What Is a Sacral Nerve Ablation: A Comprehensive Guide
If you are experiencing chronic back pain or pelvic pain, you may have come across the term “sacral nerve ablation.” But what exactly does it mean, and how can it help alleviate your discomfort? In this comprehensive guide, we will explore the ins and outs of sacral nerve ablation, including its definition, purpose, procedure, risks, benefits, recovery, and frequently asked questions.
Understanding Sacral Nerve Ablation
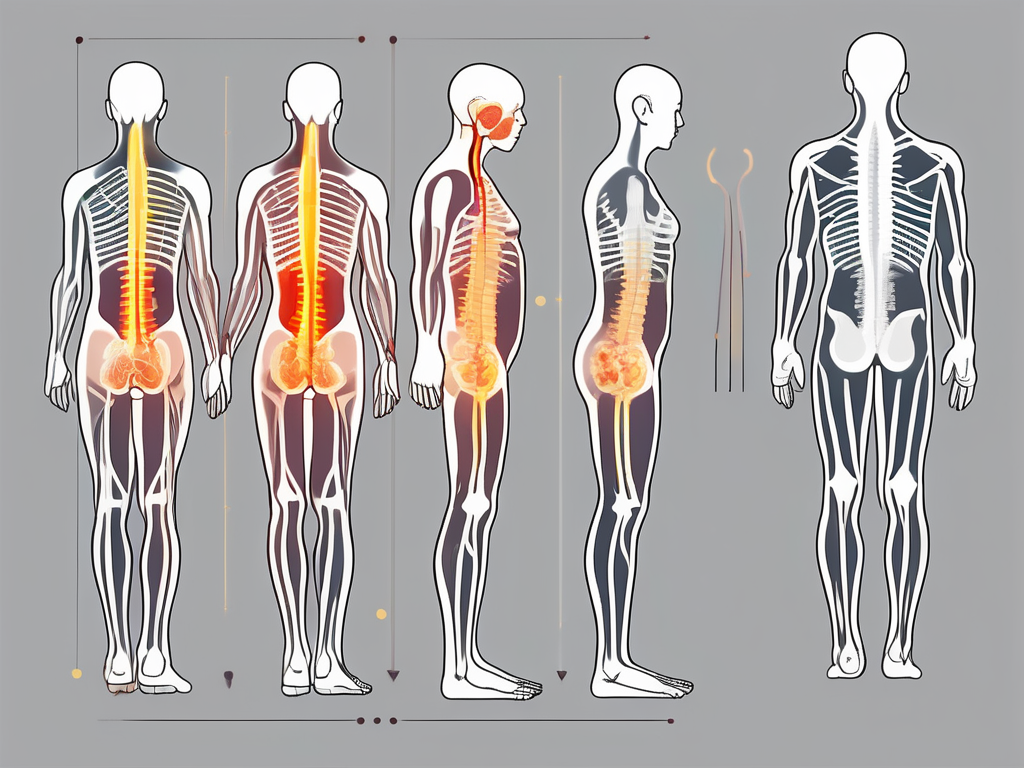
Sacral nerve ablation is a minimally invasive procedure that aims to provide relief from chronic pain in the lower back and pelvic region. By targeting specific nerves in the sacrum, which is the triangular bone at the base of the spine, this procedure disrupts the pain signals being sent to the brain, thereby reducing or eliminating pain sensation.
Chronic pain in the lower back and pelvic region can significantly impact a person’s quality of life. It can limit their ability to perform daily activities, affect their mobility, and even lead to emotional distress. Sacral nerve ablation offers hope to individuals who have been struggling with persistent pain and have not found adequate relief through traditional methods.
Definition and Purpose of Sacral Nerve Ablation
Sacral nerve ablation, also known as sacroiliac joint radiofrequency ablation, is a treatment option for individuals suffering from chronic lower back pain and pelvic pain. The procedure utilizes radiofrequency energy to heat and destroy the nerves responsible for transmitting pain signals from the sacroiliac joints in the lower back to the brain.
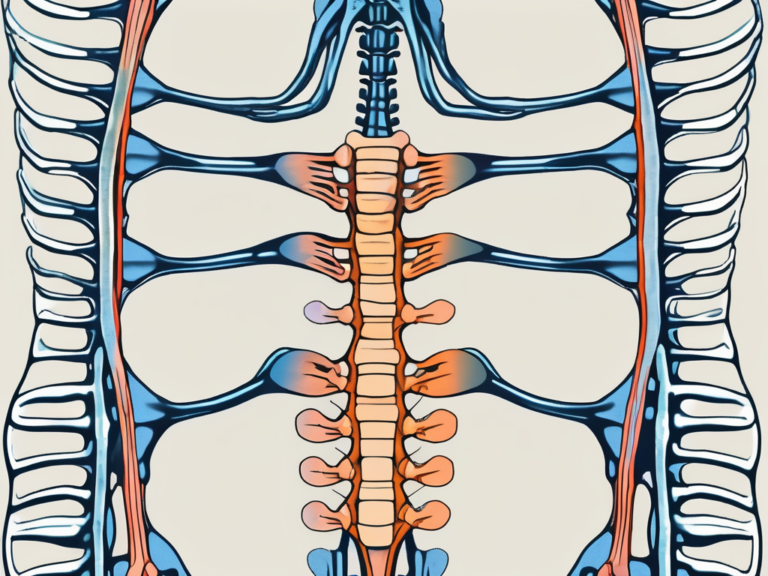
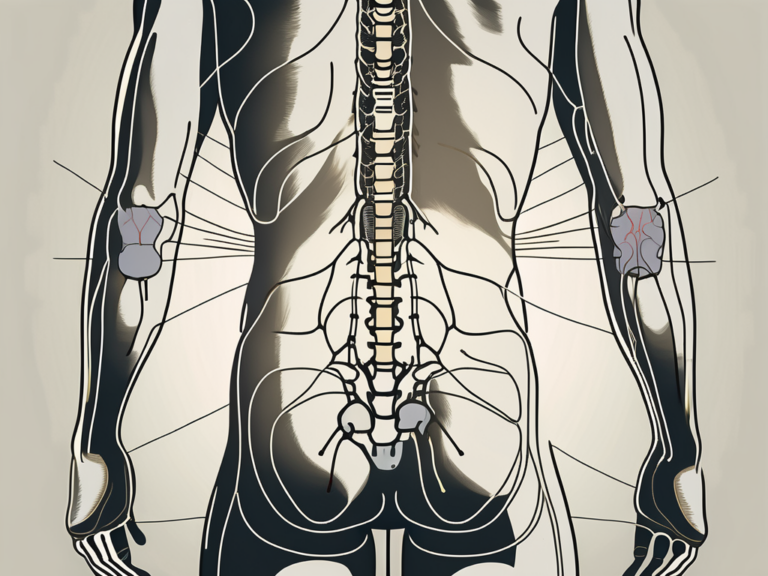
The sacroiliac joints, located between the sacrum and the ilium bones of the pelvis, are responsible for transferring weight and forces between the upper body and the legs. When these joints become inflamed or injured, they can cause significant pain and discomfort. Sacral nerve ablation targets the nerves associated with these joints, providing relief and improving overall function.
It is important to note that sacral nerve ablation is not a curative procedure but rather a means of managing pain. The goal of this treatment is to provide long-term relief and improve the overall quality of life for individuals who have not found adequate pain relief through traditional methods.
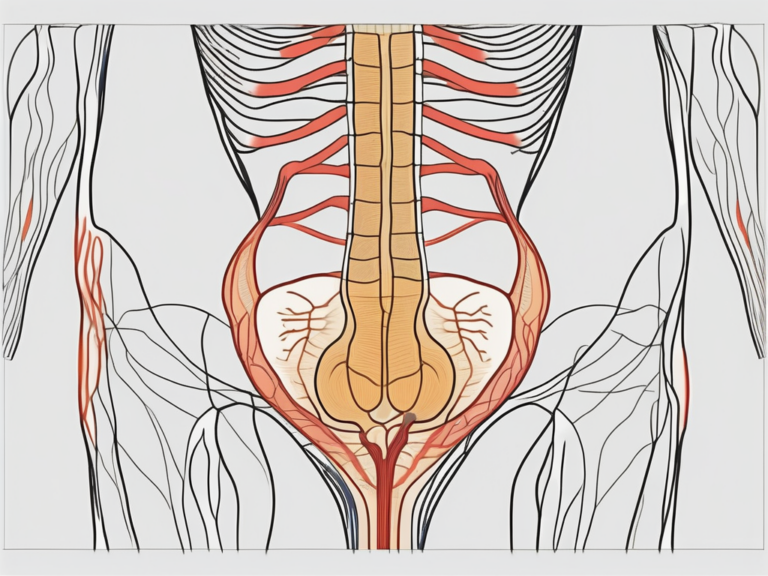
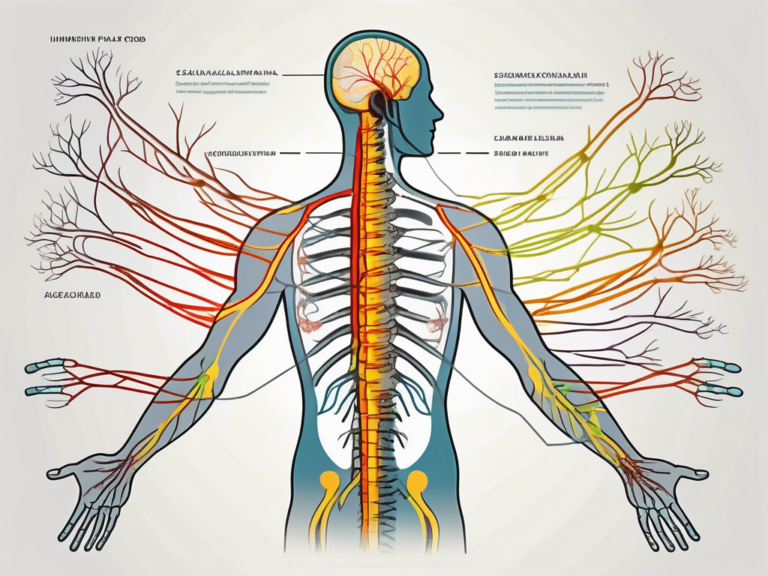
The Anatomy of the Sacral Nerve
Before diving deeper into the procedure itself, it is essential to understand the anatomy of the sacral nerve. The sacral nerve roots emerge from the lower spinal cord and exit the spinal column through tiny bony canals called foramina. These nerve roots then merge together to form the sciatic nerve, which runs down the back of each leg and provides sensation and motor control to the lower extremities.
The sacral nerves play a crucial role in transmitting sensory and motor signals between the brain and the lower body. When these nerves become damaged or inflamed, they can cause persistent pain in the lower back and pelvic area.
Understanding the intricate anatomy of the sacral nerve allows medical professionals to precisely target the nerves during the ablation procedure. By selectively disrupting the pain signals originating from the sacroiliac joints, sacral nerve ablation offers a potential solution for individuals suffering from chronic pain in the lower back and pelvic region.
The Medical Conditions Sacral Nerve Ablation Can Treat
Sacral nerve ablation has shown promising results in the management of chronic back pain and pelvic pain caused by various medical conditions. Let’s take a closer look at two primary conditions that can be effectively treated with this procedure.
Chronic Back Pain and Sacral Nerve Ablation
Chronic back pain is a common condition that can significantly impact one’s quality of life. Whether it is caused by degenerative disc disease, arthritis, or sacroiliac joint dysfunction, the constant pain can be debilitating. For individuals who have not found relief through conservative treatments such as physical therapy or medication, sacral nerve ablation offers a viable option to manage their pain.
When it comes to degenerative disc disease, the gradual wear and tear of the spinal discs can lead to chronic back pain. This condition commonly affects older individuals and can cause symptoms such as stiffness, limited mobility, and radiating pain. Sacral nerve ablation targets the nerves responsible for transmitting pain signals from the sacroiliac joints, providing significant pain reduction and improving overall function.
Arthritis, another common cause of chronic back pain, involves inflammation of the joints in the spine. This inflammation can lead to pain, stiffness, and reduced range of motion. Sacral nerve ablation can effectively alleviate the pain associated with arthritis by targeting the specific nerves involved in transmitting pain signals.
Sacroiliac joint dysfunction, characterized by pain in the lower back and buttocks, is another condition that can be effectively treated with sacral nerve ablation. This dysfunction occurs when the sacroiliac joints, which connect the sacrum to the pelvis, become irritated or inflamed. By selectively targeting the nerves responsible for transmitting pain signals from the sacroiliac joints, sacral nerve ablation can provide significant pain reduction and improve the patient’s quality of life.
However, it is crucial to consult with a medical professional to determine whether this procedure is appropriate for your specific condition. They will evaluate your medical history, conduct a thorough examination, and consider other treatment options before recommending sacral nerve ablation.
Sacral Nerve Ablation for Pelvic Pain
Pelvic pain, which can be caused by conditions such as endometriosis, interstitial cystitis, or chronic pelvic inflammatory disease, can have a profound impact on a person’s daily life. Traditional treatments, including medications and physical therapy, may not always provide sufficient relief.
Endometriosis, a condition in which the tissue lining the uterus grows outside of it, can cause severe pelvic pain. This pain can be debilitating and may interfere with daily activities. Sacral nerve ablation has emerged as a potential solution for individuals suffering from chronic pelvic pain due to endometriosis. By selectively targeting the nerves responsible for transmitting pain signals from the pelvic region, this procedure can offer significant pain reduction or elimination in some cases.
Interstitial cystitis, a chronic bladder condition characterized by frequent urination and pelvic pain, can also be effectively treated with sacral nerve ablation. This condition can cause discomfort and disrupt normal bladder function, leading to a decreased quality of life. Sacral nerve ablation can provide relief by targeting the nerves responsible for transmitting pain signals from the pelvic region.
Chronic pelvic inflammatory disease, an infection of the female reproductive organs, can cause persistent pelvic pain. This condition can be challenging to treat, and traditional methods may not always provide adequate relief. Sacral nerve ablation offers a potential solution by selectively targeting the nerves responsible for transmitting pain signals from the pelvic region, providing significant pain reduction or elimination in some cases.
However, it is important to note that sacral nerve ablation may not be suitable for all individuals with pelvic pain, and a comprehensive evaluation by a medical professional is crucial to determine the right treatment approach. They will consider your specific condition, medical history, and other treatment options before recommending sacral nerve ablation as a potential solution.
The Sacral Nerve Ablation Procedure
Now that we have covered the basics of sacral nerve ablation and the conditions it can treat, let’s delve into the actual procedure itself. To provide a comprehensive understanding, we will explore both the preparation required and a step-by-step guide to the procedure.
Preparing for the Procedure
Prior to undergoing sacral nerve ablation, a thorough evaluation by a healthcare professional is essential. This evaluation will involve a review of your medical history, a physical examination, and potentially imaging studies to assess the source of your pain.
During the evaluation, your healthcare provider will take the time to discuss the procedure with you, explaining the benefits, risks, and potential outcomes. This open and honest conversation will allow you to make an informed decision about whether sacral nerve ablation is the right treatment option for you.
Once it is determined that sacral nerve ablation is a suitable treatment option, you will be given detailed instructions on how to prepare for the procedure. This may include fasting for a certain period before the procedure, discontinuing specific medications, and arranging for transportation to and from the healthcare facility.
Additionally, your healthcare provider may recommend certain lifestyle modifications leading up to the procedure. These modifications could include avoiding strenuous activities, getting adequate rest, and managing stress levels to optimize your overall well-being.
Step-by-Step Guide to the Procedure
- Administration of local anesthesia: To ensure your comfort during the procedure, a local anesthetic will be administered to numb the area where the procedure will take place. This ensures that you will not experience any pain or discomfort throughout the process.
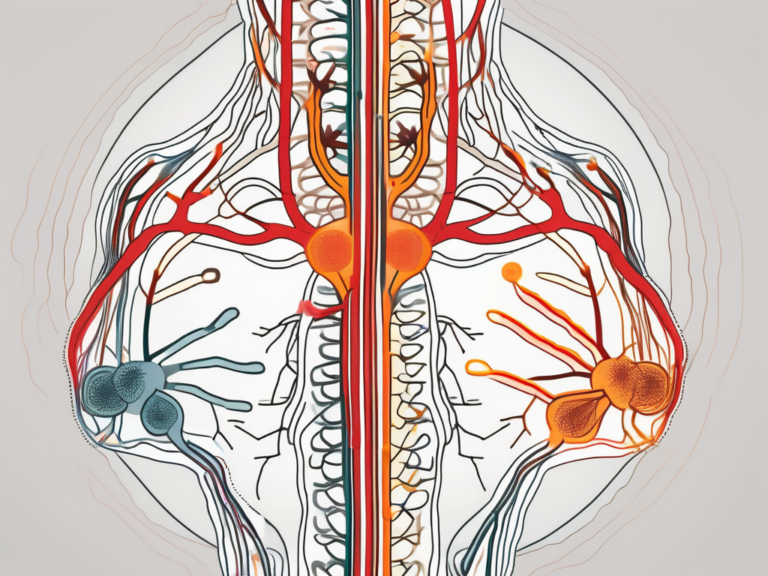
- Insertion of the needle: Using fluoroscopic guidance, a thin needle will be inserted into the targeted area, guided by real-time X-ray imaging. This ensures precise placement of the needle, minimizing the risk of complications and maximizing the effectiveness of the procedure.
- Confirmation of needle position: Once the needle is in the correct position, a contrast dye may be injected to confirm accurate needle placement. This dye allows the healthcare provider to visualize the targeted nerves more clearly, ensuring that the treatment is focused on the intended area.
- Radiofrequency energy delivery: After confirming proper needle placement, radiofrequency energy will be sent through the needle, heating the targeted nerves. The precise delivery of energy disrupts the nerves’ ability to transmit pain signals effectively, providing long-lasting pain relief.
- Post-procedure care: Following the procedure, you will be monitored for a short period to ensure no immediate complications arise. Pain relief may be experienced immediately or within a few days, depending on the individual and the specific condition being treated.
It is important to note that the specific details of the procedure may vary depending on the healthcare provider and the individual circumstances. Therefore, it is essential to have a thorough discussion with your healthcare provider to address any specific concerns or questions you may have.
Furthermore, it is crucial to follow all post-procedure instructions provided by your healthcare provider. This may include avoiding certain activities, taking prescribed medications, and attending follow-up appointments to monitor your progress and ensure optimal outcomes.
Remember, sacral nerve ablation is a minimally invasive procedure that can significantly improve your quality of life by reducing or eliminating chronic pain. By understanding the preparation and steps involved, you can approach the procedure with confidence and make informed decisions about your healthcare.
Risks and Benefits of Sacral Nerve Ablation
As with any medical procedure, sacral nerve ablation carries both risks and benefits. Understanding these can help you make an informed decision about whether this treatment option is suitable for you.
Sacral nerve ablation is a minimally invasive procedure that is commonly used to treat chronic pain in the lower back and pelvic area. It involves the use of radiofrequency energy to disrupt the nerve signals that are responsible for transmitting pain sensations from the sacral nerves to the brain. While this procedure has shown promising results in many cases, it is important to consider the potential risks and complications before making a decision.
Potential Risks and Complications
While sacral nerve ablation is generally considered safe, there are potential risks and complications associated with the procedure. These may include infection, bleeding, nerve damage, allergic reactions to medications or contrast dye, and rarely, damage to nearby structures or organs.
Infection is a potential risk with any invasive procedure, but steps are taken to minimize this risk, such as using sterile equipment and following strict hygiene protocols. Bleeding can occur during or after the procedure, but this is usually minor and can be managed with proper care. Nerve damage is a rare complication, but it can occur if the radiofrequency energy affects nearby nerves. Allergic reactions to medications or contrast dye are also rare, but it is important to inform your healthcare provider about any known allergies before the procedure. Damage to nearby structures or organs is extremely rare, but it is a possibility that should be considered.
It is important to discuss these potential risks and complications with your healthcare provider to determine whether the benefits outweigh the potential harms in your particular case. They can provide you with more specific information about the likelihood of these complications and how they can be managed or prevented.
Expected Benefits and Success Rates
The primary benefit of sacral nerve ablation is the potential reduction or elimination of chronic pain in the lower back and pelvic area. Studies have shown that a significant percentage of individuals experience improved pain control and quality of life following the procedure.
Chronic pain can have a significant impact on a person’s daily life, affecting their ability to work, engage in physical activities, and enjoy social interactions. Sacral nerve ablation offers a potential solution for those who have not found relief from other treatments, such as medication or physical therapy. By disrupting the pain signals, this procedure can provide long-lasting pain relief and improve overall well-being.
However, it is important to note that the effectiveness of sacral nerve ablation may vary depending on the individual and the specific condition being treated. Factors such as the underlying cause of the pain, the severity of the symptoms, and the overall health of the patient can all influence the outcome of the procedure. Your healthcare provider can provide more information about the expected benefits and success rates in your situation.
In conclusion, sacral nerve ablation is a treatment option that carries both risks and benefits. It is important to have a thorough discussion with your healthcare provider to fully understand the potential risks and complications, as well as the expected benefits and success rates. By weighing these factors, you can make an informed decision about whether sacral nerve ablation is the right choice for you.
Recovery and Aftercare Following Sacral Nerve Ablation
Following sacral nerve ablation, proper recovery and aftercare are essential for maximizing the procedure’s benefits and minimizing potential complications. Let’s explore the immediate post-procedure care and the long-term recovery and lifestyle adjustments that may be necessary.
Immediate Post-Procedure Care
After the procedure, you may experience some temporary discomfort or soreness at the injection site. This is normal and can usually be managed with over-the-counter pain relievers as recommended by your healthcare provider.
It is important to follow any specific post-procedure instructions provided by your healthcare provider, including limitations on physical activity and any medication requirements.
Long-Term Recovery and Lifestyle Adjustments
While sacral nerve ablation can provide effective pain relief, it is important to understand that the procedure may not be a permanent solution. In some cases, additional treatments or procedures may be necessary to maintain pain control and address any underlying causes.
Your healthcare provider will work with you to develop a comprehensive treatment plan that may include physical therapy, lifestyle modifications, or other interventions to aid in your long-term recovery. It is essential to follow the guidance of your healthcare team and engage in open communication to achieve the best possible outcome.
Frequently Asked Questions about Sacral Nerve Ablation
Is Sacral Nerve Ablation Painful?
The procedure itself is typically performed under local anesthesia, which helps minimize discomfort during the process. Some individuals may experience mild discomfort or soreness at the injection site following the procedure, but this is usually temporary and can be managed with over-the-counter pain relievers.
It is important to discuss any concerns about pain or discomfort with your healthcare provider before the procedure. They can provide additional guidance and recommendations to ensure your comfort throughout the process.
How Long Does the Procedure Last?
The duration of the sacral nerve ablation procedure can vary depending on various factors, including the individual’s specific condition and the complexity of the case. In general, the procedure typically takes between 30 minutes to one hour.
It is important to note that the actual procedure time is only one component of the overall process. Pre-procedure preparation, monitoring, and post-procedure care are also essential components of the treatment timeline. Your healthcare provider can provide more precise information regarding the expected duration of the procedure in your particular case.
In Conclusion
Sacral nerve ablation is a minimally invasive procedure that offers potential relief for individuals suffering from chronic back pain and pelvic pain. By selectively targeting specific nerves in the sacrum, this procedure disrupts pain signals and can provide significant pain reduction and improved quality of life.
However, it is important to understand that sacral nerve ablation is not a curative procedure, and the effectiveness may vary depending on the individual and the specific condition being treated. A comprehensive evaluation and discussion with a healthcare professional are essential to determine whether this treatment option is suitable for you.
As with any medical procedure, sacral nerve ablation carries potential risks and benefits. Understanding the procedure, its risks, expected benefits, and the recovery process will help you make an informed decision about whether sacral nerve ablation is the right choice for you.
If you are experiencing chronic back pain or pelvic pain, consult with a qualified healthcare provider to explore all available treatment options and determine the best course of action for your specific situation.