Where Is the Sacral Nerve That Controls the Sphincter?
The sacral nerve is a crucial component of our body’s nervous system, playing a vital role in controlling the sphincter. Understanding the sacral nerve and its function is important in recognizing the impact it has on various bodily functions. In this article, we will delve into the anatomy of the sacral nerve, its relationship with the sphincter, and the potential disorders that can arise if the sacral nerve becomes damaged or impaired.
Understanding the Sacral Nerve
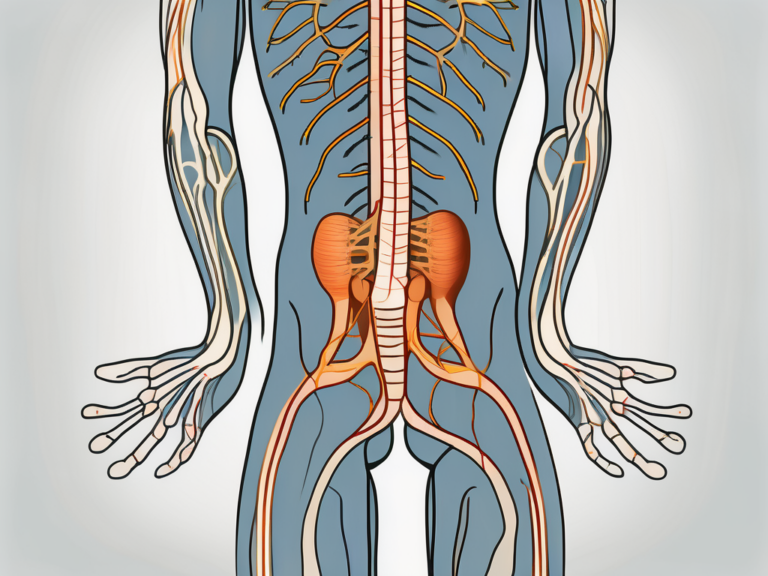
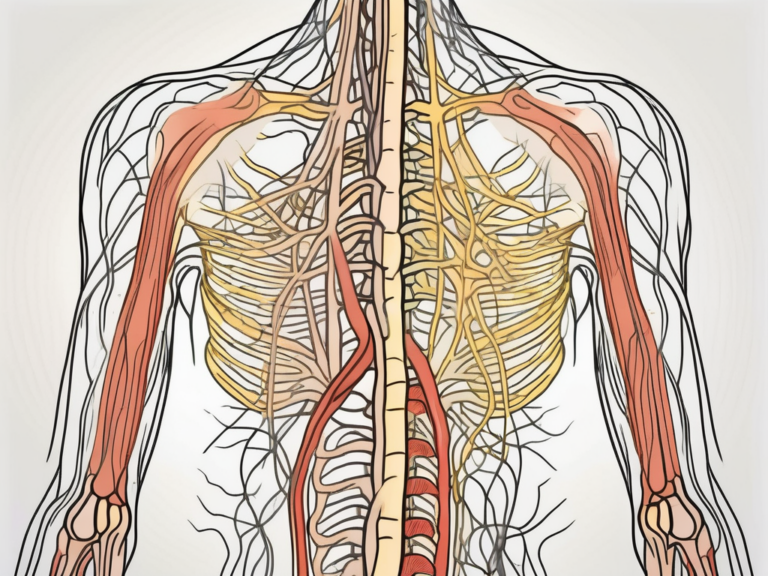
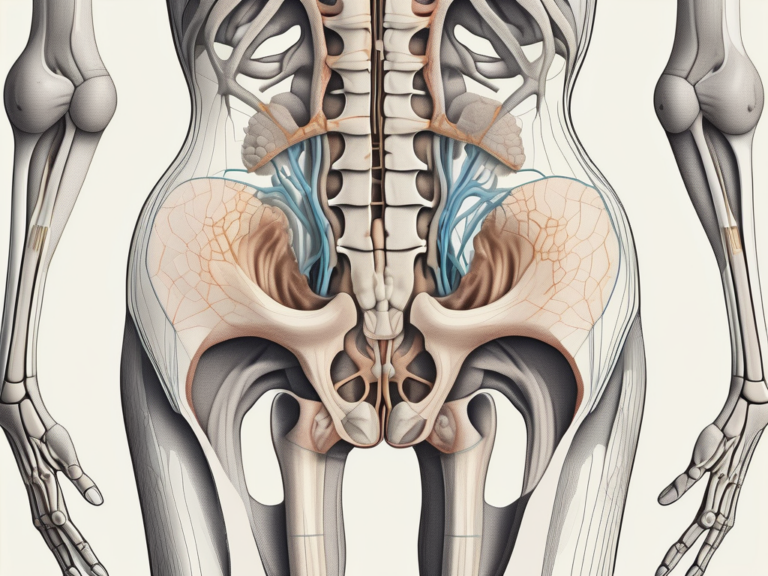
The sacral nerve is located in the lower back region, specifically in the sacrum, which is the triangular bone situated between the hip bones. It emerges from the spinal cord and extends through a series of interconnected nerve roots known as the cauda equina. The sacral nerve is a key part of the peripheral nervous system, responsible for transmitting messages between the brain and the muscles and organs located in the pelvic region.
The sacral nerve, although relatively small in size, plays a vital role in maintaining proper bodily function. It serves as a crucial link between the brain and the pelvic region, facilitating communication and coordination between various muscles and organs.
The Role of the Sacral Nerve in the Body
As one of the primary nerves responsible for autonomic control, the sacral nerve plays a crucial role in the functioning of several bodily systems. It controls the muscles that are involved in bowel and bladder movements, sexual function, and the contraction of the pelvic floor muscles.
When it comes to bowel movements, the sacral nerve ensures the proper coordination of the muscles in the rectum and anus, allowing for the smooth passage of stool. Similarly, it plays a vital role in controlling the muscles of the bladder, enabling the storage and release of urine.
In terms of sexual function, the sacral nerve is involved in the regulation of sexual arousal, orgasm, and ejaculation in males. In females, it contributes to the contraction of the vaginal muscles during sexual activity.
Furthermore, the sacral nerve is responsible for the contraction and relaxation of the pelvic floor muscles. These muscles provide support to the pelvic organs, including the bladder, uterus, and rectum. They also play a crucial role in maintaining continence, preventing urinary and fecal incontinence.
The Anatomy of the Sacral Nerve
The sacral nerve is composed of a network of nerve fibers that carry motor, sensory, and autonomic signals to and from the brain. It consists of both motor and sensory nerve fibers, which enable the transmission of signals related to movement and sensation.
The motor nerve fibers of the sacral nerve innervate the muscles involved in pelvic function. These include the muscles responsible for bowel and bladder control, as well as the muscles involved in sexual function. The motor signals originating from the brain travel through the sacral nerve, allowing for precise and coordinated muscle movements.
On the other hand, the sensory nerve fibers of the sacral nerve transmit information from the pelvic region to the brain. These fibers enable the perception of sensations such as touch, pressure, and pain in the pelvic area. They also play a role in conveying information related to bladder and bowel fullness, allowing for appropriate responses and actions.
The sacral nerve branches out from the spinal cord and extends towards specific areas of the body involved in pelvic function. It forms connections with the muscles and organs in the pelvic region, ensuring effective communication and control.
In conclusion, the sacral nerve is a vital component of the peripheral nervous system, responsible for transmitting messages between the brain and the muscles and organs of the pelvic region. Its role in autonomic control, bowel and bladder function, sexual function, and pelvic floor muscle contraction highlights its importance in maintaining overall bodily function and well-being.
The Sacral Nerve and the Sphincter
The sphincter, located at the opening of various body cavities, is directly controlled by the sacral nerve. This vital muscle regulates the flow of substances in and out of these cavities, such as the release of urine from the bladder and the passage of feces through the rectum. The sacral nerve coordinates the contraction and relaxation of the sphincter muscles to ensure the proper flow and control of bodily waste.
The sacral nerve, also known as the sacral plexus, is a complex network of nerves that originates from the lower part of the spinal cord. It is responsible for transmitting signals between the brain and the pelvic organs, including the sphincter muscles. This intricate communication system allows for precise control over the opening and closing of the sphincter, ensuring efficient waste elimination.
How the Sacral Nerve Controls the Sphincter
When the sacral nerve receives signals from the brain indicating the need for the sphincter to relax, it triggers the relaxation of the muscle, allowing the release of waste. This process is essential for normal bodily functions, as it enables the bladder to empty and the rectum to expel feces. The coordination between the sacral nerve and the sphincter muscles ensures that these actions occur at the appropriate times.
Conversely, when the brain signals the need to retain waste, the sacral nerve initiates the contraction of the sphincter muscles, ensuring tight closure and preventing leakage. This mechanism is crucial for maintaining continence and preventing involuntary release of urine or feces. The sacral nerve acts as a gatekeeper, responding to signals from the brain to either open or close the sphincter, depending on the body’s needs.
The Connection Between the Sacral Nerve and Sphincter Function
It is important to understand that any disruption or damage to the sacral nerve can result in impaired sphincter function. This can lead to issues such as urinary or fecal incontinence, where individuals may have difficulty controlling the release of waste. In some cases, dysfunction of the sacral nerve can result in an overactive bladder, causing frequent urges to urinate.
Conditions that can affect the sacral nerve and subsequently impact sphincter function include spinal cord injuries, nerve damage, and certain neurological disorders. For example, conditions like multiple sclerosis or Parkinson’s disease can disrupt the normal functioning of the sacral nerve, leading to problems with sphincter control.
Treatment options for sacral nerve dysfunction vary depending on the underlying cause and severity of the condition. In some cases, medications or physical therapy may be recommended to improve nerve function and restore sphincter control. In more severe cases, surgical interventions, such as sacral nerve stimulation, may be considered to help regulate the nerve signals and restore proper sphincter function.
Overall, the sacral nerve plays a crucial role in controlling the sphincter muscles and maintaining proper waste elimination. Its intricate connection with the brain ensures that the sphincter functions in harmony with the body’s needs. Understanding the relationship between the sacral nerve and sphincter function is essential for diagnosing and treating conditions that can disrupt this delicate balance.
Locating the Sacral Nerve
While the sacral nerve may not be visible to the naked eye, there are several ways to identify its location with the help of medical knowledge and tools.
The sacral nerve, also known as the S1 nerve, is an essential component of the nervous system. It originates from the sacral plexus, a complex network of nerves located in the lower back region. This nerve plays a crucial role in transmitting sensory and motor signals between the brain and the lower body.
Identifying the Sacral Nerve on a Diagram
Medical diagrams can accurately depict the location of the sacral nerve and its connection to the spine and pelvic region. Doctors and healthcare professionals can use these diagrams to locate the sacral nerve and assess its condition.
These diagrams often illustrate the intricate network of nerves that make up the sacral plexus. They show the precise path of the sacral nerve as it branches out from the spinal cord and extends into the pelvis. By studying these diagrams, medical professionals can gain a better understanding of the sacral nerve’s location and its relationship to other anatomical structures.
Physical Indicators of the Sacral Nerve’s Location
In some cases, physical indicators can give clues about the location of the sacral nerve. These indicators include the presence of lower back pain, numbness or weakness in the legs, or sensory changes in the pelvic region. However, a proper diagnosis requires the expertise of a trained medical professional.
Lower back pain, a common symptom associated with sacral nerve issues, can be caused by various factors such as nerve compression, inflammation, or injury. It is important to note that lower back pain can have multiple causes, and a thorough examination is necessary to determine if the sacral nerve is involved.
Numbness or weakness in the legs may also indicate a problem with the sacral nerve. The sacral nerve is responsible for transmitting motor signals to the lower limbs, and any disruption in its function can lead to muscle weakness or loss of sensation. This symptom should be evaluated by a healthcare professional to determine its underlying cause.
Sensory changes in the pelvic region, such as altered sensation or abnormal tingling, can also be linked to sacral nerve dysfunction. The sacral nerve provides sensory innervation to the pelvic organs, and any disturbance in its function can result in sensory abnormalities. A comprehensive assessment is necessary to identify the exact cause of these changes.
In conclusion, while the sacral nerve may not be visible to the naked eye, medical diagrams and physical indicators can help identify its location. By utilizing these resources and seeking professional medical advice, individuals can gain a better understanding of the sacral nerve and any potential issues affecting its function.
Disorders Related to the Sacral Nerve and Sphincter
Several disorders can affect the sacral nerve and subsequently impact sphincter function. It is crucial to be aware of these conditions to seek timely medical intervention and appropriate treatment.
The sacral nerve, also known as the S2-S4 nerve roots, plays a vital role in the proper functioning of the pelvic organs, including the bladder, rectum, and reproductive organs. Any disruption or damage to this nerve can have significant consequences on the body’s ability to control these essential bodily functions.
Common Sacral Nerve Disorders
Some common disorders related to the sacral nerve include sacral nerve compression, neuropathy, and injuries. These conditions can arise due to various factors such as trauma, inflammation, or underlying medical conditions like diabetes.
Sacral nerve compression occurs when there is pressure on the nerve roots, leading to pain, numbness, and weakness in the lower back, buttocks, and legs. This compression can result from a herniated disc, spinal stenosis, or even tumors in the pelvic region. Prompt diagnosis and treatment are crucial to prevent further damage and alleviate symptoms.
Neuropathy, another common sacral nerve disorder, refers to damage or dysfunction of the nerve fibers. This condition can cause a range of symptoms, including tingling, burning, or shooting pain in the pelvic region, as well as muscle weakness and loss of sensation. Diabetes, infections, and autoimmune diseases are some of the underlying causes of neuropathy.
Injuries to the sacral nerve can occur due to accidents, falls, or surgical procedures involving the pelvic area. These injuries can lead to severe disruptions in the nerve’s ability to transmit signals, resulting in impaired sphincter function and other complications.
Impact of Sacral Nerve Disorders on the Sphincter
When the sacral nerve is impaired, it can result in disruptions to the coordinated functioning of the sphincter muscles. This can lead to fecal or urinary incontinence, urinary retention, or difficulties with sexual function. Consulting with a healthcare professional is crucial for accurate diagnosis and appropriate treatment.
Fecal incontinence refers to the inability to control bowel movements, leading to involuntary leakage of stool. This condition can significantly impact an individual’s quality of life, causing embarrassment, social isolation, and a decline in overall well-being. Urinary incontinence, on the other hand, involves the unintentional loss of urine, which can occur during activities such as coughing, sneezing, or exercising.
Urinary retention, a common consequence of sacral nerve disorders, refers to the inability to empty the bladder fully. This can cause discomfort, frequent urination, and an increased risk of urinary tract infections. In severe cases, urinary retention may require catheterization to relieve the bladder and prevent complications.
Furthermore, sacral nerve disorders can also affect sexual function, leading to difficulties with arousal, orgasm, and erectile dysfunction in men. These challenges can have a significant impact on intimate relationships and overall sexual satisfaction.
In conclusion, disorders related to the sacral nerve can have profound effects on sphincter function and overall quality of life. It is essential to recognize the signs and symptoms of these conditions and seek medical attention promptly. With accurate diagnosis and appropriate treatment, individuals can regain control over their bodily functions and improve their well-being.
Treatment Options for Sacral Nerve Disorders
The treatment of sacral nerve disorders typically depends on the underlying cause and severity of the condition. Non-surgical and surgical options may be considered based on the individual’s specific needs and medical advice.
Sacral nerve disorders can cause a range of symptoms, including pain, numbness, and weakness in the lower back, buttocks, and legs. These symptoms can significantly impact a person’s quality of life and ability to perform daily activities. Therefore, it is crucial to explore various treatment options to alleviate symptoms and improve overall well-being.
Non-Surgical Treatments for Sacral Nerve Disorders
Non-surgical treatment options for sacral nerve disorders may include medication to manage pain and inflammation, physical therapy to strengthen pelvic muscles, and lifestyle modifications to support overall pelvic health.
Medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) or nerve pain medications may be prescribed to reduce pain and inflammation associated with sacral nerve disorders. These medications can provide temporary relief and improve the individual’s ability to engage in physical therapy exercises.
Physical therapy plays a crucial role in the non-surgical management of sacral nerve disorders. A physical therapist can design a personalized exercise program to strengthen the pelvic muscles, improve flexibility, and enhance overall stability. These exercises may include pelvic floor exercises, stretching, and core strengthening exercises.
In addition to medication and physical therapy, lifestyle modifications can also contribute to the management of sacral nerve disorders. These modifications may include maintaining a healthy weight, avoiding activities that aggravate symptoms, and practicing good posture. Additionally, alternative therapies such as acupuncture or chiropractic care may be considered to complement conventional treatments.
It is important to consult with a healthcare professional to determine the most appropriate treatment plan for sacral nerve disorders. The healthcare provider will consider the individual’s specific symptoms, medical history, and lifestyle factors to develop a comprehensive treatment approach.
Surgical Treatments for Sacral Nerve Disorders
In cases where conservative approaches are ineffective, surgical intervention may be necessary. Surgical treatments for sacral nerve disorders aim to address the underlying cause of the condition and alleviate symptoms.
Surgeons may explore options such as nerve decompression, nerve grafting, or implantation of neuromodulation devices to address sacral nerve disorders. Nerve decompression involves removing any structures that may be compressing the sacral nerves, such as herniated discs or bone spurs. Nerve grafting is a procedure where a healthy nerve is transplanted to replace a damaged or injured nerve. Implantation of neuromodulation devices, such as spinal cord stimulators, can help manage pain by delivering electrical impulses to the sacral nerves.
These surgical procedures should be carefully considered in consultation with a specialist. The decision to undergo surgery depends on various factors, including the severity of symptoms, the individual’s overall health, and the potential risks and benefits of the procedure. The specialist will thoroughly evaluate the individual’s condition and discuss the surgical options, potential outcomes, and post-operative care.
It is important to note that while surgical treatments can provide significant relief for sacral nerve disorders, they may not be suitable for everyone. Each case is unique, and the treatment plan should be tailored to the individual’s specific needs and circumstances.
Preventing Sacral Nerve Damage
While not all causes of sacral nerve disorders can be prevented, adopting certain lifestyle changes can help reduce the risk of damage to this crucial nerve.
Lifestyle Changes to Protect the Sacral Nerve
Avoiding excessive strain on the lower back, maintaining good posture, and engaging in regular exercise that targets core and pelvic muscles can all contribute to the overall health and protection of the sacral nerve. Additionally, maintaining a healthy weight and managing conditions such as diabetes can also help prevent damage to this vital nerve.
Exercises to Strengthen the Sacral Nerve
Physical therapy exercises targeting the pelvic floor muscles can strengthen the sacral nerve and improve overall sphincter function. These exercises, such as Kegels, help maintain muscle tone and promote coordination within the pelvic region. It is essential to consult with a healthcare professional or physical therapist to ensure proper technique and guidance when performing these exercises.
In conclusion, understanding the location and function of the sacral nerve that controls the sphincter is crucial for maintaining proper bodily function. Recognizing potential disorders related to the sacral nerve and seeking appropriate medical intervention can significantly impact quality of life. Remember, if you experience any symptoms or concerns related to bowel or bladder control, it is essential to consult with a healthcare professional for an accurate diagnosis and personalized treatment plan.