How Long Does It Take to Alleviate Nerve Pain from Sacral Fracture and Pelvic Injury?
Injuries to the sacrum and pelvis can be debilitating and cause significant pain. Understanding the healing process and the timeline for alleviating nerve pain is crucial for those suffering from these types of injuries. In this article, we will explore the anatomy of the sacrum and pelvis, common causes of fractures and injuries, symptoms and diagnosis, the relationship between these injuries and nerve pain, the healing process, pain management strategies, and what to expect during recovery.
Understanding Sacral Fracture and Pelvic Injury
In order to understand how long it takes to alleviate nerve pain from sacral fractures and pelvic injuries, it is important to first grasp the basics of these injuries. The sacrum is a triangular bone located at the base of the spine, between the hip bones. It connects the spine to the pelvis and provides support and stability to the upper body.
There are several common causes of sacral fractures and pelvic injuries, including falls, sports-related accidents, and motor vehicle accidents. These injuries can result in significant trauma to the bones and surrounding tissues.
The Anatomy of the Sacrum and Pelvis
The sacrum is composed of five fused vertebrae, which form a solid structure that supports the weight of the upper body. It connects to the pelvis through the sacroiliac joints, which allow for movement and flexibility in the lower back and hips.
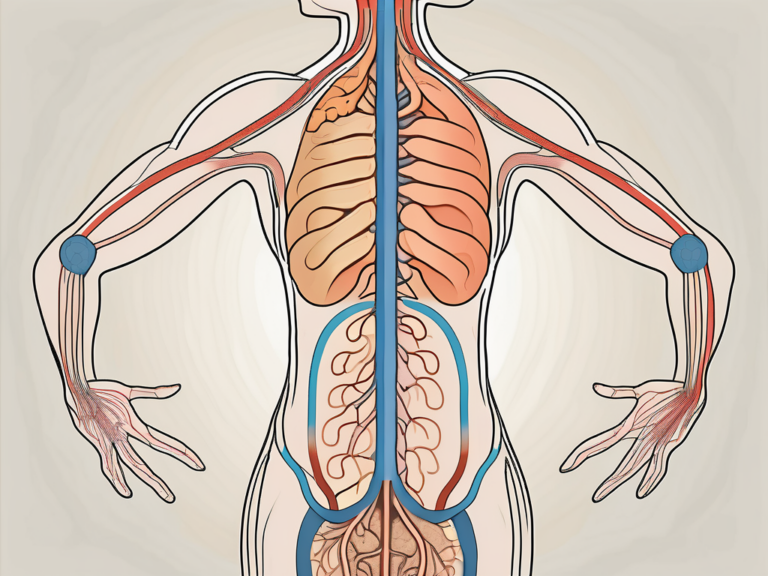
The pelvis consists of the hip bones, the sacrum, and the coccyx. Together, these structures provide support for the organs in the pelvic area and assist in maintaining balance and stability.
The sacrum, being a crucial part of the pelvic girdle, plays a vital role in the transmission of forces between the upper body and the lower limbs. It acts as a strong foundation, distributing the weight evenly and absorbing the impact during various activities such as walking, running, or jumping.
The sacroiliac joints, which connect the sacrum to the hip bones, are responsible for allowing a certain degree of movement in the lower back and hips. This mobility is essential for performing daily activities and maintaining proper posture.
Common Causes of Sacral Fractures and Pelvic Injuries
Sacral fractures and pelvic injuries can occur as a result of various traumatic events. Falls from a significant height, such as from a ladder or a tree, can cause fractures in the sacrum or pelvis. The impact of the fall can exert immense force on the pelvic region, leading to fractures and other associated injuries.
High-impact sports, such as football or skiing, can also lead to these types of injuries. The sudden and forceful movements involved in these sports can put excessive stress on the sacrum and pelvis, potentially resulting in fractures or other forms of damage.
Motor vehicle accidents, particularly those involving a direct impact to the pelvic area, are another common cause of sacral fractures and pelvic injuries. The immense forces generated during a collision can cause severe trauma to the bones and soft tissues in the pelvic region.
It is important to note that certain factors, such as age, osteoporosis, and pre-existing conditions affecting bone strength, can increase the susceptibility to sacral fractures and pelvic injuries.
Symptoms and Diagnosis of Sacral and Pelvic Injuries
The symptoms of sacral fractures and pelvic injuries can vary depending on the severity and location of the injury. Common symptoms include severe pain in the lower back, hips, and buttocks, difficulty walking or standing, bruising or swelling in the pelvic area, and limited range of motion in the hips.
It is crucial to seek medical attention if any of these symptoms are present, as prompt diagnosis and treatment are essential for optimal recovery. A healthcare professional will typically perform a thorough physical examination, reviewing the patient’s medical history, and may order imaging tests such as X-rays or CT scans to assess the extent of the injury.
In some cases, advanced imaging techniques like MRI scans may be required to provide a more detailed view of the sacrum and pelvis, allowing for a more accurate diagnosis. These imaging tests help identify the specific location and severity of the fracture or injury, enabling healthcare providers to develop an appropriate treatment plan.
Additionally, other diagnostic procedures, such as bone scans or blood tests, may be conducted to rule out any underlying conditions or complications associated with the injury.
Overall, understanding the anatomy, common causes, and symptoms of sacral fractures and pelvic injuries is crucial for both healthcare professionals and individuals seeking to gain insights into these conditions. By recognizing the importance of early diagnosis and appropriate treatment, individuals can take proactive steps towards their recovery and overall well-being.
The Relationship Between Sacral Fracture, Pelvic Injury, and Nerve Pain
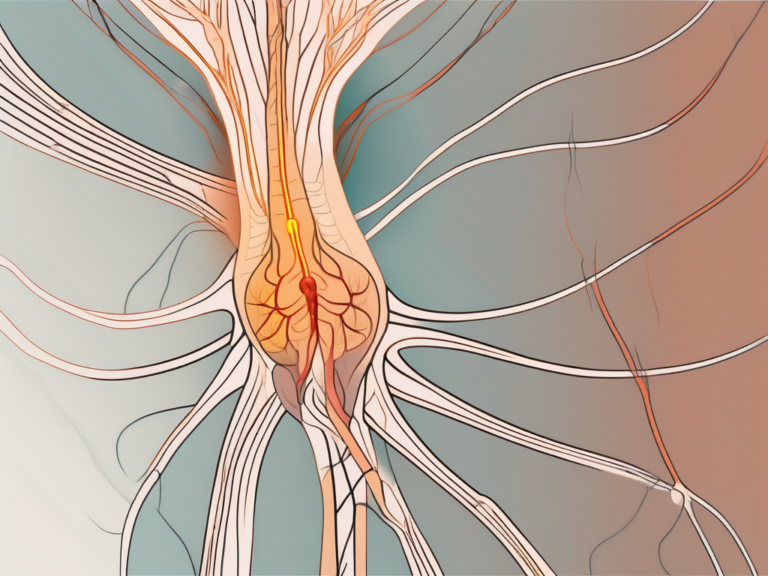
Sacral fractures and pelvic injuries can cause nerve pain due to the proximity of nerves to the affected area. The nervous system plays a crucial role in pain perception, transmitting signals from the injury site to the brain, resulting in the sensation of pain.
How Sacral Fractures and Pelvic Injuries Cause Nerve Pain
When the sacrum or pelvis is injured, the surrounding nerves can become compressed or damaged, leading to pain. The severity and duration of nerve pain can vary depending on the extent of the injury and the individual’s overall health.
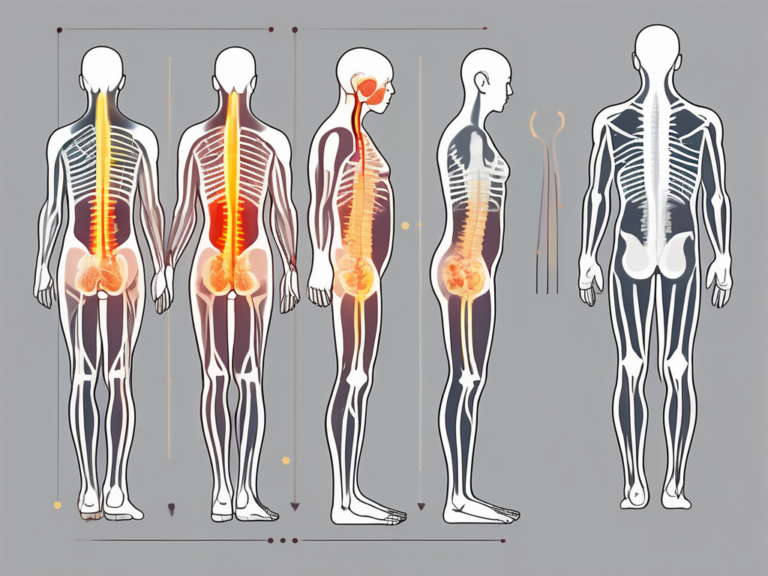
In cases of sacral fractures, the force exerted on the bone can cause it to break or crack. This can result from traumatic events such as falls, motor vehicle accidents, or sports injuries. The sacrum, a triangular bone located at the base of the spine, is an integral part of the pelvic structure. It connects the spine to the pelvis and provides stability and support to the upper body.
When a sacral fracture occurs, the nerves that pass through or near the sacrum can be affected. These nerves are responsible for transmitting sensory information, including pain signals, to the brain. The compression or damage to these nerves can disrupt their normal function, leading to the development of nerve pain.
In the case of pelvic injuries, such as fractures or dislocations, the nerves surrounding the pelvis can also be impacted. The pelvis is a complex structure consisting of multiple bones, including the sacrum, ilium, pubis, and ischium. It serves as a protective enclosure for vital organs, supports the weight of the upper body, and provides attachment points for muscles and ligaments.
When a pelvic injury occurs, the forces involved can cause significant trauma to the surrounding tissues, including the nerves. The nerves in the pelvic region play a crucial role in transmitting signals related to pain, sensation, and motor function. Any disruption or damage to these nerves can result in the development of nerve pain.
It is important to note that not all sacral fractures and pelvic injuries result in nerve pain. Some individuals may experience minimal or no nerve pain, while others may have significant discomfort. Consulting with a healthcare professional is essential for an accurate evaluation of the injury and appropriate treatment recommendations.
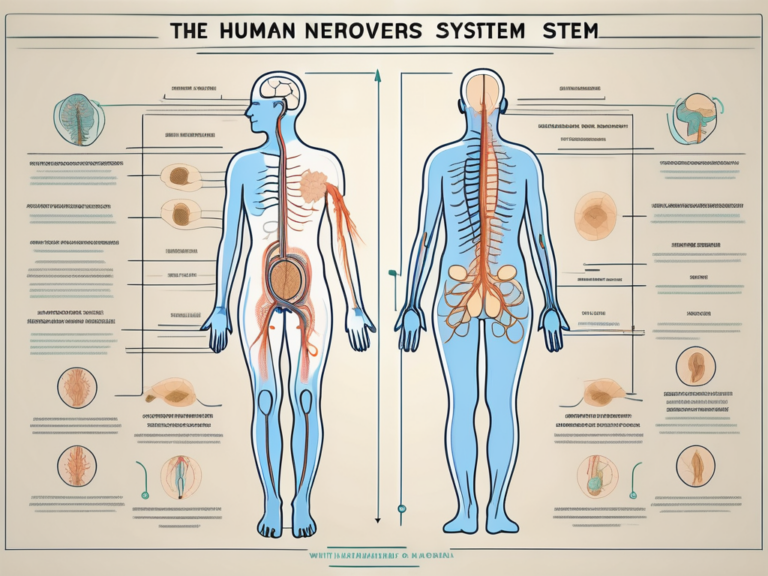
The Role of the Nervous System in Pain Perception
The nervous system is responsible for transmitting signals throughout the body, including those related to pain. Nerve pain, also known as neuropathic pain, can be persistent and challenging to manage. It is important to address nerve pain promptly and effectively to minimize patient discomfort and improve overall quality of life.
The nervous system consists of two main components: the central nervous system (CNS) and the peripheral nervous system (PNS). The CNS includes the brain and spinal cord, while the PNS encompasses the nerves that extend from the CNS to the rest of the body.
When an injury occurs, such as a sacral fracture or pelvic injury, the nerves in the affected area transmit signals to the brain, alerting it to the presence of pain. The brain then processes these signals and generates the sensation of pain, which serves as a protective mechanism to prevent further harm and promote healing.
In the case of nerve pain, the nerves themselves become the source of discomfort. Nerve damage or compression can result in abnormal signaling, leading to sensations such as burning, tingling, or shooting pain. These sensations can be chronic and debilitating, significantly impacting an individual’s quality of life.
Managing nerve pain often requires a multidisciplinary approach, involving healthcare professionals from various specialties. Treatment options may include medications to alleviate pain, physical therapy to improve mobility and function, and interventions such as nerve blocks or surgical procedures to address the underlying cause of the pain.
In conclusion, sacral fractures and pelvic injuries can cause nerve pain due to the proximity of nerves to the affected area. The nervous system plays a crucial role in pain perception, transmitting signals from the injury site to the brain, resulting in the sensation of pain. Understanding the mechanisms behind nerve pain and seeking appropriate medical care is essential for effective management and improved quality of life for individuals with these injuries.
The Healing Process of Sacral Fractures and Pelvic Injuries
Healing from sacral fractures and pelvic injuries involves a complex process that requires time and proper care. The body has natural healing mechanisms in place, but various factors can influence the healing time and the alleviation of nerve pain.
When a sacral fracture or pelvic injury occurs, the body initiates a healing response to repair the damaged tissues. This process involves the formation of new bone tissue, restoration of blood supply to the area, and the regeneration of damaged nerves.
The body’s natural healing response can take several weeks or even months, depending on the severity of the injury. During this time, it is crucial to follow the healthcare provider’s recommendations for rest, immobilization, and physical therapy to aid in the healing process.
In addition to the body’s natural healing response, there are several other factors that can influence the healing time of sacral fractures and pelvic injuries. The severity of the injury plays a significant role in determining the duration of the healing process. More severe fractures or injuries may take longer to heal compared to milder ones.
Another factor that can affect healing time is the individual’s age and overall health. Younger individuals tend to heal faster than older individuals due to their higher metabolic rate and better tissue regeneration capabilities. Additionally, individuals with underlying medical conditions such as osteoporosis or diabetes may experience delayed healing due to compromised bone health or impaired blood circulation.
For individuals with nerve pain resulting from sacral fractures or pelvic injuries, it is crucial to work closely with healthcare professionals to develop an individualized treatment plan. This may include pain management strategies such as medications or nerve blocks to alleviate discomfort. Rehabilitation exercises, guided by physical therapists, can also promote optimal healing and restore strength and flexibility to the affected area.
Furthermore, the emotional and psychological well-being of the patient can also impact the healing process. Dealing with the physical limitations and pain associated with sacral fractures and pelvic injuries can be challenging. It is essential for patients to receive emotional support and counseling to cope with the emotional aspects of their recovery.
In conclusion, healing from sacral fractures and pelvic injuries is a complex process that involves the body’s natural healing mechanisms, as well as various external factors. Following healthcare provider’s recommendations, managing pain, and addressing emotional well-being are all crucial aspects of the healing journey. With time, proper care, and support, individuals can achieve optimal healing and regain their quality of life.
Pain Management Strategies for Sacral Fracture and Pelvic Injury
Managing nerve pain resulting from sacral fractures and pelvic injuries requires a multi-faceted approach. While complete elimination of pain may not always be possible, several strategies can help alleviate discomfort and improve quality of life.
When it comes to managing nerve pain, a combination of medications, physical therapy, and surgical interventions may be necessary. Each approach has its own benefits and considerations, and consulting with a healthcare professional is crucial to determine the most appropriate course of action.
Medications for Nerve Pain Relief
Prescription medications can be an effective tool in managing nerve pain caused by sacral fractures and pelvic injuries. Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used to reduce inflammation and alleviate pain. These medications work by blocking the production of certain chemicals in the body that contribute to pain and inflammation.
In addition to NSAIDs, opioids may be prescribed for more severe cases of nerve pain. These medications work by binding to opioid receptors in the brain and spinal cord, reducing the perception of pain. However, it is important to note that opioids can be highly addictive and should be used with caution under the guidance of a healthcare professional.
Furthermore, there are nerve pain-specific medications available that target the underlying mechanisms of nerve pain. These medications, such as anticonvulsants and antidepressants, can help regulate abnormal nerve signals and provide relief from pain.
It is important to consult with a healthcare professional before starting or changing any medication regimen. They can assess the severity of the nerve pain and any underlying medical conditions to determine the most appropriate medications and dosages. Additionally, they can monitor for potential risks and side effects associated with certain medications.
Physical Therapy and Rehabilitation
Physical therapy and rehabilitation play a crucial role in the recovery process for sacral fractures and pelvic injuries. These interventions focus on improving mobility, strength, and flexibility, while also addressing nerve pain.
Physical therapists are skilled in designing individualized exercise programs and techniques to promote healing, relieve pain, and restore functionality. They may incorporate a variety of exercises, such as stretching, strengthening, and balance training, to target specific areas affected by the injury.
In addition to exercises, manual therapy techniques, such as massage and joint mobilization, can help alleviate nerve pain by reducing muscle tension and improving circulation. Specialized equipment, such as braces or assistive devices, may also be recommended to aid in the recovery process and protect the injured area.
Regular physical therapy sessions, combined with at-home exercises and self-care techniques, can significantly improve the overall outcome of sacral fractures and pelvic injuries. The goal is to gradually restore function, reduce pain, and enhance the individual’s quality of life.
Surgical Interventions and Their Impact on Pain Relief
In some cases, surgical interventions may be necessary to repair severe sacral fractures or pelvic injuries. These procedures aim to stabilize the bones and relieve pressure on nerves, which can help alleviate nerve pain.
Surgical interventions are typically considered when conservative treatments have not provided sufficient pain relief or when the injury is causing significant functional impairment. The decision to undergo surgery should be made in collaboration with a healthcare professional, taking into consideration the individual’s overall health and specific circumstances.
There are different surgical approaches depending on the nature and severity of the injury. For sacral fractures, internal fixation techniques, such as the use of screws or plates, may be employed to stabilize the fractured bones. In cases of pelvic injuries, surgical procedures may involve the use of external fixators or the reconstruction of damaged structures.
While surgical interventions can provide significant pain relief and improve overall function, they also carry risks and require a period of recovery. It is important for individuals to follow post-operative instructions and engage in rehabilitation programs to optimize the surgical outcome.
In conclusion, managing nerve pain resulting from sacral fractures and pelvic injuries requires a comprehensive approach that may include medications, physical therapy, and surgical interventions. Each strategy has its own benefits and considerations, and the most appropriate course of action should be determined in consultation with a healthcare professional. By addressing the underlying causes of nerve pain and implementing targeted interventions, individuals can find relief and improve their quality of life.
The Road to Recovery: What to Expect
Recovering from sacral fractures and pelvic injuries can be a gradual process, and the timeline for alleviating nerve pain can vary significantly from person to person.
Short-term and Long-term Prognosis
In the short term, individuals may experience considerable discomfort and limited mobility. With proper medical care, rest, and rehabilitation, most people can expect to see gradual improvements in pain and function over time.
In the long term, the prognosis for sacral fractures and pelvic injuries is generally positive. The majority of individuals will experience significant pain relief and regain full or near-full functionality with proper management and rehabilitation.
Coping Mechanisms and Lifestyle Adjustments
In addition to medical interventions, coping mechanisms and lifestyle adjustments can play a significant role in managing nerve pain and promoting recovery.
Some potential coping mechanisms include mindfulness techniques, relaxation exercises, and engaging in enjoyable activities. It is also important to maintain a healthy lifestyle by adopting a balanced diet, getting enough rest, and avoiding activities that may exacerbate pain or hinder the healing process.
The Importance of Follow-up Care and Regular Check-ups
Regular follow-up care and check-ups are crucial for individuals recovering from sacral fractures and pelvic injuries. Healthcare professionals can monitor progress, make adjustments to the treatment plan as necessary, and address any concerns or questions that may arise.
It is important to remember that every individual and injury is unique, and the time it takes to alleviate nerve pain from sacral fractures and pelvic injuries can vary. Consulting with a healthcare professional experienced in managing these injuries is key to receiving appropriate care and guidance throughout the recovery process.
While the information provided in this article aims to offer general insights, it is not intended as medical advice. Always consult with a qualified healthcare professional for an accurate diagnosis and personalized treatment recommendations.