How Does Spinal Stenosis Affect the Sacral Nerve?
Spinal stenosis is a condition that can affect various parts of the spine, including the sacral nerve. Understanding how spinal stenosis impacts the sacral nerve is essential for comprehending the symptoms, treatment options, and preventive measures associated with this condition. In this article, we will delve into the intricate details of spinal stenosis and its effect on the sacral nerve, providing you with valuable insights to better understand this complex condition. However, it is crucial to note that this article does not provide medical advice, and if you suspect you may have spinal stenosis or any related symptoms, it is always advisable to consult with a healthcare professional.
Understanding Spinal Stenosis
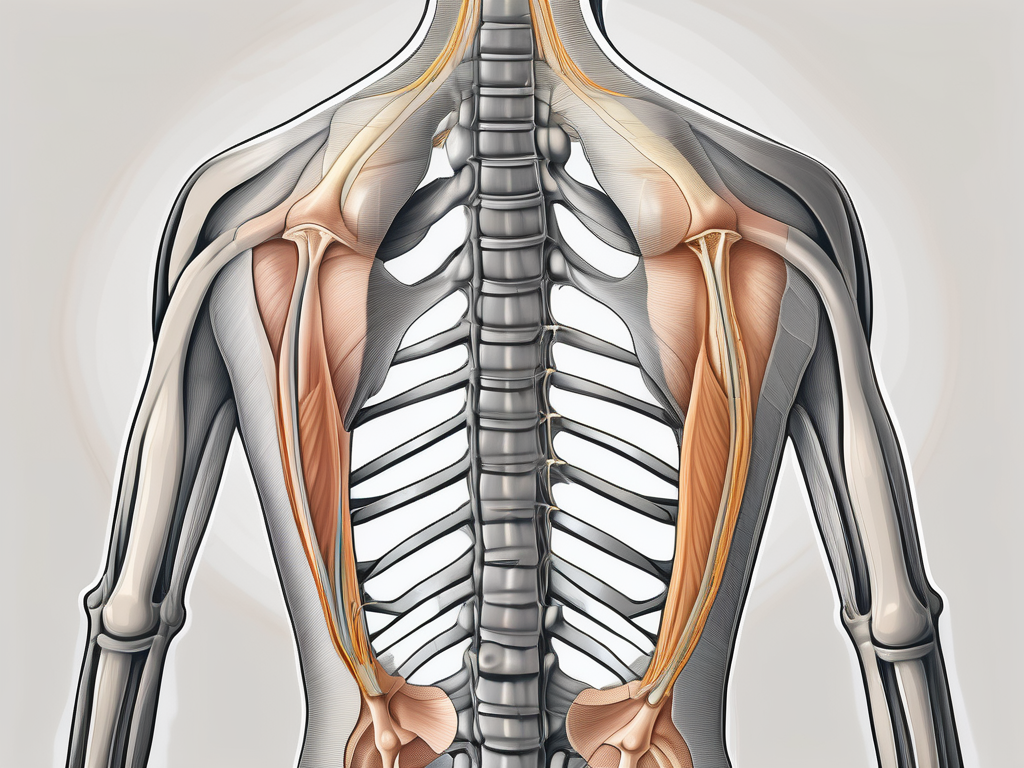
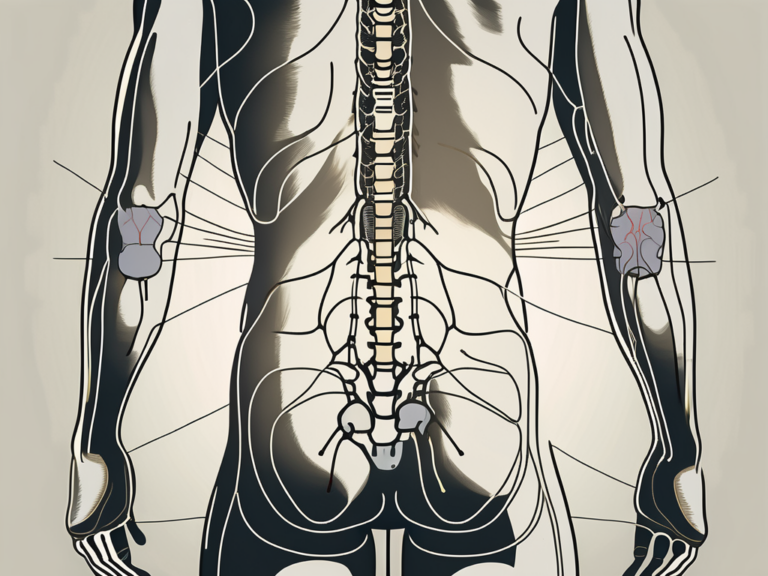
Spinal stenosis is a common condition that affects the spinal canal, causing a narrowing that can lead to pressure on the nerves and surrounding tissues. This narrowing can occur in different regions of the spine, including the cervical, thoracic, and lumbar areas. However, when spinal stenosis affects the lower back and impacts the sacral nerve, it can lead to various complications and discomfort.
Spinal stenosis is often a result of age-related changes in the spine. As we age, the spine undergoes wear and tear, which can lead to conditions such as osteoarthritis, disc degeneration, or the formation of bone spurs. These changes can gradually narrow the spinal canal, causing compression of the nerves and resulting in symptoms of spinal stenosis. While age-related changes are the most common cause of spinal stenosis, there are other less common causes as well. These include congenital disorders, spinal tumors, or spine injuries.
When the spinal canal narrows, it can compress the sacral nerve roots branching out from the lower end of the spinal cord. The sacral nerve plays a crucial role in the functioning of the lower extremities, as well as bowel and bladder control. Therefore, compression of the sacral nerve can lead to a wide range of symptoms.
Symptoms and Diagnosis of Spinal Stenosis
The symptoms of spinal stenosis affecting the sacral nerve can vary depending on the extent of nerve compression. Common symptoms include lower back pain, which can radiate down the legs. This pain is often described as a dull ache or a burning sensation. In addition to pain, individuals may experience numbness or tingling in the legs, weakness in the lower extremities, and difficulty with bowel or bladder control.
Diagnosing spinal stenosis requires a thorough evaluation by a healthcare professional. During a physical examination, the healthcare provider will assess the patient’s range of motion, reflexes, and muscle strength. They will also review the patient’s medical history to identify any risk factors or previous injuries that may contribute to the development of spinal stenosis. In some cases, imaging tests such as X-rays or MRI scans may be ordered to visualize the spinal canal and assess the extent of nerve compression.
It is important to note that while spinal stenosis can cause significant discomfort and limitations in daily activities, there are various treatment options available. These can include conservative measures such as physical therapy, pain management techniques, and lifestyle modifications. In more severe cases, surgical intervention may be necessary to relieve the compression on the nerves and restore normal spinal function.
The Role of the Sacral Nerve
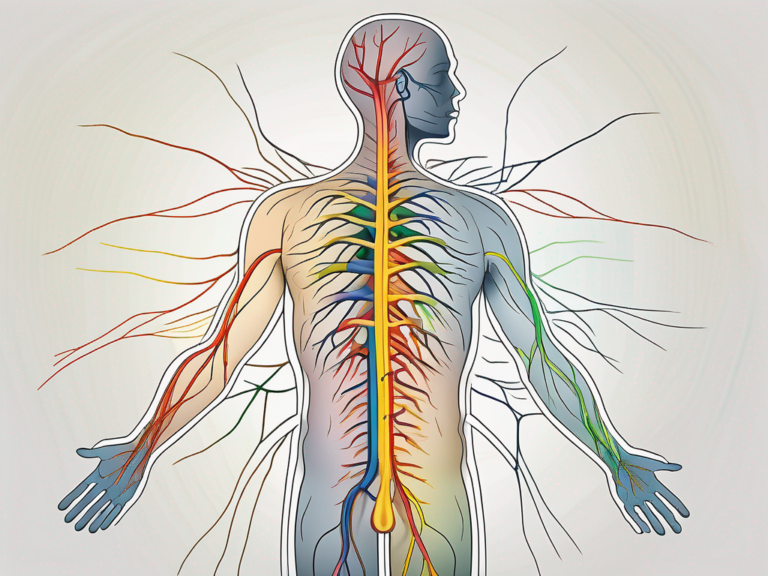
The sacral nerve plays a significant role in controlling various bodily functions. It is responsible for transmitting signals to and from the bladder, bowel, and sexual organs. Additionally, the sacral nerve is involved in the functioning of the pelvic floor muscles and is essential for maintaining balance, stability, and coordination.
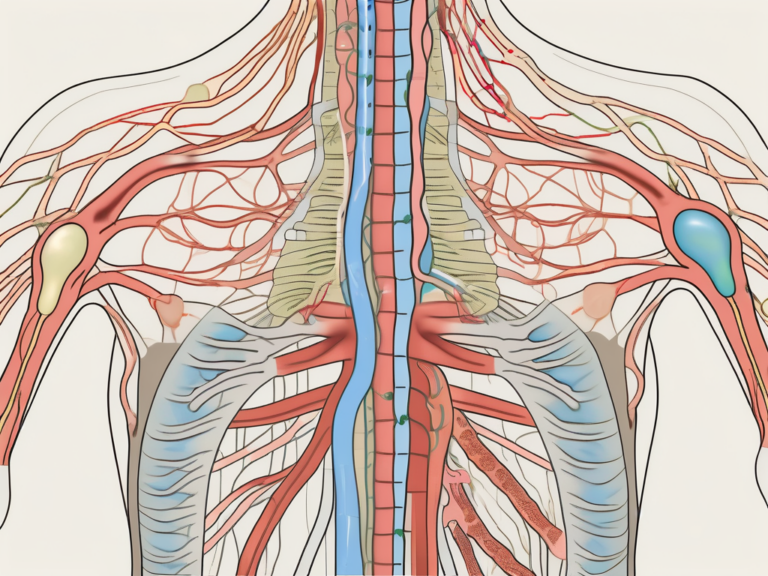
The sacral nerve, also known as the sacral plexus, is a complex network of nerves that originates from the sacral spinal cord and extends down the spinal canal. It is formed by the fusion of the ventral rami of the spinal nerves S1 to S4. These nerves branch out and supply different structures within the pelvis and the lower extremities.
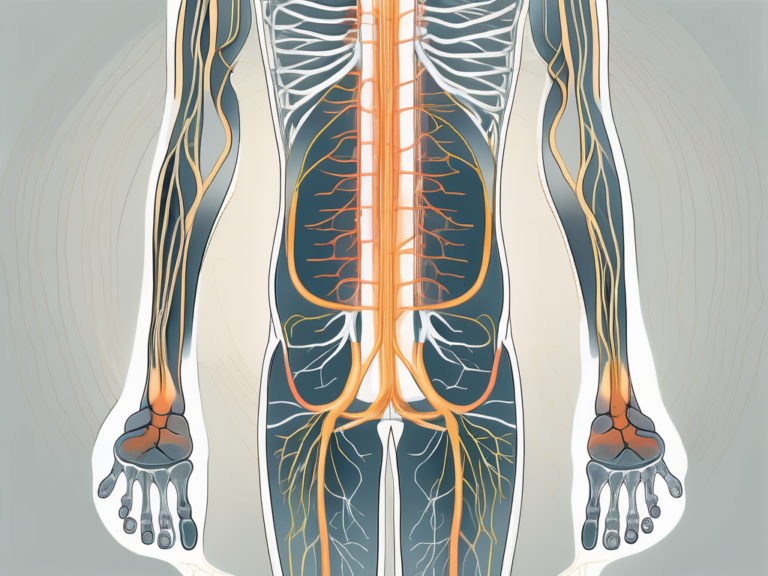
Anatomy of the Sacral Nerve
The sacral nerve is composed of several branches that innervate muscles, organs, and skin regions, allowing for the normal functioning of these areas. These branches include the superior gluteal nerve, inferior gluteal nerve, pudendal nerve, sciatic nerve, posterior femoral cutaneous nerve, and many others.
The superior gluteal nerve supplies the gluteus medius, gluteus minimus, and tensor fasciae latae muscles, which are essential for hip abduction and stabilization. The inferior gluteal nerve innervates the gluteus maximus muscle, responsible for hip extension and external rotation.
The pudendal nerve plays a crucial role in the innervation of the pelvic floor muscles, including the levator ani and coccygeus muscles. These muscles are responsible for supporting the pelvic organs, maintaining continence, and facilitating childbirth.
The sciatic nerve, the largest nerve in the body, originates from the sacral plexus. It extends down the back of the thigh, supplying the hamstrings, adductor magnus, and other muscles involved in leg movement. The sciatic nerve also provides sensory innervation to the skin of the posterior thigh, leg, and foot.
The posterior femoral cutaneous nerve innervates the skin of the posterior thigh and the popliteal fossa, contributing to the sensation in these areas.
Functions of the Sacral Nerve
The sacral nerve plays a vital role in the normal functioning of numerous bodily processes. It aids in the regulation of bladder and bowel movements by controlling the contraction and relaxation of the associated muscles. The coordination of these muscles allows for the proper emptying of the bladder and the elimination of waste from the body.
In addition to its role in bladder and bowel control, the sacral nerve is also involved in sexual function. It plays a crucial role in the process of arousal and orgasm by transmitting signals to the sexual organs and coordinating the necessary muscle contractions.
Furthermore, the sacral nerve contributes to the sensation and control of leg movements. It works in conjunction with other nerves and muscles to allow us to walk, run, and perform various physical activities. Without the proper functioning of the sacral nerve, these movements would be compromised, leading to difficulties in mobility and coordination.
In conclusion, the sacral nerve is a vital component of the nervous system, responsible for controlling various bodily functions. Its intricate anatomy and extensive innervation allow for the normal functioning of the bladder, bowel, sexual organs, and lower extremities. Understanding the role of the sacral nerve is essential in diagnosing and treating conditions that may affect its functioning, ensuring optimal health and well-being.
The Impact of Spinal Stenosis on the Sacral Nerve
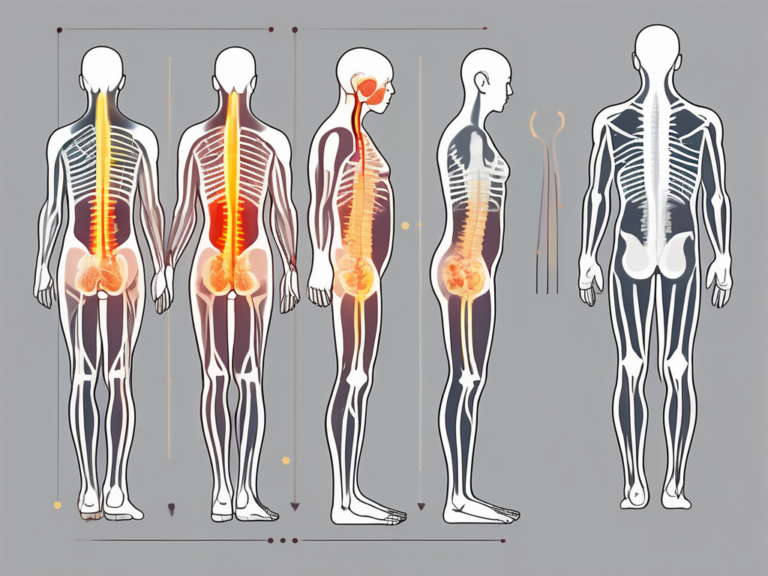
When spinal stenosis affects the sacral nerve, it can lead to several physiological changes and clinical manifestations. These changes can vary from person to person, depending on the severity and location of the nerve compression.
Spinal stenosis is a condition characterized by the narrowing of the spinal canal, which can put pressure on the nerves that pass through it. When this narrowing occurs in the lower part of the spine, specifically affecting the sacral nerve, it can have significant consequences on various bodily functions.
Physiological Changes in the Sacral Nerve
The compression of the sacral nerve roots due to spinal stenosis can disrupt the normal transmission of nerve signals. This disruption can result in a range of physiological changes that can impact an individual’s daily life.
One of the primary effects of sacral nerve compression is altered muscle function. The affected nerve branches innervate the muscles in the pelvic region and lower extremities. When these nerves are compressed, the muscles may not receive proper signals, leading to weakness and decreased control over movements.
In addition to muscle function, the compression of the sacral nerve can also cause decreased sensation in the areas it innervates. This can result in sensory disturbances in the legs and pelvis, such as numbness, tingling, or a loss of feeling. These sensory changes can further affect an individual’s balance and coordination.
Furthermore, impaired motor control is another consequence of sacral nerve compression. The affected nerves play a crucial role in coordinating movements, particularly those related to bladder and bowel control. When the nerve signals are disrupted, individuals may experience difficulties with urinary and fecal continence, leading to significant challenges in daily life.
Moreover, the impact of spinal stenosis on the sacral nerve extends beyond motor and sensory changes. It can also affect sexual function. The nerves in the sacral region are responsible for transmitting sexual sensations and controlling sexual response. When these nerves are compressed, individuals may experience a decrease in sexual desire, erectile dysfunction in men, and difficulties achieving orgasm.
Clinical Manifestations and Complications
The clinical manifestations of spinal stenosis affecting the sacral nerve can significantly impact a person’s quality of life. The combination of altered muscle function, decreased sensation, and impaired motor control can lead to chronic pain, mobility issues, and a loss of independence.
Chronic pain is a common symptom experienced by individuals with spinal stenosis affecting the sacral nerve. The compression of the nerves can cause persistent discomfort in the lower back, buttocks, and legs. This pain can be sharp, shooting, or aching in nature, making it challenging for individuals to engage in daily activities and enjoy a good quality of life.
Mobility issues are another consequence of sacral nerve compression. The weakened muscles and sensory disturbances can affect an individual’s ability to walk, stand, or perform activities that require balance and coordination. This can lead to a decrease in overall mobility and an increased risk of falls and injuries.
Loss of independence is a significant concern for individuals with spinal stenosis affecting the sacral nerve. The difficulties with bladder and bowel control, along with mobility issues, can make individuals reliant on assistance for their daily needs. This loss of independence can have a profound impact on their emotional well-being and overall quality of life.
Additionally, severe cases of spinal stenosis can result in complications such as urinary tract infections, falls, and pressure sores. The inability to empty the bladder fully can increase the risk of urinary tract infections, which can be recurrent and require medical intervention. Mobility issues and a higher likelihood of falls can lead to injuries, fractures, and other related complications. Furthermore, individuals who are unable to change positions frequently due to pain and mobility limitations may develop pressure sores, which can be painful and difficult to heal.
In conclusion, spinal stenosis affecting the sacral nerve can have far-reaching consequences on an individual’s physiological well-being and overall quality of life. The altered muscle function, decreased sensation, and impaired motor control can lead to difficulties with bladder and bowel control, reduced sexual function, muscle weakness, and sensory disturbances. These clinical manifestations, coupled with the potential for complications, highlight the importance of early identification and comprehensive management of spinal stenosis to minimize its impact on individuals’ lives.
Treatment Options for Spinal Stenosis Affecting the Sacral Nerve
Spinal stenosis affecting the sacral nerve can be a debilitating condition, causing pain, numbness, and weakness in the lower back, buttocks, and legs. Fortunately, there are various treatment options available to help individuals manage their symptoms and improve their quality of life.
When it comes to treating spinal stenosis, it is important to consider the severity of symptoms, the extent of nerve compression, and the individual’s overall health condition. This helps determine the most appropriate course of action.
Non-Surgical Treatments
Non-surgical treatments are often the first line of defense for individuals with spinal stenosis affecting the sacral nerve. These treatments aim to relieve pain, improve mobility, and enhance overall function without the need for invasive procedures.
One of the most common non-surgical treatments for spinal stenosis is physical therapy. Physical therapists can design personalized exercise programs that focus on strengthening the muscles surrounding the affected area, improving flexibility, and promoting proper posture. These exercises can help alleviate pain, increase range of motion, and enhance overall mobility.
In addition to physical therapy, pain management techniques can also be employed to provide temporary relief. Medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) or muscle relaxants may be prescribed to help reduce inflammation and alleviate pain. In some cases, epidural steroid injections may be recommended to target the specific area of nerve compression and provide localized pain relief.
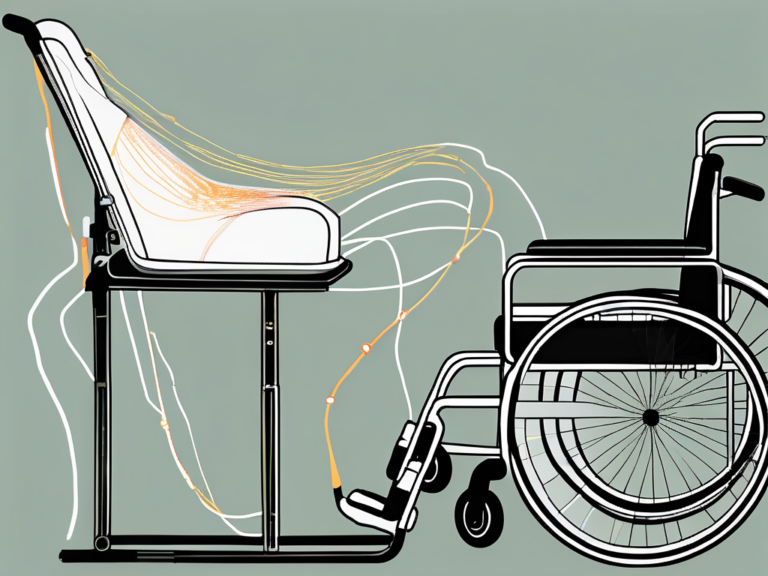
Furthermore, assistive devices like canes or walkers can play a crucial role in managing symptoms and improving stability. These devices help redistribute weight, reduce pressure on the affected nerve, and minimize the risk of falls. Additionally, orthotic devices, such as back braces or shoe inserts, may be recommended to provide additional support and alignment.
Surgical Interventions
While non-surgical treatments are often effective in managing spinal stenosis symptoms, there may be instances where surgical intervention becomes necessary. Surgical options are typically considered for individuals with severe symptoms, significant nerve compression, or when non-surgical treatments have failed to provide adequate relief.
The specific surgical approach for spinal stenosis affecting the sacral nerve depends on the location and severity of the condition. One common surgical procedure is laminectomy, which involves removing a portion of the vertebral bone to create more space for the compressed nerves. This procedure aims to alleviate pressure on the sacral nerve roots and restore normal nerve function.
Another surgical option is foraminotomy, which involves widening the space where the nerves exit the spinal column. By enlarging the foramen, the compressed nerves can be relieved, reducing pain and improving function.
In some cases, spinal fusion may be recommended. Spinal fusion involves fusing two or more vertebrae together, creating a solid bone structure. This procedure aims to stabilize the spine and prevent further compression of the sacral nerve roots.
It is important to note that surgical interventions carry risks and should be thoroughly discussed with a healthcare professional. Factors such as overall health, age, and the presence of other medical conditions should be taken into consideration when determining the most appropriate treatment approach.
In conclusion, treatment options for spinal stenosis affecting the sacral nerve are varied and depend on the severity of symptoms, the extent of nerve compression, and the individual’s overall health condition. Non-surgical treatments, such as physical therapy, pain management techniques, and assistive devices, can provide relief and improve function. However, in severe cases, surgical interventions like laminectomy, foraminotomy, or spinal fusion may be necessary to alleviate compression and restore normal nerve function. Consulting with a healthcare professional is essential in determining the best course of action for each individual.
Prevention and Management of Spinal Stenosis
While it may not be possible to prevent spinal stenosis entirely, certain measures can help reduce the risk of developing or worsening the condition.
Lifestyle Modifications
Engaging in regular physical activity, maintaining a healthy weight, and practicing good posture are essential lifestyle modifications that can promote spinal health and reduce the likelihood of spinal stenosis development or progression. Additionally, smoking cessation and avoiding excessive alcohol consumption can contribute to overall spinal well-being.
Regular Check-ups and Early Detection
Regular check-ups with a healthcare professional, particularly in individuals with a family history of spinal stenosis, can aid in early detection and timely management of the condition. Routine screenings and imaging tests can help identify spinal stenosis at an early stage, allowing for early intervention and better treatment outcomes.
In conclusion, spinal stenosis affecting the sacral nerve can have a significant impact on an individual’s well-being. Understanding the intricacies of this condition, such as its definition, causes, symptoms, and treatment options, is crucial for individuals experiencing symptoms or those seeking to prevent its onset. Remember, if you suspect you have spinal stenosis or any related symptoms, consulting with a healthcare professional is advisable to receive an accurate diagnosis and appropriate treatment.