The Nerves Included in the Sacral Plexus
The sacral plexus is a crucial network of nerves located in the pelvic region, contributing to the proper functioning of the lower limbs and pelvic organs. Understanding the intricacies of this plexus and its associated nerves is essential for comprehending various disorders and potential treatment options. In this comprehensive article, we will delve into the depths of the sacral plexus, examining its definition, function, anatomy, major nerves, role in the nervous system, associated disorders, and future research and developments.
Understanding the Sacral Plexus
Definition and Function of the Sacral Plexus
First and foremost, let’s define the sacral plexus. It is a complex web of nerves that arises from the anterior rami of spinal nerves L4 to S4. Situated within the pelvis, this network primarily serves the lower extremities and pelvic organs, playing a vital role in motor and sensory functions.
The sacral plexus is a fascinating structure that deserves a closer look. It is not just a simple collection of nerves; rather, it is a highly organized network that allows for the transmission of signals between the brain and various parts of the body. This intricate system ensures that our lower extremities and pelvic organs function properly, enabling us to walk, run, and perform various activities of daily living.
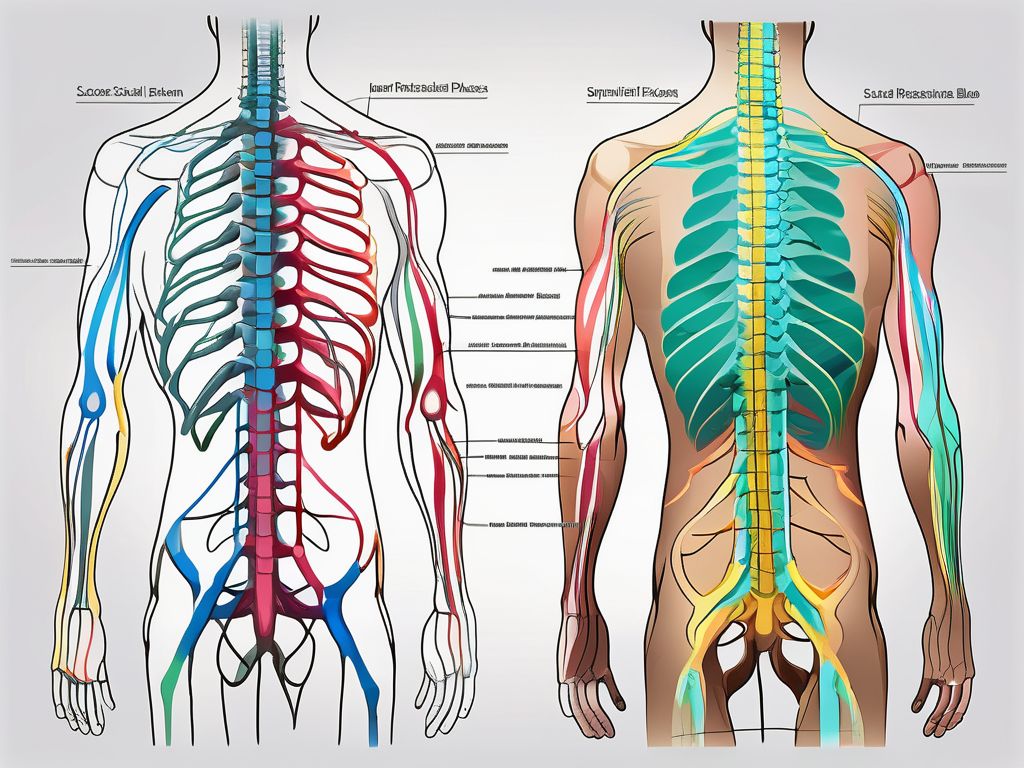
Anatomy of the Sacral Plexus
The sacral plexus is formed by the anterior divisions of spinal nerves, which combine to produce a tangled meshwork of nerves. This intricate arrangement of nerves allows for the efficient distribution of signals throughout the lower body. It is truly remarkable how the body has evolved to create such a complex network, ensuring the smooth functioning of our lower extremities and pelvic organs.
One of the main branches of the sacral plexus is the sciatic nerve. This nerve is the largest and longest nerve in the body, extending from the lower back down to the foot. It is responsible for transmitting signals that allow us to move and feel sensations in our legs and feet. Without the sciatic nerve, simple tasks like walking or even standing would be impossible.
Another important branch of the sacral plexus is the pudendal nerve. This nerve plays a crucial role in controlling the muscles of the pelvic floor, including those involved in urination and bowel movements. It also provides sensation to the genital area, ensuring proper sexual function and pleasure.
In addition to the sciatic and pudendal nerves, the sacral plexus gives rise to other branches such as the superior gluteal nerve. This nerve innervates the gluteus medius, gluteus minimus, and tensor fasciae latae muscles, which are essential for maintaining stability and balance while walking or running.
Understanding the intricate pathways and connections present within this plexus is crucial for comprehending its functions and related disorders. By studying the anatomy of the sacral plexus, healthcare professionals can better diagnose and treat conditions that affect this vital network of nerves.
The Major Nerves of the Sacral Plexus
The sacral plexus is a complex network of nerves located in the lower back region. It is responsible for innervating various muscles and providing sensory function to the lower extremities. Among the nerves originating from the sacral plexus, three major nerves stand out: the sciatic nerve, the pudendal nerve, and the superior gluteal nerve.
Sciatic Nerve
The sciatic nerve, one of the most substantial nerves in the human body, emerges from the sacral plexus and traverses down the posterior thigh. It is the longest and thickest nerve in the body, extending from the lower back all the way down to the foot. The sciatic nerve plays a crucial role in the movement and sensation of the lower leg.
As the sciatic nerve travels down the leg, it branches out into smaller nerves that innervate the muscles of the calf, ankle, and foot. These muscles are responsible for essential movements such as walking, running, and maintaining balance. Additionally, the sciatic nerve carries sensory information from the leg and foot back to the brain, allowing us to perceive touch, temperature, and pain in these areas.
In cases of sciatic nerve impingement or injury, individuals may experience pain, numbness, or weakness along the course of the nerve. This condition, known as sciatica, can be caused by various factors such as herniated discs, spinal stenosis, or muscle imbalances. Consulting a medical professional is essential for accurate diagnosis and appropriate treatment.
Pudendal Nerve
Next, the pudendal nerve, deriving its roots from the sacral plexus, plays a crucial role in controlling the perineal region. This region includes the external genitalia, anal sphincter, and muscles of the pelvic floor. The pudendal nerve is responsible for providing motor function and sensation to these areas.
The muscles innervated by the pudendal nerve are vital for various bodily functions, including bowel and bladder control, sexual function, and childbirth. Any disruption to the pudendal nerve due to trauma or compression can lead to pelvic pain, incontinence, or sexual dysfunction. Seeking expert medical advice is vital for individuals experiencing such symptoms, as proper diagnosis and treatment can significantly improve their quality of life.
Superior Gluteal Nerve
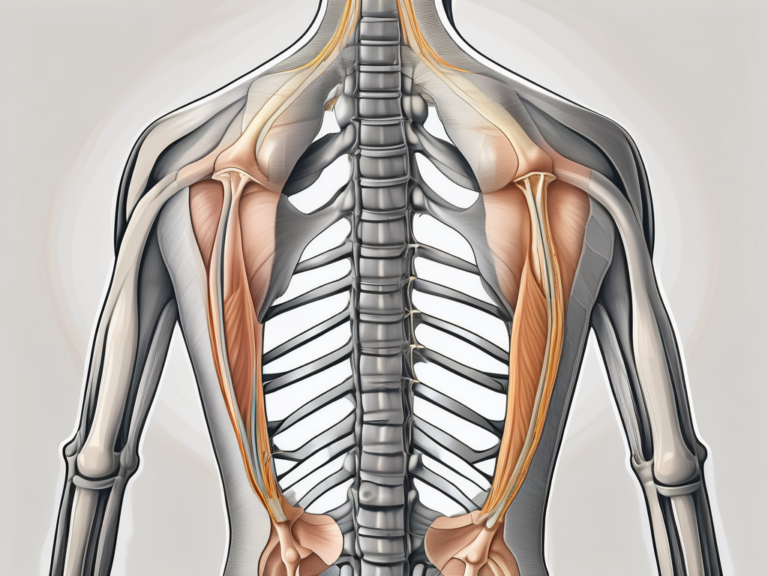
Another important nerve originating from the sacral plexus is the superior gluteal nerve. This nerve supplies the gluteus medius, gluteus minimus, and tensor fasciae latae muscles, which are located in the buttocks and upper thigh region. The superior gluteal nerve plays a crucial role in hip stability, gait, and balance.
When the superior gluteal nerve is functioning properly, it allows for smooth and coordinated movements of the hip joint. It enables us to walk, run, climb stairs, and perform various physical activities with ease. However, injury or dysfunction of the superior gluteal nerve may result in weakness or difficulty in maintaining proper posture and mobility.
Identifying and addressing issues related to the superior gluteal nerve should be done under the guidance of a medical professional. Physical therapy, targeted exercises, and other interventions can help restore proper function and alleviate symptoms associated with nerve dysfunction.
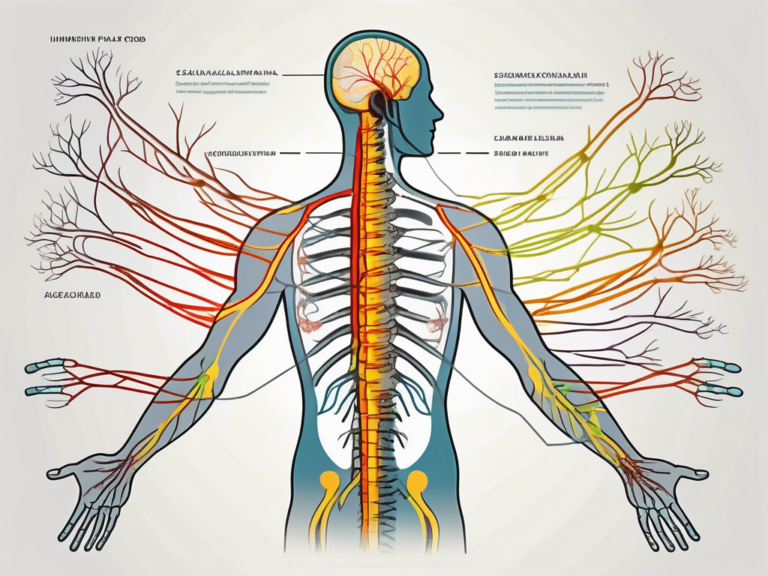
The Role of Sacral Plexus in the Nervous System
Connection with Other Nerves
Within the nervous system, the sacral plexus shares strong connections with other nerve networks, such as the lumbar plexus, lumbar sympathetic chain, and pelvic autonomic nerves. These connections enable coordinated communication and integration of various motor and sensory functions, ensuring smooth operation of the lower limbs and pelvic organs.
The lumbar plexus, located above the sacral plexus, is responsible for innervating the muscles and skin of the lower back, abdomen, and parts of the lower limbs. It works in conjunction with the sacral plexus to provide comprehensive motor and sensory control over the pelvic region and lower extremities. The lumbar sympathetic chain, on the other hand, regulates the involuntary functions of the lower limbs, such as blood vessel constriction and dilation.
Additionally, the sacral plexus connects with the pelvic autonomic nerves, which are responsible for controlling the smooth muscles of the pelvic organs, including the bladder, rectum, and reproductive organs. This intricate network of nerves ensures that the functions of the lower limbs and pelvic organs are well-coordinated, allowing for efficient movement and optimal organ performance.
Impact on Motor and Sensory Functions
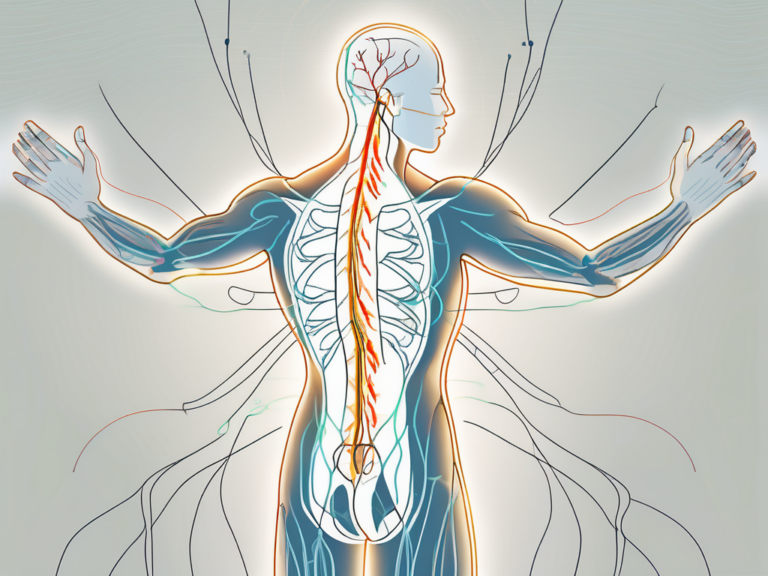
The sacral plexus plays an integral role in both motor and sensory functions. Motor signals stemming from the brain travel through the sacral plexus to innervate muscles, facilitating movement and maintaining balance. The plexus contains motor fibers that control the muscles of the hips, buttocks, thighs, and lower legs. These muscles work together to enable various movements, such as walking, running, and jumping.
Simultaneously, the sacral plexus carries sensory information from the lower limbs and pelvic organs, allowing us to perceive touch, temperature, and pain. Sensory fibers within the plexus transmit signals from the skin, joints, and organs back to the brain, providing us with a sense of our body’s position, detecting potential threats, and allowing us to respond appropriately.
For example, when walking barefoot on a hot surface, sensory receptors in the skin of the feet detect the elevated temperature. The sensory information is then transmitted through the sacral plexus to the brain, which interprets the sensation as pain and triggers a reflex action to withdraw the foot from the heat source. This rapid communication between the sacral plexus and the brain is crucial for our survival and well-being.
Dysfunction of the sacral plexus can disrupt these essential functions, leading to movement impairments and sensory disturbances. Injuries or diseases affecting the sacral plexus can result in muscle weakness, loss of coordination, and difficulty controlling bowel or bladder function. Sensory deficits, such as numbness or tingling in the lower limbs, may also occur.
It is important to recognize the significance of the sacral plexus in the nervous system and the vital role it plays in motor and sensory functions. Understanding its connections with other nerves and its impact on the lower limbs and pelvic organs can help in diagnosing and treating conditions that affect this crucial network, ultimately improving the quality of life for individuals experiencing sacral plexus dysfunction.
Disorders Associated with the Sacral Plexus
The sacral plexus is a complex network of nerves located in the lower back and pelvis region. It plays a crucial role in transmitting signals between the spinal cord and the lower extremities, including the hips, thighs, and lower legs. Disorders associated with the sacral plexus can have a significant impact on a person’s mobility and overall quality of life.
One common cause of sacral plexus injuries is trauma, such as a car accident or a fall. The forceful impact can damage the nerves, leading to pain, weakness, and altered sensation in the affected areas. Compression of the sacral plexus can also occur due to prolonged pressure on the lower back, such as sitting for extended periods or wearing tight clothing. Additionally, nerve entrapment, where a nerve becomes trapped or compressed by surrounding tissues, can contribute to sacral plexus disorders.
Causes and Symptoms of Sacral Plexus Injuries
Sacral plexus injuries can occur due to various factors, including trauma, compression, or nerve entrapment. Symptoms of these injuries may include pain, weakness, altered sensation, and difficulties with movement. Prompt medical evaluation is crucial for accurate diagnosis and formulating an appropriate treatment plan.
When the sacral plexus is injured, individuals may experience radiating pain that extends from the lower back down to the legs. This pain can be sharp, shooting, or dull and may worsen with certain movements or activities. Weakness in the affected muscles can make it challenging to perform simple tasks like walking or standing up from a seated position. Altered sensation, such as numbness or tingling, may also be present, indicating nerve damage. These symptoms can significantly impact a person’s daily life, making it essential to seek medical attention for proper diagnosis and treatment.
Treatment and Rehabilitation Options for Sacral Plexus Disorders
The treatment and rehabilitation of sacral plexus disorders depend on the underlying cause and severity of the condition. Medical professionals may employ a range of approaches, including physical therapy, medication, and, in severe cases, surgical interventions. It is vital to consult with a healthcare provider experienced in treating neurological conditions to develop an individualized care plan tailored to each patient’s needs.
Physical therapy plays a crucial role in the recovery process for individuals with sacral plexus injuries. Therapists can design specific exercises and stretches to strengthen the affected muscles, improve range of motion, and alleviate pain. They may also incorporate modalities such as heat or cold therapy, electrical stimulation, or ultrasound to promote healing and reduce inflammation.
In some cases, medication may be prescribed to manage pain and inflammation associated with sacral plexus disorders. Nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce pain and swelling, while muscle relaxants may be used to alleviate muscle spasms. In more severe cases, surgical intervention may be necessary to repair damaged nerves or release trapped nerves, providing relief and restoring function.
Rehabilitation for sacral plexus disorders is a comprehensive process that focuses on improving overall function and quality of life. It may involve ongoing physical therapy, occupational therapy, and psychological support to address any emotional or psychological challenges that may arise. The goal of rehabilitation is to help individuals regain independence, manage pain, and optimize their ability to perform daily activities.
In conclusion, disorders associated with the sacral plexus can have a significant impact on an individual’s well-being. Prompt diagnosis and appropriate treatment are essential for managing symptoms, promoting healing, and improving overall quality of life. By working closely with healthcare professionals and following a comprehensive care plan, individuals with sacral plexus disorders can regain function and live fulfilling lives.
Future Research and Developments in Sacral Plexus Study
The study of the sacral plexus is an area of ongoing research and development, driven by advancements in medical imaging techniques and the quest for new therapeutic approaches. This article explores some of the exciting developments in these areas.
Advances in Sacral Plexus Imaging Techniques
One of the significant advancements in sacral plexus research is the improvement in imaging techniques. Magnetic resonance imaging (MRI) and ultrasound have revolutionized the visualization of the sacral plexus anatomy and potential nerve abnormalities. These non-invasive imaging modalities provide detailed and accurate information, aiding in the diagnosis and treatment of sacral plexus disorders.
With MRI, healthcare professionals can obtain high-resolution images of the sacral plexus, allowing for a comprehensive assessment of its structure and potential abnormalities. This imaging technique utilizes a powerful magnetic field and radio waves to generate detailed images, enabling clinicians to identify nerve compression, tumors, or other pathologies affecting the sacral plexus.
Ultrasound, on the other hand, offers real-time imaging of the sacral plexus. This technique uses sound waves to create images of the internal structures, providing valuable information about nerve function and potential abnormalities. It is particularly useful in guiding interventions, such as nerve blocks or injections, with precision and accuracy.
Potential Therapeutic Approaches for Sacral Plexus Disorders
Researchers are actively exploring new therapeutic approaches to address sacral plexus disorders. These disorders can cause significant impairments in motor and sensory functions, affecting an individual’s quality of life. The development of innovative drug treatments, nerve regeneration techniques, and targeted interventions offers hope for improved outcomes and symptom management.
Drug treatments are being investigated to alleviate pain and improve nerve function in sacral plexus disorders. Researchers are exploring various pharmacological agents that can target specific mechanisms involved in nerve damage or inflammation. These medications aim to reduce pain, promote nerve regeneration, and restore normal function in the sacral plexus.
Nerve regeneration techniques are also a focus of research. Scientists are exploring different approaches to stimulate nerve regrowth and repair in the sacral plexus. This includes the use of growth factors, stem cells, and tissue engineering strategies to promote nerve regeneration and restore function in individuals with sacral plexus injuries or disorders.
Furthermore, targeted interventions are being developed to improve function and quality of life for individuals affected by sacral plexus disorders. These interventions may involve surgical procedures, such as nerve decompression or nerve transfers, to restore normal nerve function and alleviate symptoms. Additionally, physical therapy and rehabilitation programs are being designed to optimize motor and sensory recovery in individuals with sacral plexus injuries.
In conclusion, the study of the sacral plexus is an exciting and evolving field. Advancements in imaging techniques, such as MRI and ultrasound, have provided detailed visualization of the sacral plexus anatomy and potential nerve abnormalities. Ongoing research aims to develop new therapeutic approaches, including drug treatments, nerve regeneration techniques, and targeted interventions, to improve function and quality of life for individuals affected by sacral plexus disorders. These developments offer hope for future breakthroughs and improved outcomes in this field.
Understanding the intricacies of the sacral plexus, its anatomy, major nerves, role in the nervous system, associated disorders, and potential future developments is essential for healthcare professionals and individuals seeking medical guidance. If you are experiencing any symptoms related to sacral plexus disorders, it is crucial to consult with a qualified healthcare provider to ensure accurate diagnosis and appropriate treatment.