What Nerve Emerges from the Sacral Plexus?
The sacral plexus is an intricate network of nerves located in the pelvic region of the body. It plays a vital role in transmitting signals between the spinal cord and lower extremities. Within this vast network of nerves, there is a specific nerve that emerges, commanding attention due to its significance and impact on our daily lives. This nerve is none other than the sciatic nerve.
Understanding the Sacral Plexus
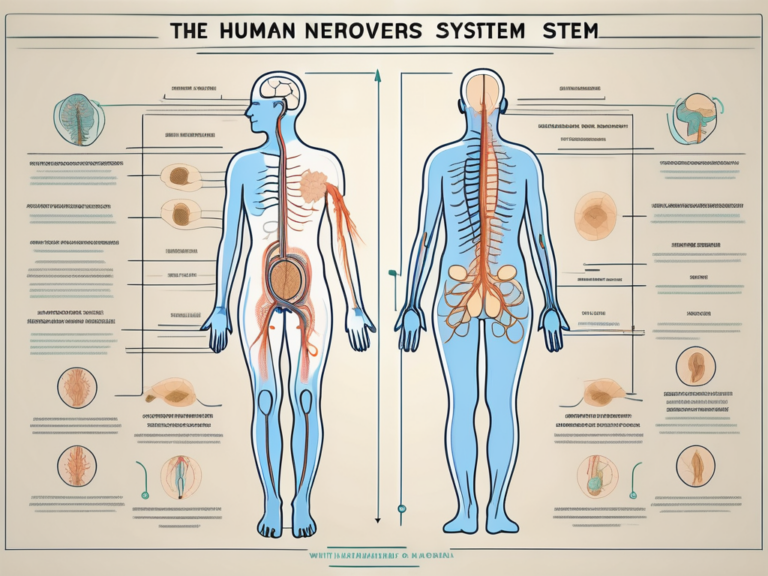
Before diving into the specifics of the nerve that emerges from the sacral plexus, it is important to have a clear understanding of the complex network itself. The sacral plexus is formed by the fusion of several nerve roots stemming from the spinal cord, specifically the lumbar and sacral regions. It is a critical component of the peripheral nervous system, responsible for transmitting both sensory and motor signals to and from the lower limbs.
The sacral plexus, although often overlooked, is a fascinating structure that plays a vital role in our everyday lives. It is like a well-orchestrated symphony, with each nerve root and fiber working in harmony to ensure the smooth functioning of our lower extremities.
Now, let’s delve deeper into the intricate anatomy of the sacral plexus to gain a comprehensive understanding of its complexity.
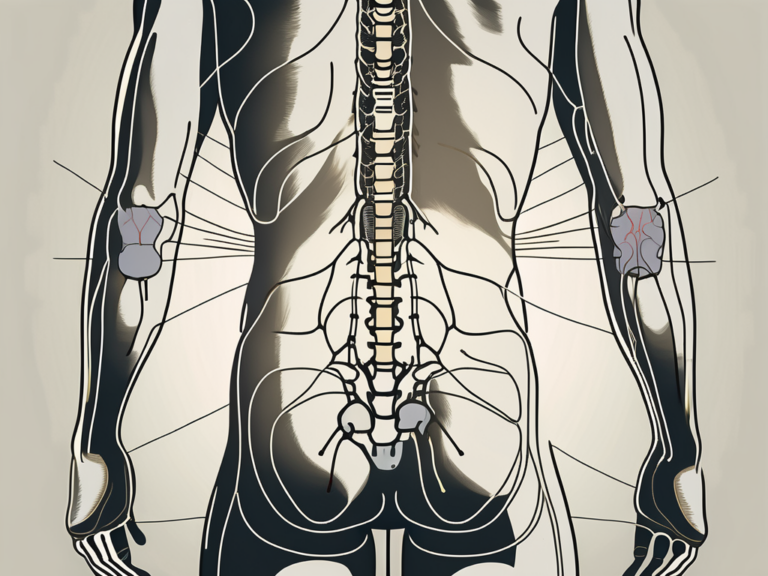
Anatomy of the Sacral Plexus
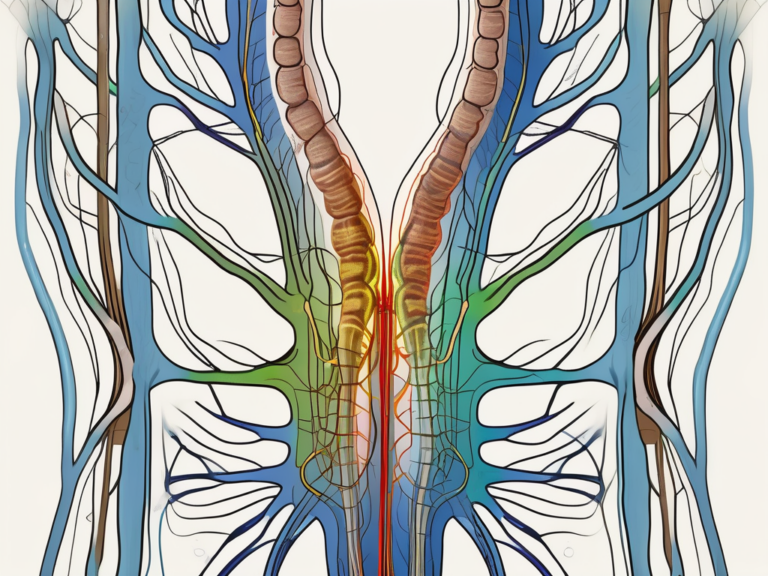
The sacral plexus is composed of nerves originating from the fifth lumbar vertebra (L5) through the first four sacral vertebrae (S1-S4). These nerve roots combine to form a network that eventually gives rise to various individual nerves, including the sciatic nerve.
Imagine the sacral plexus as a magnificent web, intricately woven with nerve fibers that branch out and extend throughout the lower part of our body. These fibers intertwine and connect, forming a network that ensures the efficient transmission of signals between the spinal cord and the lower limbs.
As the nerve roots merge and intertwine within the sacral plexus, they give rise to a multitude of nerves that serve different functions. These nerves branch out like tributaries, supplying the necessary sensory and motor innervation to specific regions of the lower body.
Functions of the Sacral Plexus
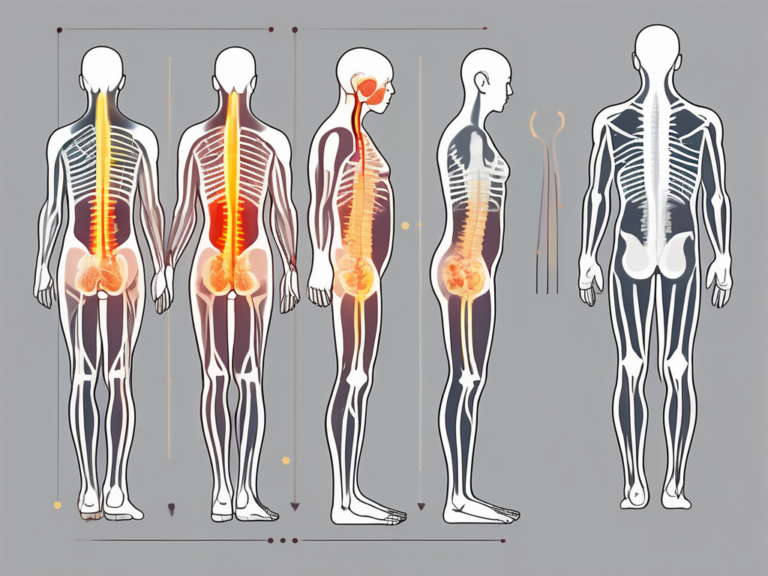
The sacral plexus plays a crucial role in controlling the sensory and motor functions of the lower extremities. It supplies nerves to the buttocks, hips, thighs, and legs, allowing for movement, sensation, and reflexes in these areas. Without the proper functioning of the sacral plexus, simple tasks such as walking, running, or even sitting comfortably can become challenging.
Think about the last time you took a step or felt the warmth of the sun on your legs. All of these experiences are made possible by the intricate network of nerves within the sacral plexus. It is truly remarkable how this complex system coordinates and facilitates our everyday movements, allowing us to navigate the world around us with ease.
Moreover, the sacral plexus is not just responsible for motor control and sensation. It also plays a crucial role in maintaining the body’s homeostasis. The autonomic fibers within the sacral plexus regulate various functions, such as blood flow, digestion, and bladder control, ensuring our body functions smoothly and efficiently.
Understanding the sacral plexus is not only fascinating but also essential in appreciating the intricate workings of our body. It serves as a reminder of the incredible complexity and interconnectedness of our nervous system, highlighting the delicate balance required for optimal functioning.
The Nerve that Emerges from the Sacral Plexus
Among the various nerves that originate from the sacral plexus, the sciatic nerve stands out as the most prominent and influential. It is the longest and thickest nerve in the human body, controlling the majority of motor and sensory functions in the leg and foot.
Identifying the Sciatic Nerve
The sciatic nerve, also known as the ischiadic nerve, emerges from the sacral plexus, specifically from the nerve roots of L4 to S3. It extends down the back of the thigh, branching out to supply the muscles and skin of the entire lower leg, foot, and toes.
As the sciatic nerve travels down the leg, it splits into two main branches known as the tibial nerve and the common fibular (peroneal) nerve. The tibial nerve continues down the back of the leg, supplying the muscles of the calf and the sole of the foot. The common fibular nerve, on the other hand, wraps around the fibular head and divides into the superficial fibular nerve and the deep fibular nerve, which innervate different muscles and areas of the foot.
The sciatic nerve’s path is not only anatomically fascinating but also crucial for our ability to move and sense the world around us. It is responsible for the coordination of various muscle groups, allowing us to walk, run, jump, and perform a wide range of lower limb movements with precision and control.
Role and Functions of the Sciatic Nerve
The sciatic nerve plays a significant role in the lower limb’s functionality, providing both motor and sensory input. It controls the movement of crucial leg muscles such as the hamstrings, quadriceps, and calf muscles. These muscles work together to flex and extend the leg, allowing us to perform activities like walking, climbing stairs, and kicking.
In addition to its motor functions, the sciatic nerve also transmits sensory information from the leg and foot back to the brain. This allows us to perceive touch, pain, and temperature in these areas. Without the sciatic nerve, our ability to feel sensations in the lower limb would be greatly impaired, making it difficult to navigate the world around us and detect potential dangers.
Furthermore, the sciatic nerve is susceptible to compression or injury, leading to a condition known as sciatica. Sciatica is characterized by pain, numbness, and tingling that radiates along the path of the nerve, often extending from the lower back down to the leg and foot. This condition can significantly impact an individual’s quality of life, making it essential to understand the anatomy and functions of the sciatic nerve to prevent and treat such issues.
In conclusion, the sciatic nerve is a vital component of the sacral plexus, responsible for controlling the majority of motor and sensory functions in the leg and foot. Its intricate path and functions make it a fascinating topic of study, highlighting the complexity and beauty of the human body’s neural network.
Connection between Sacral Plexus and Sciatic Nerve
Understanding the relationship between the sacral plexus and the sciatic nerve helps shed light on how this vital nerve emerges and travels throughout the body.
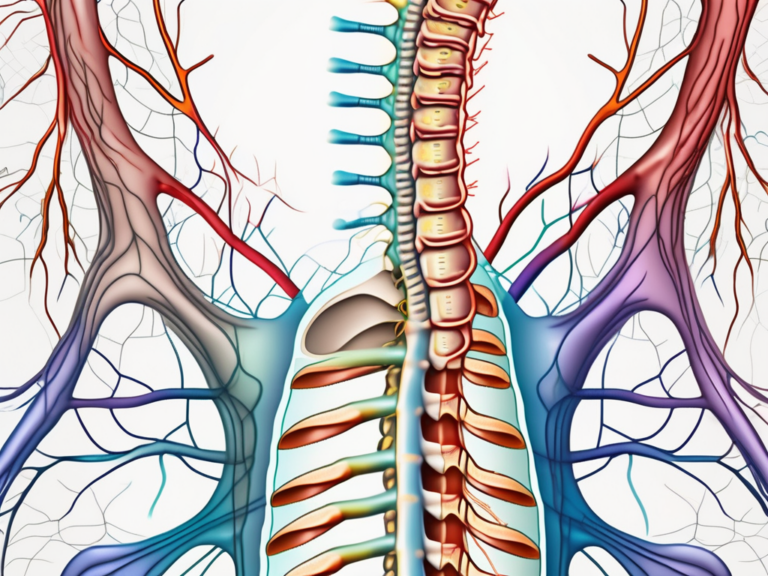
The sacral plexus, a complex network of nerves, plays a crucial role in the innervation of the lower limbs. It is formed by the convergence of nerve roots originating from the lumbar and sacral regions of the spinal cord. Among the nerves that arise from the sacral plexus, the sciatic nerve stands out as the largest and longest nerve in the human body.
How the Sciatic Nerve Originates from the Sacral Plexus
The sciatic nerve originates from a bundle of nerve roots within the sacral plexus. Specifically, the nerve roots of L4 to S3 converge to form the sciatic nerve. This fusion occurs deep within the pelvis, within the greater sciatic foramen, and allows the nerve to extend down the leg.
As the nerve roots join together, they form a thick, rope-like structure that contains both motor and sensory fibers. These fibers play a crucial role in transmitting signals between the brain and the lower extremities, allowing for voluntary movement and sensation.
The Pathway of the Sciatic Nerve
Once the sciatic nerve emerges from the sacral plexus, it travels through the buttock region and then courses down the back of the thigh. As it descends, it continues to branch out, providing innervation to various leg muscles and receiving sensory input from the skin.
The sciatic nerve is responsible for the movement and sensation of the posterior thigh, as well as the entire lower leg and foot. It sends signals to the muscles, enabling actions such as walking, running, and jumping. Additionally, it carries sensory information from the skin, allowing us to perceive touch, temperature, and pain in these regions.
As the sciatic nerve continues its journey, it eventually splits into two main branches, the tibial nerve and the common fibular (peroneal) nerve. These branches further divide into smaller nerves, each with its own specific functions and innervation patterns. The tibial nerve supplies the posterior compartment of the leg, while the common fibular nerve innervates the anterior and lateral compartments.
The tibial nerve travels down the leg and provides motor control to the muscles that flex the knee and extend the ankle and toes. It also carries sensory information from the sole of the foot and the back of the leg.
The common fibular nerve, on the other hand, innervates the muscles that dorsiflex the foot and extend the toes. It also provides sensation to the front of the leg and the top of the foot.
Together, the tibial and common fibular nerves ensure the proper functioning of the lower limb, allowing for a wide range of movements and sensations.
In conclusion, the connection between the sacral plexus and the sciatic nerve is a vital component of the human nervous system. Understanding the origin and pathway of the sciatic nerve provides valuable insights into the complex network of nerves that enable movement and sensation in the lower extremities.
Potential Health Issues Related to the Sacral Plexus and Sciatic Nerve
Unfortunately, the intricate nature of the sacral plexus and the essential role played by the sciatic nerve in our daily lives make them susceptible to various health issues.
The sacral plexus, a network of nerves located in the pelvis, is responsible for innervating the lower extremities. It is a complex structure formed by the merging of the lumbosacral trunk and the sacral nerves. Due to its intricate nature, disorders affecting the sacral plexus can result from trauma, compression, or disease.
One common disorder of the sacral plexus is sacral plexopathy. This condition occurs when there is damage or dysfunction in the sacral plexus, leading to symptoms such as pain, weakness, numbness, or sensation loss in the lower extremities. Sacral radiculopathy, another disorder of the sacral plexus, is characterized by the compression or irritation of the nerve roots that make up the plexus. This can occur due to conditions like herniated discs or spinal stenosis.
Sciatica, a well-known condition, is often associated with disorders of the sacral plexus. It is characterized by pain that radiates along the path of the sciatic nerve, which is the longest nerve in the body. The sciatic nerve originates from the sacral plexus and travels down the back of the leg. Sciatic nerve pain, commonly referred to as sciatica, can be caused by various factors.
Herniated discs, a common cause of sciatic nerve pain, occur when the soft inner material of a spinal disc protrudes through the tough outer layer. This can lead to compression or irritation of the sciatic nerve, resulting in pain, tingling, numbness, or muscle weakness. Another cause of sciatica is spinal stenosis, a condition characterized by the narrowing of the spinal canal. This narrowing can put pressure on the sciatic nerve, causing pain and discomfort.
In addition to structural causes, muscle imbalances can also contribute to sciatic nerve pain. Imbalances in the muscles surrounding the pelvis and lower back can lead to abnormal stress on the sciatic nerve, resulting in pain and other symptoms.
It is important to note that while these conditions can cause significant discomfort and affect daily life, they can often be managed through various treatment options. Physical therapy, medication, and in some cases, surgery, may be recommended to alleviate symptoms and improve overall function.
Treatment and Management of Sacral Plexus and Sciatic Nerve Disorders
When faced with sacral plexus or sciatic nerve disorders, seeking proper medical advice and treatment is crucial. While the severity and specific condition may vary, several approaches can help alleviate symptoms and improve overall well-being.
The sacral plexus and sciatic nerve are intricate parts of the human body’s nervous system, responsible for transmitting signals between the brain and the lower extremities. When these nerves are affected by disorders or injuries, it can lead to debilitating pain, numbness, and loss of mobility.
Non-Surgical Treatment Options
Non-surgical treatment options for sacral plexus and sciatic nerve disorders may include physical therapy, pain medications, and lifestyle modifications. Physical therapy plays a crucial role in the rehabilitation process, helping patients regain strength, flexibility, and range of motion. Skilled therapists employ various techniques such as stretching exercises, manual therapy, and electrical stimulation to stimulate nerve regeneration and improve overall function.
In addition to physical therapy, pain medications may be prescribed to manage acute pain and provide temporary relief. These medications can range from over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) to prescription-strength analgesics. However, it is important to note that pain medications only provide symptomatic relief and do not address the underlying cause of the disorder.
Lifestyle modifications can also play a significant role in managing sacral plexus and sciatic nerve disorders. These modifications may include maintaining a healthy weight, practicing good posture, avoiding prolonged sitting or standing, and engaging in regular low-impact exercises. By adopting these lifestyle changes, individuals can reduce the strain on their nerves and promote overall nerve health.
It is essential to consult with a healthcare professional to determine the most appropriate treatment plan for each individual case. A thorough evaluation, including a comprehensive medical history, physical examination, and diagnostic tests, will help guide the treatment decisions and ensure the best possible outcome.
Surgical Interventions for Severe Cases
In severe cases where conservative treatments fail to provide relief or when the condition significantly affects daily living, surgical intervention may be considered. Surgical procedures aim to alleviate nerve compression or address underlying issues causing the disorder.
One common surgical procedure for sacral plexus and sciatic nerve disorders is a decompression surgery. This procedure involves removing any structures or tissues that are compressing the nerve, such as herniated discs or bone spurs. By relieving the pressure on the nerve, decompression surgery can help restore normal nerve function and alleviate pain.
In some cases, nerve grafting or nerve transfer surgeries may be necessary. These procedures involve taking a healthy nerve from another part of the body and grafting it onto the damaged nerve or transferring a nerve from a less critical muscle to the affected area. These techniques aim to restore nerve continuity and promote nerve regeneration.
However, the decision to undergo surgery should always be made in consultation with a specialist, considering the potential risks and benefits. Surgical interventions carry inherent risks, including infection, bleeding, and nerve damage, and should only be pursued when the potential benefits outweigh the risks.
Overall, the nerve that emerges from the sacral plexus, namely the sciatic nerve, plays a critical role in our daily lives. Its proper functioning is essential for maintaining mobility and sensation in the lower extremities. Understanding the anatomy, functions, and potential health issues related to the sacral plexus and sciatic nerve is crucial for seeking appropriate medical attention and achieving optimal well-being.