What Nerve Supplies the Sacral Plexus Root?
The sacral plexus is an essential part of the nervous system, responsible for innervating the lower limbs, pelvis, and perineum. Understanding its anatomy and functions can provide valuable insights into its role in overall health and well-being. In this article, we will explore the intricate details of the sacral plexus, its connection to other nerves, common disorders associated with it, and the future of research in this field.
Understanding the Sacral Plexus
Anatomy of the Sacral Plexus
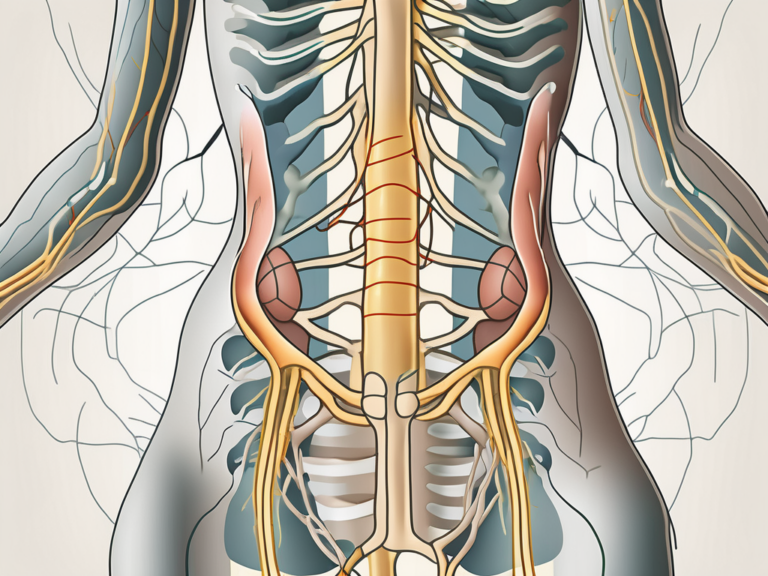
The sacral plexus is a fascinating network of nerves that plays a vital role in the human body. It is formed by the union of nerves arising from the lumbosacral region, specifically the fourth and fifth lumbar spinal nerves and the first to fourth sacral spinal nerves. These nerves intertwine and form a complex network, resembling a “plexus,” hence the name.
Located within the pelvic cavity, adjacent to the sacrum, the sacral plexus is strategically positioned to serve its functions. Within this intricate network, there are several significant nerves responsible for specific functions.
One of the primary nerves involved in the sacral plexus is the sciatic nerve. As the largest nerve in the human body, the sciatic nerve is responsible for providing motor and sensory innervation to the lower limbs. It branches out from the sacral plexus, extending down the leg and enabling us to perform essential movements such as walking, running, and maintaining balance.
In addition to the sciatic nerve, there are other key nerves within the sacral plexus that deserve recognition. The pudendal nerve, for example, plays a crucial role in controlling the muscles of the perineum, which are responsible for various functions such as urination and defecation. The superior gluteal nerve, on the other hand, innervates the gluteus medius, gluteus minimus, and tensor fasciae latae muscles, contributing to hip stability and movement. Lastly, the inferior gluteal nerve innervates the gluteus maximus muscle, which is the largest muscle in the buttocks and plays a significant role in activities such as climbing stairs and standing up from a seated position.
Functions of the Sacral Plexus
The sacral plexus is a powerhouse when it comes to motor and sensory functions. Motor neurons originating from the sacral plexus control the movement of muscles in the lower limbs, pelvis, and perineum. These motor neurons send signals that allow us to perform various activities, from simple tasks like walking to more complex movements like dancing or playing sports.
Moreover, the sacral plexus carries sensory information from the lower limbs, pelvis, and perineum back to the central nervous system. This sensory input helps us perceive touch, temperature, and pain sensations, allowing us to interact with the world around us. For example, when we step on a sharp object, the sensory nerves within the sacral plexus transmit signals to our brain, alerting us to the pain and prompting us to remove our foot from the source of discomfort.
It is important to note that dysfunction in the sacral plexus can lead to various sensory and motor impairments. For instance, damage to the sciatic nerve can result in conditions such as sciatica, characterized by pain, numbness, and tingling sensations that radiate down the leg. Similarly, injuries to the pudendal nerve can cause pelvic pain, urinary and fecal incontinence, and sexual dysfunction.
In conclusion, the sacral plexus is a complex and essential component of the human body. Its intricate network of nerves enables us to perform a wide range of motor activities and perceive sensory information from the lower limbs, pelvis, and perineum. Understanding the anatomy and functions of the sacral plexus is crucial for appreciating the intricacies of the human nervous system and the remarkable capabilities it provides us.
The Nervous System and the Sacral Plexus
The Role of the Nervous System
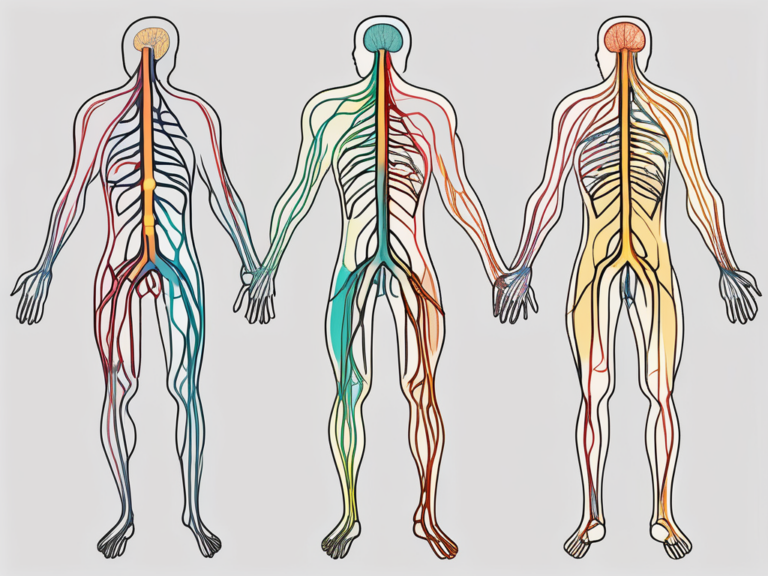
The nervous system is an intricate network of nerves, cells, and tissues that coordinates and controls bodily functions. It is divided into two main components: the central nervous system (CNS) and the peripheral nervous system (PNS).
The CNS, consisting of the brain and spinal cord, acts as the control center for the entire body. It receives and processes information from the PNS and sends out appropriate responses to maintain homeostasis. The PNS, on the other hand, connects the CNS to the rest of the body and includes various structures such as nerves, ganglia, and plexuses.
One of the important plexuses in the PNS is the sacral plexus. This intricate network of nerves is located in the pelvic region and plays a crucial role in the functioning of the lower limbs, pelvis, and perineum.
How the Nervous System Interacts with the Sacral Plexus
The sacral plexus receives input from the brain and spinal cord through various nerve pathways. This interaction allows the nervous system to regulate and control the functioning of the sacral plexus. The CNS sends signals to the sacral plexus, instructing it to initiate specific movements or to receive sensory information from the lower limbs, pelvis, and perineum.
For example, when you decide to take a step forward, the brain sends signals through the spinal cord to the sacral plexus, activating the muscles in your legs and coordinating their movement. This seamless communication between the nervous system and the sacral plexus allows you to walk, run, and perform various activities effortlessly.
Conversely, the sacral plexus relays sensory information back to the CNS, providing crucial feedback about the state of the body. For instance, if you accidentally touch a hot surface, the sacral plexus sends signals to the brain, alerting it of the potential danger. This rapid transmission of sensory information allows the brain to react quickly, pulling your hand away from the hot surface to prevent injury.
Moreover, the sacral plexus also plays a vital role in the regulation of bladder and bowel control. It receives signals from the CNS, instructing the muscles in the pelvic region to contract or relax, allowing for proper elimination and continence.
Overall, the bidirectional communication between the nervous system and the sacral plexus is essential for maintaining the proper functioning of the lower limbs, pelvis, and perineum. It enables the nervous system to respond to changes in the environment and internal conditions, ensuring the body’s overall well-being.
The Sciatic Nerve and the Sacral Plexus
Anatomy of the Sciatic Nerve
The sciatic nerve, often referred to as the “great sciatic nerve,” is the largest nerve in the body and plays a significant role in the functioning of the sacral plexus. It originates from the sacral plexus, a complex network of nerves formed by the fusion of nerve roots L4 to S3. This intricate web of nerves is responsible for the innervation of the lower limbs and pelvic region.
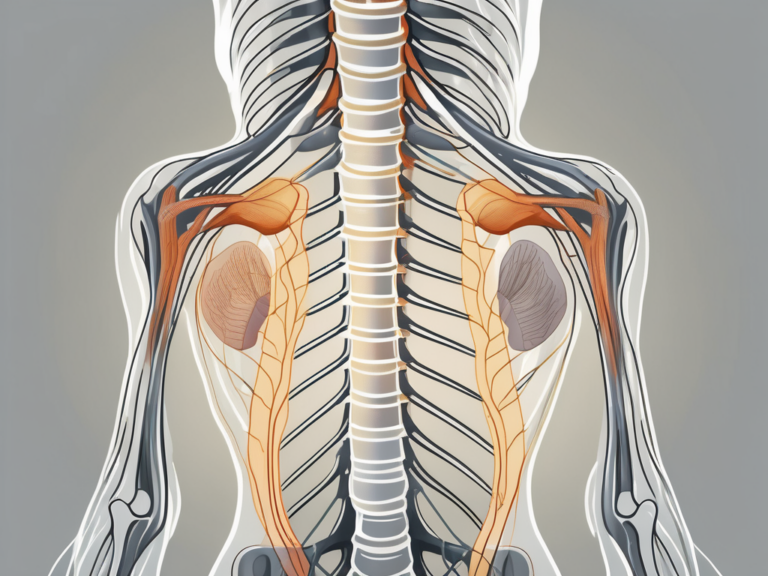
As the sciatic nerve descends down the leg, it branches out and divides into two major nerves: the tibial nerve and the common peroneal nerve. These branches are essential for the proper functioning of various muscles and sensory perception in the lower limb.
The tibial nerve, one of the branches of the sciatic nerve, innervates the posterior thigh muscles, including the hamstrings and the muscles of the leg and foot. It provides motor control and enables movements such as flexion of the knee and extension of the ankle. Additionally, the tibial nerve carries sensory information from the skin on the sole of the foot and the back of the leg.
On the other hand, the common peroneal nerve, the other branch of the sciatic nerve, supplies the anterior and lateral muscles of the leg. It is responsible for foot dorsiflexion, which allows us to lift the front of the foot, and foot eversion, which enables us to turn the sole of the foot outward. The common peroneal nerve also carries sensory information from the skin on the front and sides of the leg.
The sciatic nerve’s extensive distribution and its branches’ functions make it vital for various movements and functions of the lower limb. Without the proper functioning of the sciatic nerve and its connection to the sacral plexus, simple activities such as walking, running, and even standing would be compromised.
The Sciatic Nerve’s Connection to the Sacral Plexus
The sciatic nerve arises from the sacral plexus as a result of several nerve roots converging. This connection ensures that the nerve receives the necessary motor and sensory inputs from the sacral plexus and the broader nervous system. The sacral plexus, located in the pelvis, is a complex network of nerves that serves as a central hub for the lower limb’s innervation.
The sacral plexus consists of nerve roots originating from the spinal cord’s lower segments, specifically L4 to S3. These nerve roots merge and intertwine, forming the sciatic nerve, which then extends down the leg. The integration of multiple nerve roots within the sciatic nerve provides it with a diverse range of functions and allows it to transmit both motor and sensory signals efficiently.
Dysfunction in the sciatic nerve or the sacral plexus can result in conditions such as sciatica, a common and often debilitating condition. Sciatica is characterized by pain, weakness, or numbness in the lower back, buttocks, and legs. It can be caused by various factors, including herniated discs, spinal stenosis, or even muscle imbalances.
Understanding the intricate anatomy and connection between the sciatic nerve and the sacral plexus is crucial for diagnosing and treating conditions that affect this region. Medical professionals, such as neurologists and physiotherapists, rely on this knowledge to develop effective treatment plans and rehabilitation strategies to alleviate pain and restore proper function.
Other Nerves Connected to the Sacral Plexus
Pudendal Nerve and Its Role
The pudendal nerve is another significant nerve originating from the sacral plexus. It supplies the perineum, external genitalia, and anal region. The pudendal nerve plays a vital role in controlling voluntary movements of the pelvic floor muscles, as well as providing sensory innervation to these areas.
When it comes to voluntary movements of the pelvic floor muscles, the pudendal nerve is crucial in maintaining continence. It allows us to control the release of urine and feces, ensuring that we can hold it in until it is convenient to go to the bathroom. Additionally, the pudendal nerve is responsible for the contraction of the muscles during sexual activity, contributing to sexual pleasure and orgasm.
Damage or dysfunction of the pudendal nerve can lead to conditions such as pudendal neuralgia, which is characterized by chronic pain, tingling, or numbness in the perineal region. This condition can significantly impact a person’s quality of life, causing discomfort and affecting their ability to engage in daily activities. If you experience any discomfort in this area, it is essential to consult with a medical professional to receive an accurate diagnosis and appropriate treatment.
Superior and Inferior Gluteal Nerves Explained
Two other nerves connected to the sacral plexus are the superior and inferior gluteal nerves. These nerves innervate specific muscles in the buttocks region, namely the gluteus maximus, gluteus medius, and gluteus minimus. They play essential roles in controlling hip movement, maintaining balance, and supporting the body’s weight during standing and walking.
The gluteus maximus, the largest muscle in the buttocks, is responsible for extending the hip joint and allowing us to stand up from a seated position or climb stairs. The gluteus medius and gluteus minimus, located on the side of the hip, help stabilize the pelvis during walking and running, preventing excessive tilting or swaying.
If you experience any difficulties with muscle control in the gluteal region or notice changes in your gait or balance, it is advisable to seek medical advice. A healthcare professional can evaluate your symptoms and determine if further investigation or treatment is necessary. Proper functioning of the gluteal muscles is crucial for maintaining mobility and preventing falls, especially in older adults.
Disorders Related to the Sacral Plexus
The sacral plexus is a complex network of nerves located in the lower back and pelvis. It is responsible for transmitting signals between the spinal cord and the lower limbs, pelvis, and perineum. When the sacral plexus is affected by a disorder, it can lead to a variety of symptoms and impact an individual’s mobility and quality of life.
Common Symptoms of Sacral Plexus Disorders
Sacral plexus disorders can manifest in various ways, with symptoms depending on the specific condition and underlying cause. One of the most common symptoms is pain, which can range from mild discomfort to severe and debilitating. The pain may be localized to the lower back, buttocks, or legs, or it may radiate to other areas of the body.
In addition to pain, individuals with sacral plexus disorders may experience numbness or tingling sensations in the lower limbs, pelvis, or perineum. This can lead to a loss of sensation and affect the individual’s ability to perceive touch, temperature, or pressure in these areas.
Weakness or loss of function in the lower limbs is another common symptom of sacral plexus disorders. This can make it difficult to walk, stand, or perform daily activities that require lower body strength. It may also affect bladder and bowel control, leading to urinary or fecal incontinence.
If you experience any of these symptoms, it is crucial to consult with a healthcare professional for a proper diagnosis. They can conduct a thorough evaluation, which may include physical examinations, imaging studies, or nerve conduction tests to determine the underlying cause and recommend appropriate treatment options.
Treatment Options for Sacral Plexus Disorders
Treatment for sacral plexus disorders depends on the underlying cause and the severity of symptoms experienced. In many cases, non-invasive approaches are recommended as a first-line treatment. Physical therapy can help improve strength, flexibility, and mobility in the affected areas. Pain management techniques, such as medications or nerve blocks, may also be used to alleviate discomfort and improve quality of life.
Lifestyle modifications can also play a significant role in managing sacral plexus disorders. This may include weight management, regular exercise, and avoiding activities that exacerbate symptoms. Assistive devices, such as braces or canes, may be recommended to provide support and improve mobility.
In more severe cases or when conservative treatments are ineffective, surgical intervention may be indicated. Surgery aims to address the underlying cause, relieve pressure on affected nerves, or repair damaged structures. Procedures such as nerve decompression, nerve grafting, or nerve transfer may be performed to restore function and alleviate symptoms.
However, it is important to note that every case is unique, and treatment options should be discussed with a healthcare professional who can provide tailored advice based on an individual’s specific situation. They will consider factors such as the individual’s overall health, the severity of symptoms, and the potential risks and benefits of each treatment option.
Future Research on the Sacral Plexus
Current Challenges in Sacral Plexus Research
Despite significant progress, there are still many challenges in the field of sacral plexus research. One of the primary difficulties is the complexity of the nervous system and its intricate connections. Understanding the functions and interactions of the sacral plexus within this complex network requires further investigation and technological advancements.
Additionally, the scarcity of specific treatments for sacral plexus disorders highlights the need for continued research. Developing novel treatment strategies and improving the accuracy of diagnostic techniques are crucial goals for future studies in this area.
Potential Breakthroughs in Understanding the Sacral Plexus
Advancements in technology, such as imaging techniques and neural mapping, hold great promise for further understanding the intricacies of the sacral plexus. These breakthroughs could provide valuable insights into the diagnosis and treatment of sacral plexus disorders, helping to improve patients’ outcomes and quality of life.
Moreover, ongoing research into neuroplasticity and nerve regeneration may offer potential solutions for individuals affected by sacral plexus injuries or dysfunction. By enhancing our understanding of nerve regeneration and promoting functional recovery, scientists and clinicians hope to develop innovative therapies that can restore normal nervous system function.
Conclusion
The sacral plexus is a fascinating and essential component of the nervous system. It supplies innervation to the lower limbs, pelvis, and perineum, playing a vital role in motor and sensory functions. Understanding the complex anatomy, functions, and interactions of the sacral plexus is key to comprehending various disorders and developing effective treatment strategies.
If you suspect any issues related to the sacral plexus or experience symptoms such as pain, weakness, or sensory changes in the lower limbs or pelvis, it is crucial to consult with a healthcare professional. They can provide accurate diagnosis, recommend appropriate treatments, and guide you on your journey toward optimal health and well-being.