What Is a Sacral Nerve Stimulator? A Comprehensive Guide
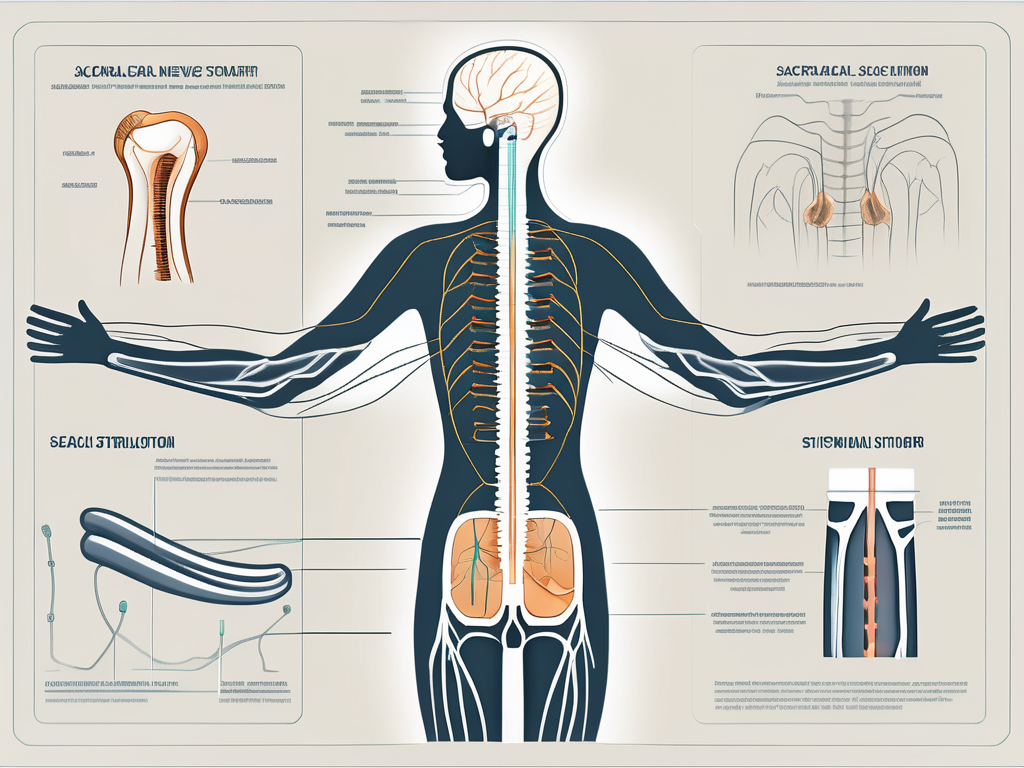
Sacral nerve stimulators are innovative medical devices that have revolutionized the treatment of various medical conditions. By stimulating the sacral nerve, these devices offer hope and relief to individuals suffering from conditions such as overactive bladder and chronic pain. In this comprehensive guide, we will delve into the world of sacral nerve stimulation, exploring its anatomy, function, medical applications, procedure, and life after implantation.
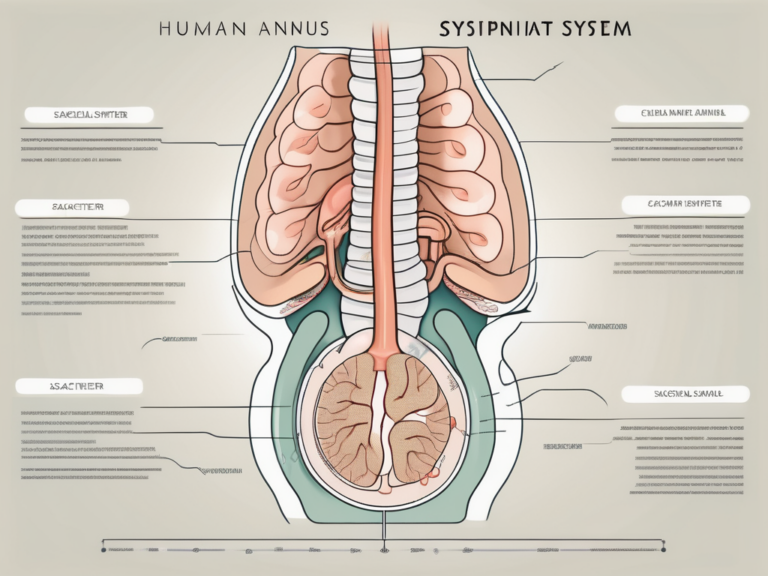
Understanding the Sacral Nerve
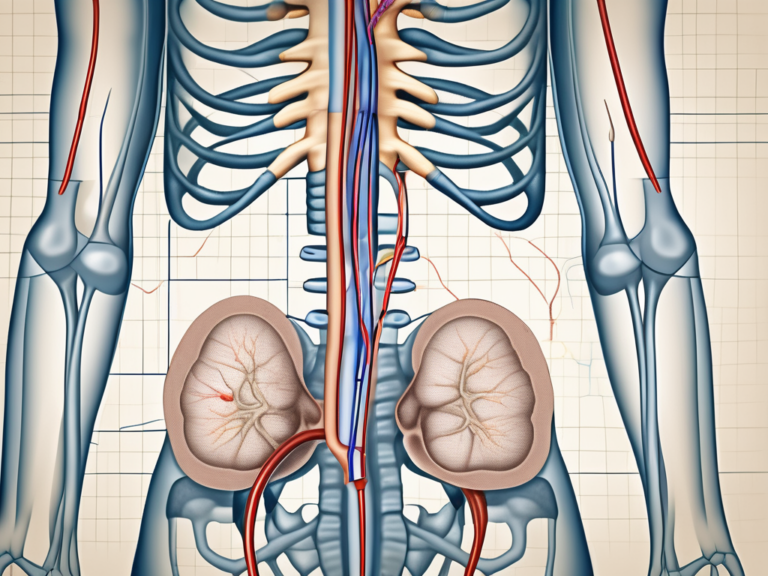
The sacral nerve, also known as the S1-S4 nerve roots, plays a crucial role in the innervation of the pelvic region. It is responsible for coordinating the functioning of the bladder, bowel, and sexual organs. The sacral nerve is an intricate network of nerves that transmit signals between these organs and the central nervous system.
Anatomy of the Sacral Nerve
The sacral nerve is composed of a complex network of nerves originating from the spinal cord. It extends from the lower back down to the tailbone and branches out to supply the pelvic organs.
Within the sacral nerve, there are four nerve roots: S1, S2, S3, and S4. These roots emerge from the spinal cord and form a bundle that travels through the sacral canal. As they exit the sacral canal, the nerve roots divide into smaller branches, which then innervate specific areas of the pelvic region.
The S1 nerve root, the largest of the four, supplies sensation to the back of the thigh and calf, as well as the outer edge of the foot. It also plays a role in controlling the muscles that enable ankle movement.
The S2 nerve root provides sensation to the back of the thigh, the inner side of the foot, and the buttocks. It also contributes to the motor control of the hip and knee joints.
The S3 nerve root is responsible for sensation in the buttocks and the inner thighs. It also helps control the muscles involved in bowel and bladder function.
The S4 nerve root, the smallest of the four, primarily innervates the perineum, which includes the area between the anus and the genitals. It plays a crucial role in sexual function and the control of the external anal sphincter.
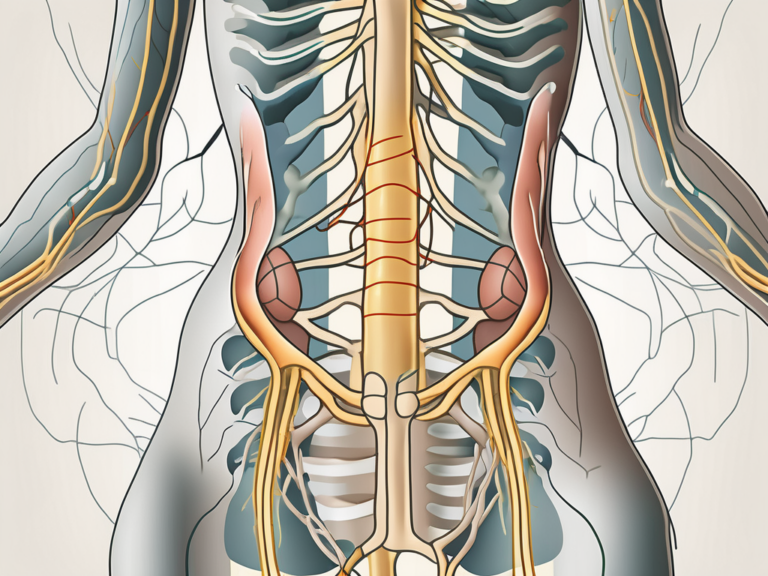
Function of the Sacral Nerve
The sacral nerve controls the contraction and relaxation of the bladder, allowing for proper urine storage and voiding. When the bladder is full, sensory signals are transmitted from the bladder to the sacral nerve, triggering the urge to urinate. The sacral nerve then sends motor signals back to the bladder, causing it to contract and expel urine.
In addition to bladder control, the sacral nerve also regulates bowel movements. It coordinates the relaxation and contraction of the muscles in the rectum and anus, enabling the expulsion of feces during defecation.
Furthermore, the sacral nerve contributes to sexual function by controlling genital sensation and orgasm. It plays a role in transmitting pleasurable sensations from the genitals to the brain, allowing for sexual arousal and climax.
When the sacral nerve is damaged or dysfunctional, it can lead to various pelvic disorders. For example, damage to the sacral nerve may result in urinary incontinence, where the individual has difficulty controlling their bladder. It can also cause bowel dysfunction, leading to constipation or fecal incontinence. Additionally, sexual dysfunction, such as erectile dysfunction or loss of sensation, can occur when the sacral nerve is affected.
Overall, the sacral nerve is a vital component of the nervous system, responsible for the proper functioning of the pelvic organs. Its intricate anatomy and multifaceted functions highlight its importance in maintaining urinary, bowel, and sexual health.
Introduction to Sacral Nerve Stimulation
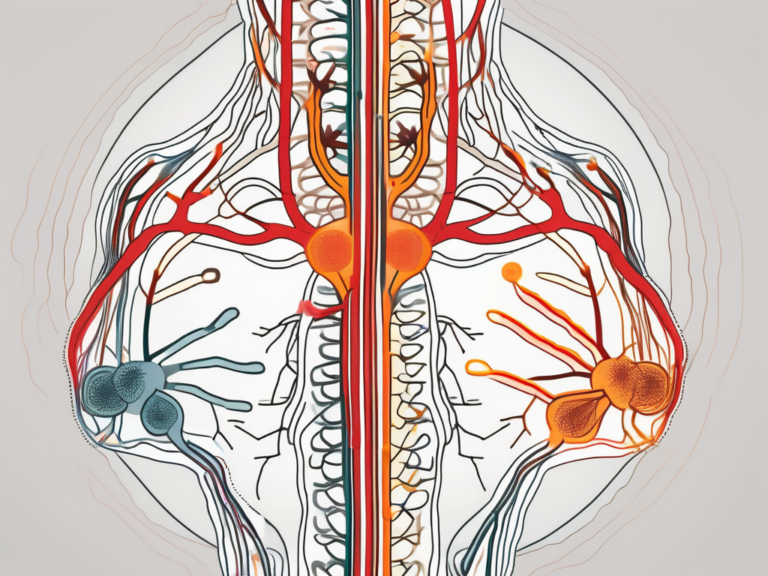
Sacral nerve stimulation is a therapeutic approach that involves the use of an implanted device to modulate the activity of the sacral nerve. By delivering electrical impulses to the nerve, it aims to restore normal function and alleviate symptoms associated with certain medical conditions.
The sacral nerve, also known as the S3 nerve, plays a crucial role in the functioning of the lower urinary tract and pelvic floor muscles. It is responsible for transmitting signals between the brain and the bladder, bowel, and pelvic organs. When the sacral nerve is not functioning properly, it can lead to a range of debilitating symptoms, such as urinary incontinence, urinary retention, fecal incontinence, and chronic pelvic pain.
The Concept of Nerve Stimulation
Nerve stimulation has been used for decades to manage various neurological disorders. It works on the principle that controlled electrical stimulation can modulate the activity of specific nerves, thereby influencing their function.
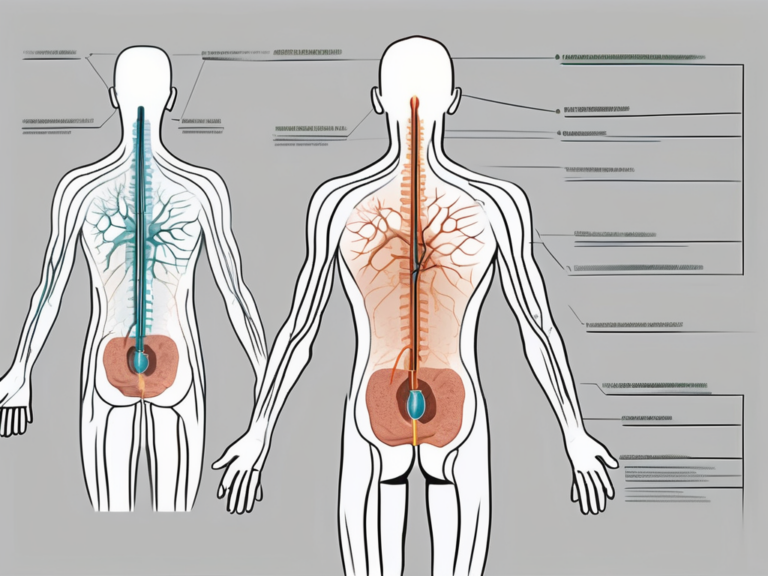
During sacral nerve stimulation, a small device, similar to a pacemaker, is surgically implanted near the sacral nerve. This device delivers mild electrical impulses to the nerve, which helps to regulate its activity. The electrical stimulation can be adjusted based on the individual’s needs, ensuring optimal therapeutic effects.
Research has shown that nerve stimulation can have profound effects on the nervous system. It can help to restore normal nerve function, improve muscle control, and alleviate pain. The exact mechanisms by which nerve stimulation works are still being studied, but it is believed to involve the modulation of nerve signals and the release of neurotransmitters.
The Role of Sacral Nerve Stimulation
In the context of sacral nerve stimulation, the goal is to regulate the activity of the sacral nerve to improve bladder control, relieve chronic pain, and enhance overall quality of life.
For individuals with urinary incontinence, sacral nerve stimulation can be a life-changing treatment option. It can help to reduce or eliminate episodes of involuntary urine leakage, allowing individuals to regain control over their bladder function. This can significantly improve their quality of life, boost self-confidence, and eliminate the need for constant use of absorbent pads or diapers.
Moreover, sacral nerve stimulation has shown promising results in managing chronic pelvic pain. By modulating the activity of the sacral nerve, it can help to alleviate pain and discomfort associated with conditions such as interstitial cystitis, endometriosis, and pudendal neuralgia. This can provide much-needed relief for individuals who have been suffering from debilitating pain for an extended period.
Additionally, sacral nerve stimulation has been found to be effective in treating fecal incontinence. By stimulating the sacral nerve, it can improve the coordination of the pelvic floor muscles and the rectum, leading to better bowel control and a reduction in episodes of fecal leakage.
In conclusion, sacral nerve stimulation is a valuable therapeutic approach for managing various medical conditions. By modulating the activity of the sacral nerve, it can restore normal function, alleviate symptoms, and improve overall quality of life. Further research and advancements in this field hold the potential for even more effective treatments in the future.
The Sacral Nerve Stimulator Device
The sacral nerve stimulator device consists of several components that work together to provide therapeutic benefits. These devices are typically composed of a generator, leads, and an external control unit.
Components of a Sacral Nerve Stimulator
The generator is the main component of the device and is responsible for delivering electrical impulses to the sacral nerve. It is implanted under the skin in the lower abdomen or buttock. The leads, thin insulated wires, are placed near the sacral nerve to deliver the electrical stimulation. The external control unit, usually a handheld device, allows the patient or healthcare provider to adjust the stimulation settings.
The generator is a small, battery-powered device that is designed to last for several years. It is made up of a pulse generator, a battery, and a circuit board. The pulse generator generates the electrical impulses that are delivered to the sacral nerve. The battery provides the power needed to operate the device, and the circuit board controls the timing and intensity of the electrical stimulation.
The leads are carefully placed near the sacral nerve during a surgical procedure. These leads are made of flexible materials that allow them to be positioned accurately and comfortably. Once in place, the leads are connected to the generator through small incisions in the skin. The leads are then secured in place to ensure that they do not move or become dislodged.
The external control unit is an essential part of the sacral nerve stimulator device. It allows the patient or healthcare provider to adjust the stimulation settings according to the individual’s needs. The control unit is usually a handheld device that is easy to use and navigate. It may have buttons or a touchscreen interface that allows the user to increase or decrease the intensity of the electrical stimulation, change the frequency of the impulses, or turn the device on and off.
How Does a Sacral Nerve Stimulator Work?
When the sacral nerve stimulator is activated, it sends electrical signals to the sacral nerve, modulating its activity. This stimulation alters the nerve’s response and restores normal function to the pelvic organs, thereby improving urinary control, reducing chronic pain, or addressing other conditions being targeted.
The electrical impulses generated by the sacral nerve stimulator mimic the natural signals that the brain sends to the sacral nerve. By modulating the nerve’s activity, the device can help regulate the function of the pelvic organs, such as the bladder, bowel, and muscles in the pelvic region. This can lead to improved urinary control, reduced pain, and enhanced quality of life for individuals suffering from conditions such as overactive bladder, urinary incontinence, or chronic pelvic pain.
The sacral nerve stimulator works by stimulating the sacral nerve at a specific frequency and intensity. The settings can be adjusted to meet the individual’s needs and can be modified over time as the patient’s condition changes. The device can be programmed to deliver continuous stimulation or intermittent bursts of electrical impulses, depending on the desired therapeutic effect.
It is important to note that the sacral nerve stimulator is not a cure for the underlying condition but rather a treatment option that can help manage symptoms and improve quality of life. The device should be used under the guidance of a healthcare professional who can determine the appropriate settings and monitor the patient’s progress.
Medical Conditions Treated with Sacral Nerve Stimulation
The application of sacral nerve stimulation spans across various medical conditions, providing therapeutic benefits and improving the quality of life for patients.
Sacral nerve stimulation, also known as sacral neuromodulation, is a minimally invasive procedure that involves the implantation of a small device near the sacral nerves. These nerves play a crucial role in controlling bladder and bowel function, as well as pelvic pain. By delivering mild electrical impulses to these nerves, sacral nerve stimulation helps regulate their activity, leading to improved symptoms and overall well-being.
Overactive Bladder and Sacral Nerve Stimulation
Overactive bladder is a condition characterized by a sudden and uncontrollable urge to urinate. It can significantly disrupt daily activities and negatively impact a person’s quality of life. While conservative measures such as behavioral modifications and medications are often the first line of treatment, some individuals may not respond well to these approaches.
Sacral nerve stimulation offers an alternative treatment method for individuals with overactive bladder who have not found relief with other therapies. By modulating the activity of the sacral nerves, this procedure can help regulate bladder function, reduce urinary urgency and frequency, and improve bladder control. Studies have shown that sacral nerve stimulation can provide long-term symptom improvement and enhance the quality of life for patients with overactive bladder.
Chronic Pain Management with Sacral Nerve Stimulation
Chronic pain conditions, such as interstitial cystitis, pudendal neuralgia, and chronic pelvic pain, can significantly impact a person’s daily life. These conditions often cause persistent discomfort, affecting physical and emotional well-being. Traditional pain management approaches, such as medications and physical therapy, may not always provide adequate relief for individuals with these conditions.
Sacral nerve stimulation has shown promise in providing pain relief and improving the overall well-being of individuals with chronic pain conditions. By targeting the sacral nerves involved in pain signaling, this procedure can help modulate pain perception and reduce the intensity of symptoms. Research studies have demonstrated that sacral nerve stimulation can lead to significant pain reduction and improved quality of life for patients with interstitial cystitis, pudendal neuralgia, and chronic pelvic pain.
Furthermore, sacral nerve stimulation is a reversible procedure, meaning that the device can be removed if the patient no longer wishes to continue with the treatment. This flexibility allows individuals to explore different treatment options and make informed decisions about their healthcare.
The Procedure of Sacral Nerve Stimulation
The implantation of a sacral nerve stimulator involves a surgical procedure that should be performed by a qualified healthcare professional. Let’s explore what to expect before, during, and after the procedure.
Preparing for the Procedure
Before the procedure, your healthcare provider will conduct a thorough evaluation and discuss the potential risks and benefits associated with sacral nerve stimulation. It is essential to share your complete medical history and any concerns or questions you may have. Pre-operative instructions, such as fasting and medication adjustments, will be provided.
What to Expect During the Procedure
During the procedure, you will be placed under anesthesia to ensure you are comfortable throughout. The surgeon will make small incisions to implant the generator and leads. The procedure duration may vary based on individual circumstances, but it is typically completed within a few hours.
Risks and Benefits of Sacral Nerve Stimulation
As with any medical procedure, there are potential risks and benefits associated with sacral nerve stimulation. Understanding these factors is crucial for making an informed decision regarding treatment.
Potential Risks and Complications
Complications associated with sacral nerve stimulation are rare but can include infection, bleeding, lead migration, and technical malfunctions. It is important to discuss these risks with your healthcare provider and determine if the potential benefits outweigh them in your specific case.
Benefits and Effectiveness of Sacral Nerve Stimulation
The benefits of sacral nerve stimulation can be life-changing for individuals suffering from conditions such as overactive bladder or chronic pain. Improved bladder control, reduced pain, and enhanced quality of life are common outcomes reported by patients who have undergone sacral nerve stimulation.
Life After Sacral Nerve Stimulation
After the surgical procedure, a period of recovery and adjustment follows. Understanding what to expect and how to navigate life with a sacral nerve stimulator is essential for long-term success.
Recovery and Aftercare
Following surgery, you will receive detailed instructions on post-operative care, including wound care, activity restrictions, and follow-up appointments. It is important to adhere to these instructions to ensure proper healing and optimize the effectiveness of sacral nerve stimulation.
Living with a Sacral Nerve Stimulator
Living with a sacral nerve stimulator device entails adapting to a few lifestyle modifications. You may need to avoid certain activities or adjust stimulation settings as directed by your healthcare provider. Regular follow-up visits will monitor your progress and allow for any necessary adjustments.
Frequently Asked Questions about Sacral Nerve Stimulation
Here are some common questions and answers that can provide additional insight into sacral nerve stimulation:
Is Sacral Nerve Stimulation Painful?
The implantation procedure is performed under anesthesia, ensuring that you will not experience pain during the surgery. After the procedure, you may experience discomfort or mild pain in the surgical area, which can be managed with prescribed pain medications.
Can a Sacral Nerve Stimulator be Removed?
While sacral nerve stimulators are intended to be long-term therapy, they can be removed if necessary. It is crucial to discuss the potential for device removal with your healthcare provider if you experience complications or changes in your condition that warrant its removal.
In conclusion, sacral nerve stimulation offers a comprehensive approach to addressing various medical conditions related to bladder function and chronic pain. With the help of an experienced healthcare provider, exploring the potential benefits, risks, and considerations of sacral nerve stimulation can lead to improved quality of life for individuals seeking relief from these conditions. If you are interested in exploring sacral nerve stimulation as a treatment option, consult with a qualified healthcare professional to determine if it is suitable for your specific needs.