Understanding the Lumbar Sacral Spine: Key Area for Sciatic Nerve Pain
The lumbar sacral spine plays a crucial role in the development of sciatic nerve pain, a condition that can cause significant discomfort and limit mobility. In order to better understand this connection and provide effective treatment options, it is important to have a comprehensive understanding of the anatomy of the lumbar sacral spine, the role of its vertebrae, as well as the intricate relationship between discs, nerves, and muscles.
Anatomy of the Lumbar Sacral Spine
The lumbar sacral spine is a fascinating and intricate part of the human body. Comprised of several vertebrae located in the lower back region, it serves as a crucial support system for the upper body and facilitates movement. Let’s delve deeper into the wonders of the lumbar sacral spine!
The Role of Vertebrae in the Lumbar Sacral Region
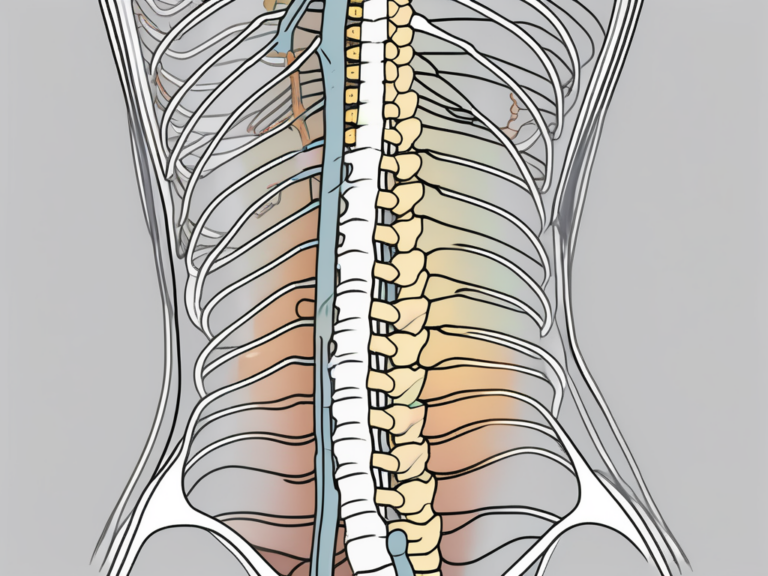
Each vertebra in the lumbar sacral spine is interconnected, forming a complex structure that not only supports the spinal cord but also provides remarkable flexibility. The lumbar vertebrae, in particular, are remarkable due to their larger size and shape, which grant them the ability to bear the weight of the body and absorb the forces exerted during various activities.
These lumbar vertebrae are not just strong; they are also designed to protect the delicate nerves passing through them. Their robust bony structure acts as a shield, ensuring the safety of the spinal cord and the nerves that branch off from it.
Discs, Nerves, and Muscles: Integral Components
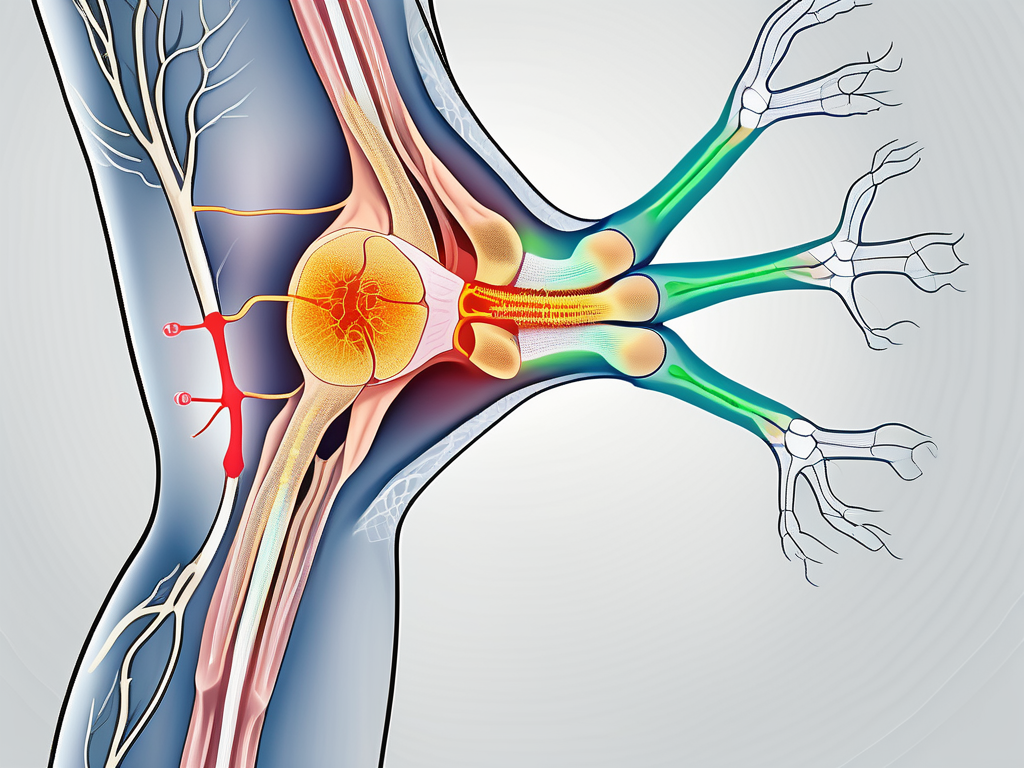
Between each lumbar vertebra, there are intervertebral discs that play a vital role in maintaining the spine’s health and functionality. These discs consist of two main parts: the tough outer layer called the annulus fibrosus and the gel-like inner core called the nucleus pulposus. Together, they form a dynamic duo that provides cushioning, prevents bone-to-bone contact, and allows the spine to bend and flex with ease.
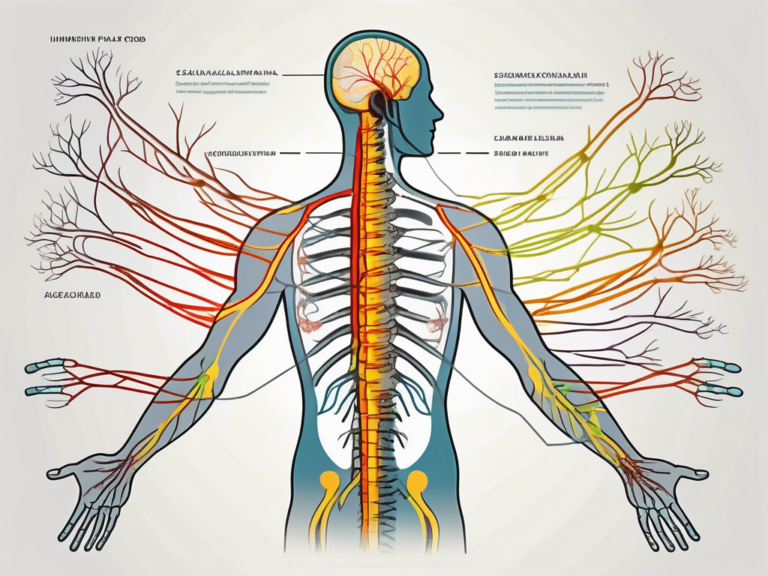
Adjacent to the vertebral bodies are pairs of spinal nerves that branch off from the spinal cord. These nerves are like messengers, transmitting signals between the brain and various parts of the body. In the case of the lumbar sacral spine, one nerve stands out in particular – the sciatic nerve. This nerve, known as the longest and thickest nerve in the body, plays a vital role in the lower back and lower limb function.
While the vertebrae and nerves are essential components of the lumbar sacral spine, we must not forget the muscles that surround and support this intricate structure. Strong core muscles, including those in the abdomen and lower back, play a crucial role in providing stability and allowing for movement. These muscles act as guardians, protecting the spine from excessive stress or injury and ensuring its overall well-being.
As we explore the anatomy of the lumbar sacral spine, we begin to appreciate the complexity and interconnectedness of its various components. From the robust vertebrae to the resilient intervertebral discs and the intricate network of nerves and muscles, each element plays a unique role in maintaining the spine’s strength, flexibility, and overall functionality. The lumbar sacral spine truly is a marvel of human anatomy!
The Connection Between Lumbar Sacral Spine and Sciatic Nerve
Understanding how the sciatic nerve passes through the lumbar sacral spine is essential in comprehending the relationship between these two areas. The sciatic nerve originates from the lower lumbar region and travels through the buttocks, down the back of the leg, and into the foot. It is responsible for providing sensory and motor functions to the lower body.
The lumbar sacral spine, also known as the lumbosacral spine, is the lower part of the vertebral column. It consists of five lumbar vertebrae and the sacrum, a triangular bone located at the base of the spine. The lumbar sacral spine plays a crucial role in supporting the upper body and facilitating movement.
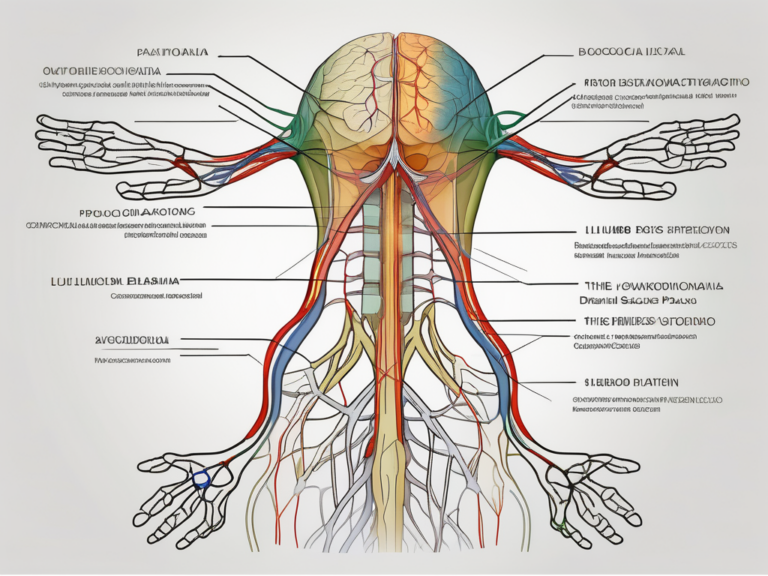
How the Sciatic Nerve Passes Through the Lumbar Sacral Spine
The sciatic nerve is formed by several nerve roots that emerge from the spinal cord in the lumbar sacral region. These nerve roots then come together to form the sciatic nerve, which exits the spine through small openings between the vertebrae known as the intervertebral foramina. These intervertebral foramina provide a pathway for the nerve to travel outside the spinal column and into the surrounding tissues.
As the sciatic nerve leaves the lumbar sacral spine, it enters the buttock region and passes through a group of muscles known as the piriformis muscle. This muscle can sometimes cause compression or irritation of the sciatic nerve, leading to a condition called piriformis syndrome. In piriformis syndrome, the muscle spasms or tightens, putting pressure on the nerve and causing pain and discomfort.
From the buttocks, the sciatic nerve continues its journey down the back of the leg, branching out to provide innervation to various muscles and relay sensory information to the brain. It is the longest and thickest nerve in the human body, and its extensive distribution allows for the transmission of signals between the lower body and the central nervous system.
Due to its intricate path and exposure to potential compression or irritation, the sciatic nerve is susceptible to injury or inflammation, leading to sciatic nerve pain and associated symptoms such as numbness, tingling, or weakness in the lower back, buttocks, and legs.
Understanding Sciatic Nerve Pain
Sciatic nerve pain, also referred to as sciatica, is a common condition caused by the compression or irritation of the sciatic nerve. While it can occur due to various factors, such as spinal stenosis or a herniated disc, the lumbar sacral spine is often a key area of focus for diagnosis and treatment.
Spinal stenosis is a condition characterized by the narrowing of the spinal canal, which can put pressure on the sciatic nerve as it passes through the lumbar sacral spine. This narrowing can be caused by age-related changes, such as the thickening of ligaments or the formation of bone spurs, or by conditions like arthritis or degenerative disc disease.
A herniated disc, on the other hand, occurs when the soft inner core of a spinal disc protrudes through the outer layer and presses against the sciatic nerve. This can happen as a result of injury, wear and tear, or degenerative changes in the spine.
The symptoms of sciatic nerve pain can range from mild discomfort to severe, debilitating pain that affects daily activities and quality of life. In addition to pain, individuals may experience numbness, tingling, or weakness in the lower back, buttocks, and legs. These symptoms can be aggravated by certain activities, such as sitting for long periods, bending, or lifting heavy objects.
If you experience symptoms of sciatic nerve pain, it is important to consult with a medical professional to determine the underlying cause and develop an appropriate treatment plan. While some cases may resolve with conservative measures, such as rest, physical therapy, and pain medication, others may require more intensive interventions, including epidural steroid injections or surgery.
In conclusion, the lumbar sacral spine and the sciatic nerve are intricately connected. Understanding the path of the sciatic nerve through the lumbar sacral spine and the potential causes of sciatic nerve pain can help in diagnosing and managing this common condition.
Common Conditions Affecting the Lumbar Sacral Spine
Several conditions can affect the lumbar sacral spine and contribute to sciatic nerve pain. Understanding these conditions can provide insights into the nature of lumbar sacral spine health and the importance of timely intervention.
Lumbar Spinal Stenosis and Sciatica
Lumbar spinal stenosis occurs when the spinal canal narrows, putting pressure on the spinal cord and nerve roots. This narrowing can be caused by various factors, such as age-related degeneration, bone spurs, or herniated discs. When the sciatic nerve is affected, it can result in the development of sciatic nerve pain.
Sciatica caused by lumbar spinal stenosis often presents with symptoms such as leg pain, numbness, and weakness. The pain may radiate from the lower back down to the buttocks and legs, making it difficult for individuals to perform everyday activities.
Fortunately, there are several treatment options available for lumbar spinal stenosis and its associated sciatica. Physical therapy can help strengthen the muscles supporting the spine and improve flexibility. Pain medication, such as nonsteroidal anti-inflammatory drugs (NSAIDs), may be prescribed to alleviate discomfort. In severe cases where conservative treatments fail to provide relief, surgery may be considered to decompress the affected nerves and alleviate symptoms.
Lumbar Herniated Disc and Its Impact
A lumbar herniated disc, also known as a slipped or ruptured disc, occurs when the soft gel-like inner core of an intervertebral disc leaks out through a tear in the annulus fibrosus. This can happen due to age-related wear and tear, trauma, or repetitive strain on the spine. When a herniated disc affects the lumbar region, it can cause compression of the adjacent nerve roots, including the sciatic nerve, leading to sciatica.
Individuals with a lumbar herniated disc may experience a range of symptoms, including lower back pain, leg pain, tingling, and muscle weakness. The severity of symptoms can vary depending on the location and size of the herniation.
Treatment options for a lumbar herniated disc and its impact on sciatica may involve a combination of rest, physical therapy, and pain management techniques. Resting and avoiding activities that exacerbate the symptoms can help reduce inflammation and promote healing. Physical therapy exercises can strengthen the surrounding muscles, improve posture, and alleviate pressure on the affected nerves. Pain management techniques, such as hot or cold therapy, epidural steroid injections, or oral medications, may be recommended to manage pain and inflammation. In some cases, when conservative treatments fail to provide relief or if there are severe neurological symptoms, surgical intervention may be necessary to remove or repair the herniated disc.
By understanding the causes and effects of lumbar spinal stenosis and lumbar herniated discs, individuals can make informed decisions about their treatment options. Early intervention and appropriate management can help alleviate symptoms, improve quality of life, and prevent further complications.
Diagnosis and Treatment of Lumbar Sacral Spine Conditions
Accurate diagnosis of lumbar sacral spine conditions is crucial for determining appropriate treatment strategies. Various diagnostic techniques may be employed to evaluate the structure and function of the lumbar sacral spine, including imaging studies, such as X-rays, MRI scans, or CT scans.
When it comes to diagnosing lumbar sacral spine conditions, medical professionals have a range of tools at their disposal. X-rays are often the first imaging technique used, as they can provide a clear picture of the bones in the spine. However, X-rays may not always reveal the full extent of the problem, especially when it comes to soft tissue injuries or nerve compression.
In cases where X-rays do not provide enough information, MRI scans or CT scans may be ordered. These imaging techniques can provide detailed images of the soft tissues, including the spinal discs, nerves, and surrounding structures. MRI scans use magnetic fields and radio waves to create images, while CT scans use X-rays and a computer to generate cross-sectional images of the spine.
Diagnostic Techniques for Lumbar Sacral Spine Conditions
In addition to imaging studies, medical professionals may also perform physical examinations, evaluate medical history, and use diagnostic injections to confirm the source of pain. Physical examinations can involve assessing the patient’s range of motion, muscle strength, and reflexes. These examinations help doctors identify any abnormalities or areas of concern.
Medical history is another important aspect of the diagnostic process. Understanding a patient’s past medical conditions, previous injuries, and family history can provide valuable insights into the potential causes of their lumbar sacral spine condition. This information can help guide the diagnostic process and inform treatment decisions.
Diagnostic injections, such as nerve blocks or facet joint injections, can be used to determine the source of pain. These injections involve injecting a local anesthetic or anti-inflammatory medication into specific areas of the spine. If the injection provides temporary pain relief, it suggests that the injected area is the source of the pain.
By combining the information gathered from imaging studies, physical examinations, medical history, and diagnostic injections, medical professionals can develop a comprehensive understanding of the patient’s condition. This holistic approach to diagnosis ensures that the treatment plan is tailored to the individual’s specific needs.
Non-Surgical Treatment Options for Sciatic Nerve Pain
For many individuals experiencing sciatic nerve pain, non-surgical treatment options may provide relief. These may include physical therapy, stretches and exercises to strengthen the core and improve flexibility, pain medication, heat or cold therapy, and lifestyle modifications.
Physical therapy is a common non-surgical treatment option for sciatic nerve pain. A physical therapist can design a personalized exercise program to target the underlying causes of the pain and improve overall spinal health. These exercises may include stretching, strengthening, and low-impact aerobic activities.
In addition to physical therapy, pain medication can help manage the symptoms of sciatic nerve pain. Nonsteroidal anti-inflammatory drugs (NSAIDs) can reduce inflammation and alleviate pain, while muscle relaxants can help ease muscle spasms. However, it is important to note that pain medication should be used under the guidance of a healthcare professional and for short-term relief.
Heat or cold therapy can also provide temporary relief for sciatic nerve pain. Applying a heating pad or hot pack to the affected area can help relax muscles and increase blood flow, while cold therapy, such as ice packs, can reduce inflammation and numb the area. Alternating between heat and cold therapy may provide additional benefits.
Lastly, lifestyle modifications can play a significant role in managing sciatic nerve pain. Maintaining a healthy weight, practicing good posture, and avoiding activities that exacerbate the pain can all contribute to long-term pain relief. Additionally, stress management techniques, such as meditation or yoga, can help reduce tension and promote overall well-being.
It is important to note that each case is unique, and treatment plans should be tailored to the individual’s specific needs. Consulting with a healthcare professional is always recommended to ensure the most appropriate course of action.
Surgical Interventions for Severe Cases
In cases where conservative measures are ineffective or if there is significant nerve compression, surgical intervention may be necessary. Surgical procedures may involve removing the source of compression, such as a herniated disc or bone spur, or creating more space for the nerve roots. It is essential to consult with a qualified surgeon to discuss the potential risks and benefits associated with surgery.
Surgery for lumbar sacral spine conditions is typically considered a last resort when all other treatment options have been exhausted. However, for individuals with severe pain or progressive neurological symptoms, surgery can provide significant relief and improve quality of life.
There are different surgical approaches depending on the specific condition and the patient’s needs. For example, a discectomy may be performed to remove a herniated disc that is pressing on a nerve root. In more complex cases, spinal fusion surgery may be necessary to stabilize the spine and alleviate pain.
Before undergoing surgery, patients will undergo a thorough evaluation to ensure they are suitable candidates. This evaluation may include additional imaging studies, such as a discogram or a myelogram, to further assess the condition of the spine. The surgeon will discuss the potential risks and benefits of the procedure, as well as the expected recovery process.
Post-surgical rehabilitation is an essential part of the recovery process. Physical therapy and rehabilitation exercises are typically prescribed to help restore strength, flexibility, and mobility. Following the surgeon’s instructions and attending follow-up appointments are crucial for a successful recovery.
In conclusion, accurate diagnosis is crucial for determining appropriate treatment strategies for lumbar sacral spine conditions. Diagnostic techniques, such as imaging studies, physical examinations, medical history evaluations, and diagnostic injections, help medical professionals develop personalized treatment plans. Non-surgical options, such as physical therapy, pain medication, heat or cold therapy, and lifestyle modifications, can provide relief for sciatic nerve pain. In severe cases, surgical interventions may be necessary to address the underlying cause of the condition. Consulting with a healthcare professional is always recommended to ensure the most appropriate course of action.
Prevention and Management of Lumbar Sacral Spine Health
Preventing and managing lumbar sacral spine conditions are essential for maintaining overall spinal health. While it may not be possible to completely eliminate the risk of developing these conditions, incorporating certain lifestyle changes and habits can significantly reduce the likelihood and severity of symptoms.
Lifestyle Changes for a Healthy Spine
Engaging in regular physical activity, maintaining proper posture, and avoiding prolonged sitting or standing can help improve the health of the lumbar sacral spine. Additionally, maintaining a healthy weight, avoiding tobacco use, and practicing stress reduction techniques may further contribute to overall spinal health.
Exercises to Strengthen the Lumbar Sacral Spine
Performing targeted exercises to strengthen the core muscles and improve flexibility can help support the lumbar sacral spine and reduce the risk of injury. Consultation with a physical therapist or fitness professional is recommended to ensure proper technique and an individualized exercise program.
Importance of Regular Check-ups and Early Diagnosis
Regular check-ups with a healthcare professional play a crucial role in the early diagnosis and management of lumbar sacral spine conditions. Early intervention can provide optimal outcomes and help prevent the progression of symptoms or complications. If you experience any persistent discomfort or noticeable changes in your lower back or lower extremities, seek medical attention promptly.
In conclusion, understanding the lumbar sacral spine and its relationship to sciatic nerve pain is essential for effective diagnosis and treatment. By comprehending the anatomy, common conditions, diagnostic techniques, and treatment options associated with the lumbar sacral spine, individuals can take proactive steps to maintain spinal health and seek appropriate medical care when necessary. Remember, consulting with a healthcare professional is crucial for tailored guidance and comprehensive management of any spine-related concerns.