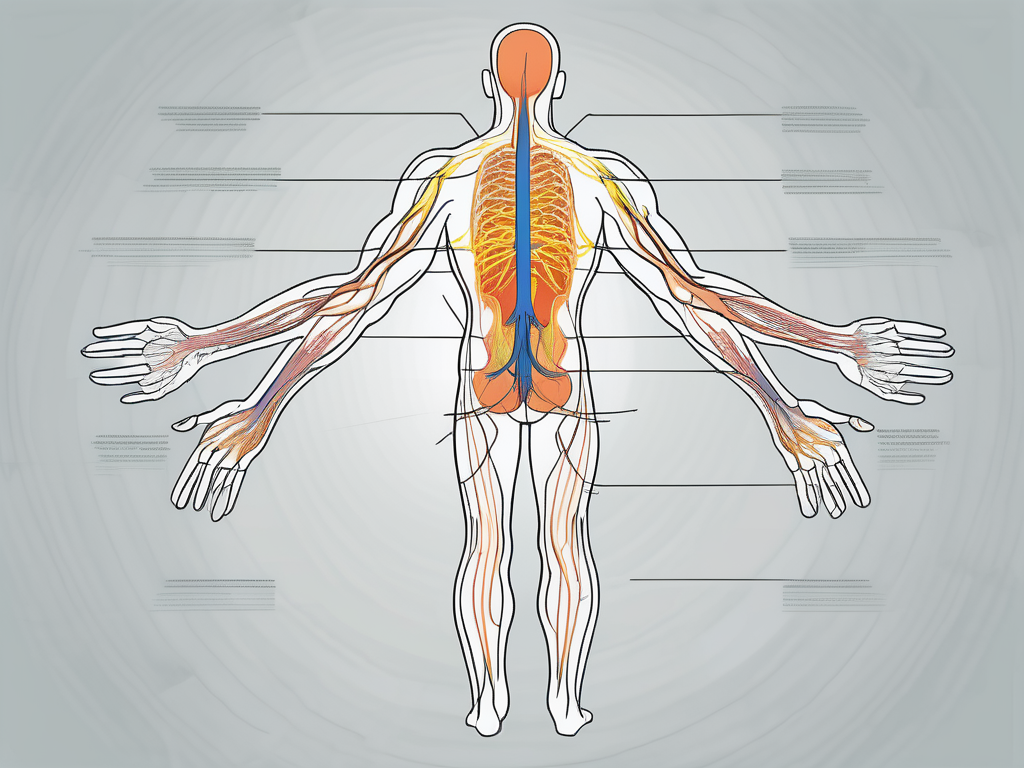
The sacral plexus is a complex network of nerves located in the pelvic region. It arises from the spinal nerves in the lower back, specifically from the fourth and fifth lumbar vertebrae and the first four sacral vertebrae. The plexus then gives rise to various nerves that supply the lower limbs and pelvic region.
The sacral plexus is an intricate structure that plays a vital role in the functioning of the lower limbs and pelvis. Let’s delve deeper into its anatomy and function to gain a comprehensive understanding.
Anatomy of the Sacral Plexus
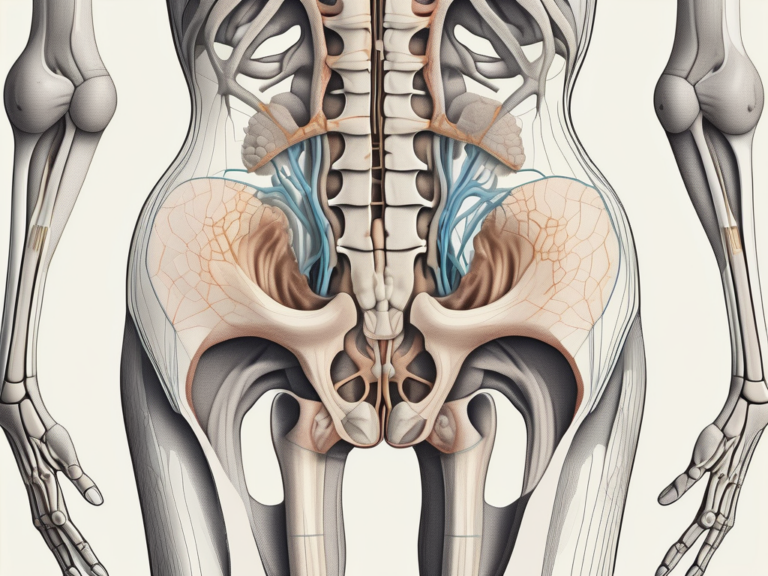
The sacral plexus is formed by the merging of multiple nerve roots, namely the anterior rami of the spinal nerves. This merging occurs within the pelvis, just below the lumbar plexus. The sacral plexus is a complex web of nerves that intertwines and interconnects, forming a network that extends its reach to various regions of the lower body.
As the sacral plexus takes shape, it gives rise to the major nerves that innervate the lower limbs, including the sciatic nerve. The sciatic nerve, one of the largest nerves in the body, originates from the sacral plexus and extends down the back of the thigh, branching out to provide sensation and motor control to the leg and foot.
Moreover, the sacral plexus also gives rise to other important nerves, such as the pudendal nerve, which supplies sensation to the external genitalia, perineum, and anus, and the superior and inferior gluteal nerves, which innervate the muscles of the buttocks.
Function of the Sacral Plexus
The sacral plexus plays a crucial role in carrying sensory and motor signals between the lower limbs and the central nervous system. It acts as a communication highway, transmitting vital information that allows us to move, feel, and respond to stimuli in our legs and pelvis.
Motor signals originating from the central nervous system travel through the sacral plexus to reach the muscles of the lower limbs, enabling us to walk, run, jump, and perform various movements. The sacral plexus also carries sensory signals from the lower limbs back to the brain, allowing us to perceive touch, pain, temperature, and other sensations.
Additionally, the sacral plexus is involved in the coordination of reflexes in the legs and pelvis. Reflexes are involuntary responses that occur automatically in response to certain stimuli. For example, when you step on a sharp object, the sacral plexus helps initiate the reflex action that quickly withdraws your foot to avoid injury.
Overall, the sacral plexus is a remarkable structure that plays a fundamental role in the functioning of our lower limbs and pelvis. Its intricate anatomy and intricate network of nerves ensure the smooth transmission of signals, allowing us to move with precision and experience the world through our legs and feet.
The Sciatic Nerve: The Largest Nerve of the Sacral Plexus
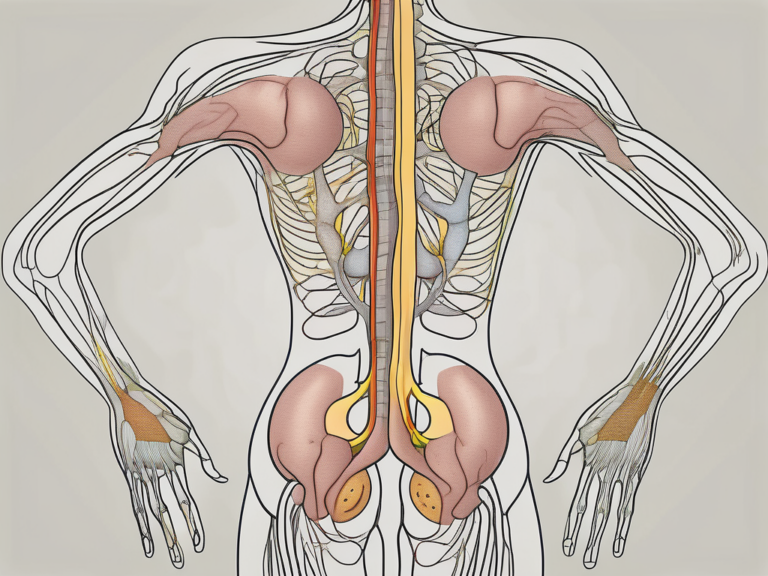
The sciatic nerve, a vital structure originating from the sacral plexus, is the largest nerve in the body. It is a composite nerve made up of two individual nerves – the tibial nerve and the common peroneal nerve.
The sciatic nerve, also known as the ischiadic nerve, plays a crucial role in the functioning of the lower limb. It is responsible for transmitting signals between the brain and the leg, allowing for movement and sensation.
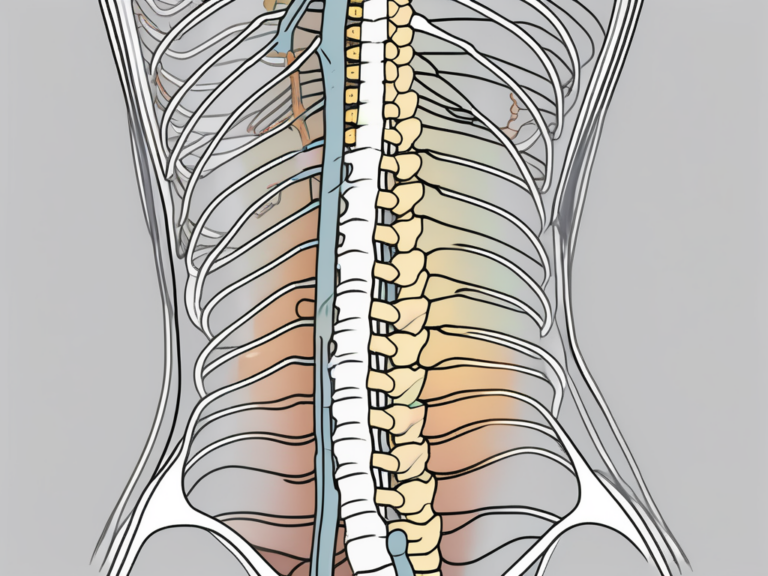
Anatomy of the Sciatic Nerve
The sciatic nerve begins its journey in the pelvis, where it emerges from the sacral plexus. This plexus is a network of nerves that arise from the lower spinal cord. From its origin, the sciatic nerve travels through the buttocks and continues down the back of the thigh.
As it descends, the sciatic nerve branches out into smaller nerves that supply the lower leg and foot. These branches include the tibial nerve and the common peroneal nerve, which are responsible for different functions within the leg.
The tibial nerve, one of the branches of the sciatic nerve, innervates the muscles of the posterior compartment of the leg. It controls the movement of important muscles such as the gastrocnemius, soleus, and tibialis posterior. These muscles play a key role in activities such as walking, running, and maintaining balance.
The common peroneal nerve, another branch of the sciatic nerve, innervates the muscles of the anterior and lateral compartments of the leg. It controls the movement of muscles such as the peroneus longus and peroneus brevis, which are involved in ankle dorsiflexion and eversion. These movements are essential for activities such as walking on uneven surfaces and maintaining stability.
Function of the Sciatic Nerve
The sciatic nerve is responsible for providing both motor and sensory functions to the leg and foot. It controls the movement of the muscles in the lower limb and transmits sensations of touch, temperature, and pain from the leg and foot to the brain.
Motor function: The sciatic nerve carries signals from the brain to the muscles of the leg, allowing for voluntary movement. It enables actions such as walking, running, and jumping by coordinating the contraction and relaxation of various leg muscles.
Sensory function: In addition to motor control, the sciatic nerve also plays a crucial role in transmitting sensory information from the leg and foot to the brain. It carries signals related to touch, temperature, and pain, allowing us to perceive and respond to our environment. For example, when we step on a sharp object, the sciatic nerve quickly relays the sensation of pain to the brain, triggering a reflexive withdrawal of the foot.
Disorders of the Sciatic Nerve: Despite its importance, the sciatic nerve can be susceptible to various disorders. One common condition is sciatica, which refers to pain that radiates along the path of the sciatic nerve. This pain can be caused by a herniated disc, spinal stenosis, or other conditions that compress or irritate the nerve.
In conclusion, the sciatic nerve is a vital component of the sacral plexus and the largest nerve in the body. Its intricate anatomy and multifaceted functions make it a fascinating structure to study. Understanding the sciatic nerve helps us appreciate the complexity of the human nervous system and the remarkable capabilities it provides for movement and sensation in the lower limb.
Conditions Affecting the Sacral Plexus
Several conditions can affect the sacral plexus and its main nerve, the sciatic nerve. One common condition is sciatica, which affects millions of people worldwide.
Sciatica: A Common Condition Affecting the Sciatic Nerve
Sciatica occurs when there is compression or irritation of the sciatic nerve. This can result in pain, numbness, tingling, or weakness along the path of the nerve, typically radiating from the lower back down the back of the leg.
Sciatica can be caused by various factors, including herniated discs, spinal stenosis, or muscle imbalances. It is often characterized by sharp, shooting pain that can be debilitating for those affected. The pain may worsen with certain movements or prolonged sitting or standing.
While sciatica is commonly associated with older adults, it can affect individuals of all ages. Certain occupations or activities that involve repetitive movements or prolonged sitting can increase the risk of developing sciatica.
Fortunately, most cases of sciatica can be managed with conservative treatments such as physical therapy, pain medication, and lifestyle modifications. In severe cases, surgical intervention may be necessary to alleviate the compression on the sciatic nerve.
Other Disorders of the Sacral Plexus
Aside from sciatica, there are other disorders that can affect the sacral plexus, such as sacral plexopathy, piriformis syndrome, or nerve root impingement. These conditions can cause similar symptoms and may require medical attention for diagnosis and treatment.
Sacral plexopathy refers to a dysfunction or damage to the sacral plexus, which can result from trauma, tumors, or infections. Symptoms may include pain, weakness, or sensory disturbances in the lower extremities.
Piriformis syndrome is a condition where the piriformis muscle, located deep in the buttocks, compresses the sciatic nerve. This can lead to sciatica-like symptoms, including pain, numbness, or tingling in the buttocks and down the leg. Physical therapy, stretching exercises, and medication are commonly used to manage piriformis syndrome.
Nerve root impingement occurs when a nerve root in the lower spine becomes compressed or irritated. This can cause radiating pain, numbness, or weakness in the lower back, buttocks, and legs. Treatment options may include physical therapy, medication, or in some cases, surgical intervention.
It is important to consult with a healthcare professional if you experience persistent or worsening symptoms related to the sacral plexus. Proper diagnosis and treatment can help alleviate pain and improve quality of life.
Diagnosis and Treatment of Sacral Plexus Disorders
When it comes to diagnosing and treating sacral plexus disorders, it is crucial to consult with a healthcare professional. They will conduct a thorough physical examination, review medical history, and may order further diagnostic tests to determine the underlying cause of the symptoms.
Sacral plexus disorders can present with a variety of symptoms, including pain, numbness, tingling, and weakness in the lower back, hips, buttocks, and legs. These symptoms can greatly impact a person’s quality of life and ability to perform daily activities. Therefore, it is important to seek prompt medical attention for an accurate diagnosis and appropriate treatment.
Diagnostic Techniques for Sacral Plexus Disorders
Diagnostic techniques may include imaging studies, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, to visualize the sacral plexus and identify any abnormalities. These imaging tests provide detailed images of the nerves, bones, and soft tissues in the pelvic region, allowing healthcare professionals to assess the condition of the sacral plexus.
In addition to imaging studies, electromyography (EMG) and nerve conduction studies may also be conducted to assess the function of the nerves. EMG involves the insertion of small needles into the muscles to record their electrical activity, while nerve conduction studies measure the speed and strength of electrical signals as they travel along the nerves.
These diagnostic tests help healthcare professionals determine the extent and location of the nerve damage, as well as the underlying cause of the sacral plexus disorder. By identifying the specific problem, they can develop an individualized treatment plan to address the patient’s needs.
Treatment Options for Sacral Plexus Disorders
The treatment for sacral plexus disorders depends on the underlying cause and severity of the condition. It may involve a combination of conservative approaches like rest, physical therapy, medication, and lifestyle modifications.
Rest is an important component of the treatment plan as it allows the body to heal and reduces stress on the affected nerves. Physical therapy plays a crucial role in improving strength, flexibility, and mobility. A skilled physical therapist can design a personalized exercise program to target the specific muscles and nerves affected by the sacral plexus disorder.
In some cases, medication may be prescribed to manage pain, reduce inflammation, or address any underlying medical conditions contributing to the sacral plexus disorder. Nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, and neuropathic pain medications are commonly used to alleviate symptoms and improve the patient’s comfort.
Lifestyle modifications, such as maintaining a healthy weight, practicing good posture, and avoiding activities that exacerbate symptoms, can also play a significant role in managing sacral plexus disorders. These modifications help reduce strain on the affected nerves and promote overall well-being.
In more severe cases, when conservative treatments fail to provide relief, surgery may be necessary. Surgical interventions aim to alleviate pressure on the affected nerves, repair any damage, and restore normal function. The specific surgical procedure will depend on the underlying cause of the sacral plexus disorder and the individual patient’s needs.
It is important to note that the treatment approach for sacral plexus disorders is highly individualized. Each patient’s condition is unique, and healthcare professionals will tailor the treatment plan to address their specific needs and goals. Regular follow-up appointments and ongoing communication with the healthcare team are essential to monitor progress, make any necessary adjustments to the treatment plan, and ensure optimal outcomes.
Prevention and Management of Sacral Plexus Disorders
While it may not be possible to prevent all sacral plexus disorders, there are steps individuals can take to promote sacral plexus health and minimize the risk of developing certain conditions.
The sacral plexus is a complex network of nerves that plays a crucial role in the functioning of the lower limbs. It is responsible for transmitting signals from the spinal cord to the muscles and organs in the pelvic region. Any disruption or damage to the sacral plexus can lead to a variety of disorders, including sciatica, sacral plexopathy, and pelvic floor dysfunction.
Lifestyle Changes for Sacral Plexus Health
Lifestyle changes, such as maintaining a healthy weight, practicing good posture, and engaging in regular exercise, can help reduce the risk of developing sacral plexus disorders. Obesity and excessive weight gain can put extra pressure on the lower back and pelvic region, increasing the likelihood of nerve compression and damage. By maintaining a healthy weight, individuals can alleviate this pressure and promote optimal sacral plexus health.
Practicing good posture is another essential aspect of sacral plexus health. Slouching or sitting in a hunched position for extended periods can strain the muscles and nerves in the lower back, leading to discomfort and potential nerve damage. By maintaining proper posture while sitting, standing, and walking, individuals can reduce the risk of sacral plexus disorders and promote overall spinal health.
Incorporating regular exercise into one’s routine is also crucial for sacral plexus health. Engaging in activities that strengthen the core muscles, such as yoga, Pilates, or weightlifting, can provide stability and support to the lower back and pelvic region. Additionally, exercises that promote flexibility, such as stretching and yoga, can help prevent muscle imbalances and reduce the risk of nerve compression.
Furthermore, it is important to avoid activities that put excessive strain on the lower back and legs. Lifting heavy objects incorrectly, participating in high-impact sports without proper conditioning, or engaging in repetitive movements that stress the sacral plexus can all increase the risk of developing sacral plexus disorders. By being mindful of these activities and taking necessary precautions, individuals can protect the sacral plexus from potential harm.
Physical Therapy and Sacral Plexus Disorders
For individuals with sacral plexus disorders, physical therapy can be beneficial in managing symptoms and promoting recovery. Physical therapists are healthcare professionals who specialize in the evaluation and treatment of musculoskeletal and neurological conditions.
Physical therapy sessions for sacral plexus disorders typically involve a comprehensive assessment of the individual’s condition, including a thorough examination of their range of motion, strength, and functional abilities. Based on the findings, the physical therapist will develop a customized exercise program to address the specific needs of the patient.
The exercise program may include a combination of stretching, strengthening, and balance exercises to improve the function of the lower limbs. These exercises are designed to target the muscles surrounding the sacral plexus, promoting flexibility, stability, and overall function.
In addition to exercise, physical therapists may also incorporate other treatment modalities into the rehabilitation plan. These may include manual therapy techniques, such as joint mobilization or soft tissue massage, to alleviate pain and improve mobility. Electrical stimulation, ultrasound therapy, and heat or cold therapy may also be utilized to reduce inflammation, promote healing, and manage symptoms.
Furthermore, physical therapists can provide education and guidance on proper body mechanics and ergonomics to prevent further injury and promote long-term sacral plexus health. They can teach individuals how to perform daily activities, such as lifting, bending, and sitting, in a way that minimizes strain on the lower back and pelvic region.
In conclusion, while it may not be possible to prevent all sacral plexus disorders, individuals can take proactive steps to promote sacral plexus health and minimize the risk of developing certain conditions. Lifestyle changes, such as maintaining a healthy weight, practicing good posture, and engaging in regular exercise, can play a significant role in preventing sacral plexus disorders. Additionally, physical therapy can be an effective treatment option for individuals with sacral plexus disorders, helping to manage symptoms and promote recovery. By prioritizing sacral plexus health and seeking appropriate care, individuals can optimize their overall well-being and quality of life.
Conclusion
In conclusion, the sciatic nerve is the largest nerve of the sacral plexus. Understanding the anatomy and function of the sacral plexus, as well as the conditions that can affect it, is crucial for individuals experiencing symptoms related to the lower limbs. If you suspect you have a sacral plexus disorder, it is essential to consult with a healthcare professional who can provide expert guidance and recommend the appropriate diagnostic and treatment options for your specific condition.