What Is the Largest Nerve from the Sacral Plexus?
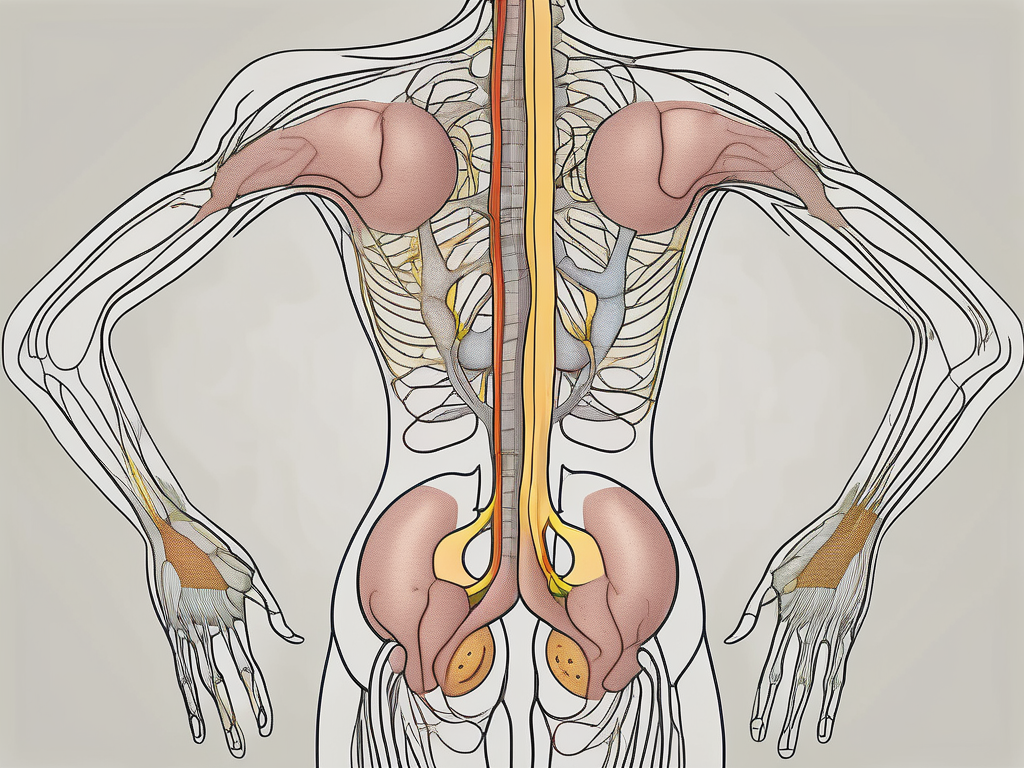
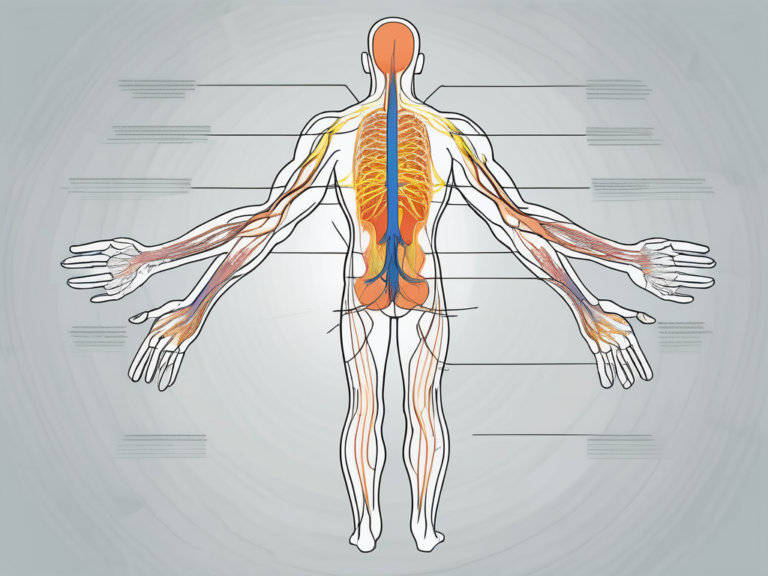
The sacral plexus is a complex network of nerves located in the lower back, formed by the fusion of the fourth and fifth lumbar nerves and the first, second, third, and fourth sacral nerves. It supplies nerves to the pelvis, genitals, and lower limbs, playing a crucial role in motor and sensory functions. Within the intricate system of the sacral plexus, the largest nerve is the sciatic nerve.
Understanding the Sacral Plexus
The sacral plexus is a vital component of the peripheral nervous system. It originates from the lower spinal cord and extends down to the pelvis, where it branches out to various nerves responsible for transmitting signals between the brain and the lower body. This complex network is essential for transmitting information related to movement, sensation, and organ function in the pelvis and lower limbs.
The sacral plexus is a fascinating structure that plays a crucial role in the overall functioning of the human body. Let’s delve deeper into its anatomy and functions to gain a better understanding of its importance.
Anatomy of the Sacral Plexus
The sacral plexus consists of multiple nerves, including the sciatic nerve, pudendal nerve, superior gluteal nerve, and many more. These nerves arise from the roots of the fourth lumbar to the fourth sacral nerves and form a network that supplies nerves to various regions of the lower body.
One of the major nerves in the sacral plexus is the sciatic nerve, which is the longest and thickest nerve in the human body. It originates from the sacral plexus and extends down the back of the thigh, branching out to provide motor and sensory innervation to the lower leg and foot. The sciatic nerve is responsible for controlling movements such as walking, running, and jumping, as well as providing sensations like touch, pain, and temperature perception.
Another important nerve in the sacral plexus is the pudendal nerve, which is responsible for innervating the pelvic region. It controls the muscles of the perineum, which are essential for bladder and bowel control, as well as sexual function. The pudendal nerve also provides sensory innervation to the external genitalia, perineum, and anus.
Functions of the Sacral Plexus
The sacral plexus plays a crucial role in motor and sensory functions of the lower body. It facilitates movement of the lower limbs and provides sensations such as touch, pain, and temperature perception. Additionally, it innervates the pelvic organs, controlling bladder and bowel function, as well as sexual function.
When you walk, run, or perform any movement with your lower limbs, it is the sacral plexus that coordinates the muscle contractions and ensures smooth and coordinated movements. Without the sacral plexus, even simple tasks like walking would be impossible.
In addition to motor functions, the sacral plexus also provides sensory feedback from the lower body to the brain. This feedback allows us to perceive sensations like touch, pain, and temperature. For example, when you step on a sharp object, it is the sacral plexus that transmits the pain signal to your brain, alerting you to the potential danger.
Furthermore, the sacral plexus plays a vital role in controlling bladder and bowel function. It innervates the muscles that control the release of urine and feces, ensuring proper functioning of the urinary and digestive systems. Additionally, it is involved in sexual function, providing innervation to the genital organs and facilitating sexual arousal and orgasm.
Any disruption or damage to the sacral plexus can lead to a variety of symptoms and conditions. For example, injuries to the sciatic nerve can result in sciatica, a condition characterized by pain, numbness, and weakness in the lower back, buttocks, and legs. Damage to the pudendal nerve can lead to urinary and fecal incontinence, sexual dysfunction, and loss of sensation in the pelvic region.
In conclusion, the sacral plexus is a complex and intricate network of nerves that plays a crucial role in the motor and sensory functions of the lower body. It is responsible for coordinating movements, providing sensations, and controlling bladder, bowel, and sexual function. Understanding the anatomy and functions of the sacral plexus is essential for appreciating the intricate workings of the human body.
The Sciatic Nerve: The Largest Nerve from the Sacral Plexus
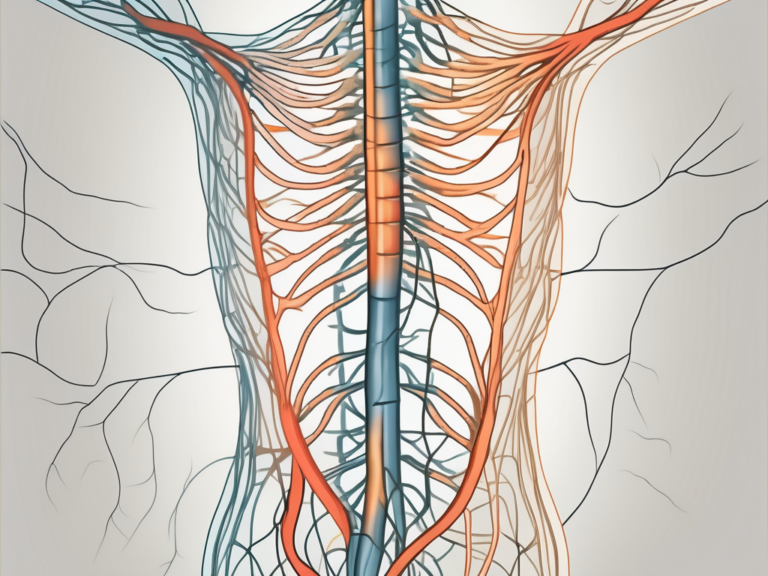
The sciatic nerve, originating from the sacral plexus, is the largest nerve in the body. It is a combination of multiple nerves, primarily the L4, L5, S1, S2, and S3 nerve roots. This nerve extends from the lower back, through the buttocks, and down the back of each leg.
The sciatic nerve is a vital component of the body’s nervous system, playing a crucial role in enabling movement and providing sensation to the lower limbs. It is an intricate network of nerve fibers that allows us to perform various activities such as walking, running, standing, and sitting.
Anatomy of the Sciatic Nerve
The sciatic nerve is composed of two main branches, the tibial nerve and the common peroneal nerve. These branches innervate different muscles and provide sensation to distinct areas of the leg.
The tibial nerve, one of the branches of the sciatic nerve, supplies the muscles located on the back part of the leg and the sole of the foot. It is responsible for the movement and coordination of these muscles, allowing us to perform activities such as walking, running, and jumping with ease.
On the other hand, the common peroneal nerve, another branch of the sciatic nerve, innervates the muscles on the front and side of the leg and the top of the foot. It plays a crucial role in controlling the movement and coordination of these muscles, enabling activities such as lifting the foot, flexing the toes, and maintaining balance.
Functions of the Sciatic Nerve
The sciatic nerve is responsible for enabling movement and providing sensation to the lower limbs. It controls the muscles needed for walking, running, standing, and sitting.
When we walk or run, the sciatic nerve sends signals to the muscles in our legs, coordinating their contractions and relaxations to produce smooth and coordinated movements. It ensures that our steps are stable and balanced, preventing us from stumbling or falling.
In addition to motor functions, the sciatic nerve also provides sensory information to the brain. It allows us to feel sensations such as touch, temperature, and pain in the lower limbs. This sensory feedback is essential for our body’s awareness of its surroundings and helps us navigate the world safely.
However, any injury or compression of the sciatic nerve can result in pain, weakness, tingling, numbness, and difficulty in performing everyday activities. Conditions such as sciatica, which is characterized by pain radiating along the path of the sciatic nerve, can significantly impact a person’s quality of life.
Therefore, it is crucial to take care of the sciatic nerve and maintain its health. Regular exercise, proper posture, and avoiding prolonged sitting or standing can help prevent issues related to the sciatic nerve. If any symptoms or discomfort arise, it is advisable to seek medical attention to ensure timely diagnosis and appropriate treatment.
Other Nerves Originating from the Sacral Plexus
In addition to the sciatic nerve, the sacral plexus gives rise to several other important nerves that contribute to motor and sensory functions of the lower body.
The sacral plexus, a complex network of nerves located in the pelvic region, is responsible for innervating various muscles and providing sensation to different areas of the lower body. While the sciatic nerve is perhaps the most well-known nerve originating from the sacral plexus, there are several other nerves that play crucial roles in maintaining proper function and movement.
Pudendal Nerve
The pudendal nerve, derived from the sacral plexus, is a vital nerve that supplies the muscles of the pelvic floor. These muscles are responsible for crucial functions such as urinary and bowel control. Additionally, the pudendal nerve provides sensation to the perineum and external genitalia, contributing to sexual pleasure and overall genital sensation.
When the pudendal nerve becomes dysfunctional, it can result in a condition known as pudendal neuralgia. This condition is characterized by chronic pain, numbness, and tingling in the pelvic region, perineum, and external genitalia. Pudendal neuralgia can significantly impact a person’s quality of life, causing discomfort and difficulty with bladder and bowel function.
Superior Gluteal Nerve
The superior gluteal nerve, another significant nerve stemming from the sacral plexus, plays a crucial role in the movement and stability of the hip joint. It innervates important muscles such as the gluteus medius, gluteus minimus, and tensor fasciae latae.
The gluteus medius and gluteus minimus muscles are responsible for abduction and rotation of the hip joint, while the tensor fasciae latae muscle aids in hip flexion and stabilization. These muscles are essential for maintaining proper posture, balance, and overall lower body movement.
Injury to the superior gluteal nerve can have significant consequences, leading to weakness or paralysis of the affected muscles. This can result in difficulties with walking, running, and other lower body movements. It may also cause an imbalance in hip movement, leading to compensatory changes in gait and posture.
Understanding the intricate network of nerves originating from the sacral plexus provides valuable insights into the complexity of the human body. The proper functioning of these nerves is crucial for maintaining motor control and sensory perception in the lower body. By appreciating the role of nerves such as the pudendal nerve and the superior gluteal nerve, we gain a deeper understanding of the intricate mechanisms that allow us to move, sense, and interact with the world around us.
Common Disorders Associated with the Sacral Plexus
The sacral plexus is a complex network of nerves located in the pelvis. It plays a vital role in transmitting signals between the spinal cord and the lower extremities. Unfortunately, this intricate system is susceptible to various disorders that can cause significant discomfort and impair daily activities. Understanding these conditions and their causes is crucial for early detection and appropriate management.
One of the most common disorders associated with the sacral plexus is sciatica. Sciatica occurs when the sciatic nerve, which originates from the sacral plexus, is compressed or irritated. This compression can be due to a herniated disc, bone spurs, spinal stenosis, or even muscle imbalances. Individuals with sciatica may experience pain, tingling, numbness, or weakness along the path of the sciatic nerve, which extends from the lower back down to the buttocks, thighs, and legs.
Treatment for sciatica may involve a combination of medications, physical therapy, and in some cases, surgery. Nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce inflammation and alleviate pain. Physical therapy exercises can strengthen the muscles supporting the spine and improve flexibility. In severe cases, surgical intervention may be necessary to relieve pressure on the sciatic nerve. If you are experiencing symptoms of sciatica, it is essential to consult with a healthcare professional for an accurate diagnosis and appropriate treatment.
Another disorder associated with the sacral plexus is pudendal neuralgia. Pudendal neuralgia is a condition characterized by chronic pain in the pelvic and genital area, caused by irritation or damage to the pudendal nerve. The pudendal nerve, originating from the sacral plexus, supplies sensation to the perineum, anus, and genitals.
Individuals with pudendal neuralgia may experience a variety of symptoms, including sharp or burning pain, numbness, and discomfort during sexual intercourse or prolonged sitting. The pain can be debilitating and significantly impact a person’s quality of life. It is important to note that pudendal neuralgia is often misdiagnosed or overlooked, as its symptoms can mimic other pelvic pain conditions.
Treatment options for pudendal neuralgia include medications, nerve blocks, physical therapy, and occasionally surgery. Medications such as anticonvulsants or tricyclic antidepressants can help alleviate nerve pain. Nerve blocks, which involve injecting an anesthetic or steroid into the affected nerve, can provide temporary relief. Physical therapy techniques, such as pelvic floor muscle relaxation exercises and nerve gliding exercises, can help reduce pain and improve function. In severe cases, surgical decompression of the pudendal nerve may be considered.
If you suspect you may have pudendal neuralgia or any other disorder associated with the sacral plexus, it is crucial to seek medical advice from a healthcare provider specialized in pelvic pain disorders. Early diagnosis and appropriate treatment can significantly improve symptoms and enhance your overall well-being.
Treatment and Management of Sacral Plexus Disorders
The treatment and management of sacral plexus disorders depend on the specific condition and its underlying cause. It is essential to consult with a healthcare professional or specialist to formulate an appropriate treatment plan. Sacral plexus disorders can cause significant pain and discomfort, affecting an individual’s quality of life. Therefore, it is crucial to explore various treatment options to find the most effective approach for each patient.
When it comes to non-surgical treatments for sacral plexus disorders, there are several options available. One common approach is medication to manage pain and inflammation. Nonsteroidal anti-inflammatory drugs (NSAIDs) may be prescribed to reduce swelling and alleviate discomfort. Additionally, analgesics or pain relievers may be recommended to help control pain symptoms. It is important to follow the prescribed dosage and guidelines provided by the healthcare professional to ensure safe and effective use of these medications.
In addition to medication, physical therapy plays a significant role in the treatment and management of sacral plexus disorders. Physical therapists can design personalized exercise programs to improve strength, flexibility, and overall function. These exercises may include stretching, strengthening, and balance training. Physical therapy can also help individuals regain mobility and reduce the risk of future injuries. It is essential to commit to the recommended physical therapy regimen and attend regular sessions to achieve optimal results.
Lifestyle modifications are another crucial aspect of managing sacral plexus disorders. These modifications may involve changes in daily activities, posture, and ergonomics. For example, individuals may be advised to avoid prolonged sitting or standing, use proper body mechanics when lifting heavy objects, and maintain good posture throughout the day. Additionally, incorporating relaxation techniques, such as deep breathing exercises or meditation, can help reduce stress and promote overall well-being.
Complementary therapies, such as acupuncture or chiropractic care, may also be beneficial for some individuals with sacral plexus disorders. Acupuncture involves the insertion of thin needles into specific points on the body to stimulate healing and relieve pain. Chiropractic care focuses on the alignment of the spine and nervous system through manual adjustments. These alternative treatments can provide additional pain relief and improve overall function. However, it is important to consult with a qualified practitioner and inform them about your specific condition before pursuing these therapies.
In certain cases, surgical intervention may be necessary to address sacral plexus disorders. Surgical procedures may involve decompression of nerves, removal of herniated discs, or the repair of damaged nerves. These surgical interventions aim to alleviate pressure on the affected nerves and restore proper function. If surgery is recommended as part of your treatment plan, it is crucial to thoroughly discuss the potential risks, benefits, and expected outcomes with your healthcare provider. They will provide you with detailed information and help you make an informed decision.
In conclusion, the treatment and management of sacral plexus disorders require a comprehensive approach tailored to each individual’s specific needs. Non-surgical treatments, such as medication, physical therapy, and lifestyle modifications, can provide significant relief and improve overall function. Complementary therapies, like acupuncture or chiropractic care, may offer additional benefits for some individuals. In certain cases, surgical intervention may be necessary to address the underlying cause of the disorder. Consulting with a healthcare professional or specialist is crucial to develop an effective treatment plan and achieve the best possible outcomes.
The Future of Sacral Plexus Research
Ongoing research in the field of sacral plexus disorders holds promise for improved diagnostics and treatment approaches.
Advances in Treatment Approaches
Advancements in treatment approaches for sacral plexus disorders are focusing on minimizing invasiveness and maximizing efficacy. Researchers are exploring novel therapies, such as targeted drug delivery, nerve stimulation techniques, and regenerative medicine approaches, to promote nerve regeneration and functional recovery.
Potential Breakthroughs in Understanding the Sacral Plexus
Scientists are continually enhancing our understanding of the sacral plexus and its intricate connections. Ongoing studies aim to unravel the mechanisms of nerve injury, repair, and regeneration, leading to potential breakthroughs in the prevention and treatment of sacral plexus disorders.
In conclusion, the sciatic nerve is the largest nerve originating from the sacral plexus. Its anatomy and function are intricately tied to the well-being of the lower body. Understanding the sacral plexus, its other branches, and the common disorders associated with it is crucial for early detection and appropriate management. If you suspect you may have a sacral plexus disorder or are experiencing related symptoms, it is vital to consult with a healthcare professional who can provide accurate diagnosis and guide you through the best treatment options available.