When Is a Sacral Nerve Stimulation Removed?
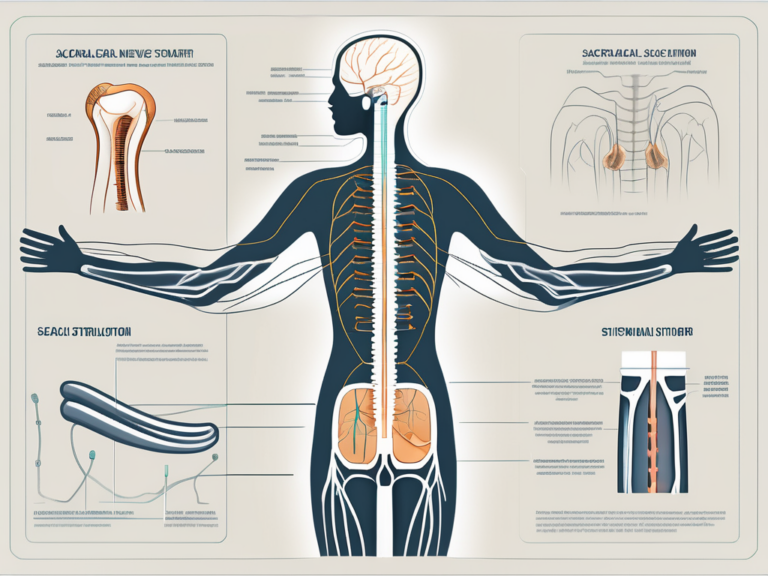
Sacral nerve stimulation is a medical treatment used to manage certain conditions, such as urinary and fecal incontinence, overactive bladder, and chronic pelvic pain. While this therapy can be beneficial for many individuals, there may come a time when a patient and their healthcare provider decide that the device should be removed. In this article, we will explore the reasons why sacral nerve stimulation may be removed, the removal process, and what life may be like after the removal.
Understanding Sacral Nerve Stimulation
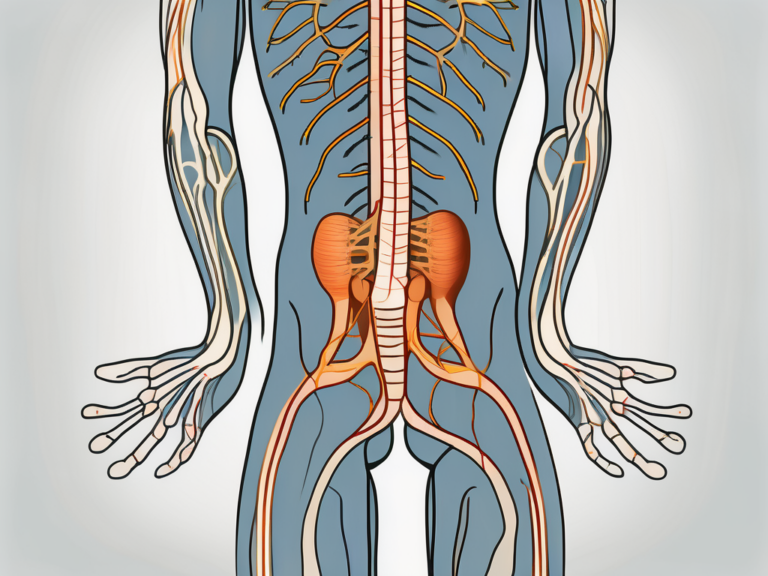
Before delving into the removal of sacral nerve stimulation, let’s first understand what it is and why it is used. Sacral nerve stimulation, also known as sacral neuromodulation, involves implanting a small device under the skin to regulate the activity of the sacral nerves that control the bladder, bowels, and pelvic floor muscles. By modulating these nerves, sacral nerve stimulation can help alleviate various symptoms and improve quality of life for many patients.
The sacral nerves, located in the lower part of the spine, play a crucial role in the proper functioning of the bladder, bowels, and pelvic floor muscles. When these nerves are not functioning optimally, it can lead to a range of problems, including urinary and fecal incontinence, urinary retention, and pelvic pain. Sacral nerve stimulation aims to restore the normal function of these nerves and improve the overall control of the bladder and bowels.
The Purpose of Sacral Nerve Stimulation
The primary goal of sacral nerve stimulation is to provide symptom relief and enhance bladder and bowel control. This therapy is typically recommended for individuals who have not responded to more conservative treatment options, such as medications, behavioral modifications, or physical therapy.
For patients suffering from overactive bladder, sacral nerve stimulation can help reduce the frequency and urgency of urination, as well as decrease episodes of urinary incontinence. Similarly, for individuals with fecal incontinence, this therapy can improve bowel control and reduce embarrassing accidents. By targeting the sacral nerves directly, sacral nerve stimulation offers a more targeted and effective approach to managing these conditions.
The Procedure of Sacral Nerve Stimulation
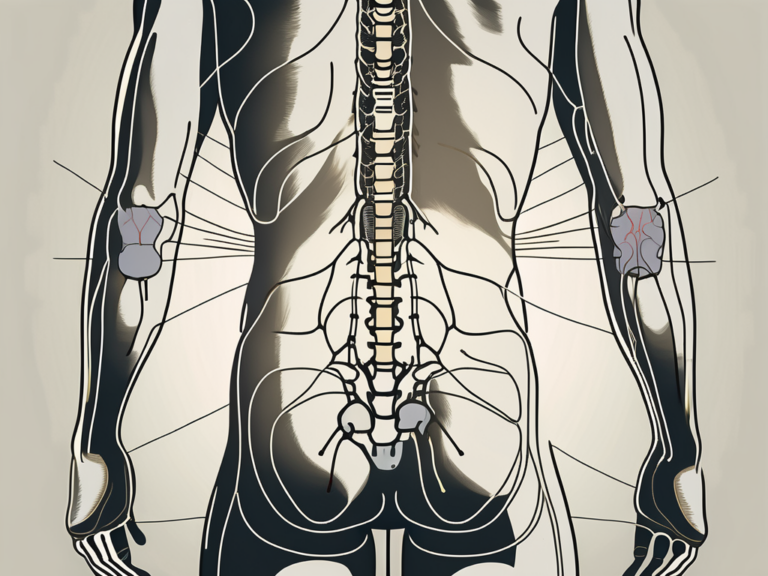
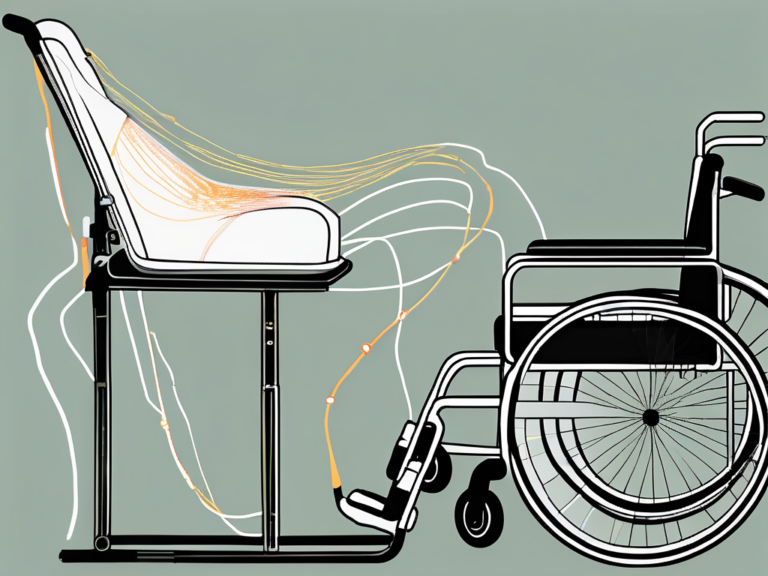
Implanting a sacral nerve stimulation device involves a surgical procedure performed under anesthesia. The procedure begins with the placement of a slender lead near the sacral nerves. This lead is carefully positioned to ensure optimal contact with the nerves and effective delivery of electrical impulses.
Once the lead is in place, a small generator is implanted under the skin, usually in the upper buttock or lower abdomen. This generator serves as the power source for the sacral nerve stimulation system and is responsible for delivering the electrical impulses to the sacral nerves. The generator is connected to the lead through a thin wire, which is also implanted under the skin.
Following the surgery, the device is programmed to deliver electrical impulses to the sacral nerves. The programming can be adjusted as needed over time to optimize the therapy and achieve the desired results. Patients may need to work closely with their healthcare provider to fine-tune the settings and find the most effective stimulation parameters for their specific condition.
It is important to note that sacral nerve stimulation is a reversible therapy. If a patient no longer wishes to continue with the treatment or experiences any complications, the device can be removed through a surgical procedure. The removal procedure is typically straightforward and involves disconnecting the lead and generator from the sacral nerves and removing them from the body.
In conclusion, sacral nerve stimulation is a valuable therapy option for individuals who have not found relief from more conservative treatments for bladder and bowel control issues. By understanding the purpose and procedure of sacral nerve stimulation, patients can make informed decisions about their healthcare and explore this innovative treatment approach.
Reasons for Sacral Nerve Stimulation Removal
While sacral nerve stimulation can be an effective treatment option for many individuals, there are situations where removal may be necessary. Let’s explore some of the reasons why sacral nerve stimulation may be removed.
Ineffectiveness of the Treatment
Sometimes, sacral nerve stimulation may not provide the desired level of symptom relief or improvement. Each individual responds differently to this therapy, and it is essential to manage expectations accordingly. If a patient does not experience significant improvement in their symptoms after a reasonable trial period, their healthcare provider may discuss the possibility of removing the device.
For example, consider a patient named Sarah who has been struggling with chronic pelvic pain for several years. She decides to try sacral nerve stimulation as a potential solution. However, despite undergoing the treatment for several months, Sarah does not notice a significant reduction in her pain levels. After consulting with her healthcare provider, they mutually agree that removing the device would be the best course of action for Sarah’s case.
Complications and Risks
Although the risks associated with sacral nerve stimulation are generally low, there can be potential complications. These can include infection, lead migration, pain, discomfort, or irritation at the site of the device, and rare instances of nerve damage. In some cases, complications may be severe enough to warrant the removal of the device to prevent further harm or alleviate ongoing discomfort.
Let’s consider the case of John, who underwent sacral nerve stimulation to manage his overactive bladder. Unfortunately, he developed an infection at the site of the device, leading to persistent pain and discomfort. Despite attempts to treat the infection, it became clear that removing the device was necessary to prevent further complications and ensure John’s well-being.
Patient’s Personal Decision
Ultimately, the decision to remove sacral nerve stimulation rests with the patient. For various personal reasons, a patient may choose to discontinue this treatment. It is important for individuals to have open and honest discussions with their healthcare provider to determine if removal is the right course of action and to consider alternative treatment options that may better suit their needs.
Take the case of Michael, who has been using sacral nerve stimulation to manage his urinary incontinence. While the treatment initially provided some relief, Michael finds that it interferes with his daily activities and affects his quality of life. After careful consideration and discussions with his healthcare provider, Michael decides to have the device removed to explore other treatment options that align better with his lifestyle and preferences.
It is crucial to recognize that the decision to remove sacral nerve stimulation is a personal one, and patients should feel empowered to make choices that best suit their individual circumstances and needs.
The Removal Process of Sacral Nerve Stimulation
If the decision is made to remove sacral nerve stimulation, the process typically involves several steps. Let’s explore what patients can expect during the removal process.
When it comes to the removal of sacral nerve stimulation, patients can find comfort in knowing that the procedure is generally less complex and invasive than the initial implantation. However, it is still important for healthcare providers to take certain precautions to ensure a successful removal.
Pre-removal Preparations
Before the removal procedure, a healthcare provider will evaluate the patient’s overall health and review their medical history. This assessment is crucial to ensure that the patient is in a suitable condition for the surgical removal. In some cases, additional tests may be ordered to assess the patient’s nerve function and overall well-being.
In preparation for the removal, imaging tests such as X-rays or MRIs may be performed to assess the position and condition of the device and associated leads. These tests provide valuable information to the healthcare team, allowing them to plan the removal procedure with precision and accuracy.
Furthermore, patients may be advised to discontinue certain medications or adjust their dosages prior to the removal. This is done to minimize any potential risks or complications during the procedure. It is important for patients to follow these instructions diligently and communicate any concerns or questions they may have with their healthcare provider.
The Surgical Procedure
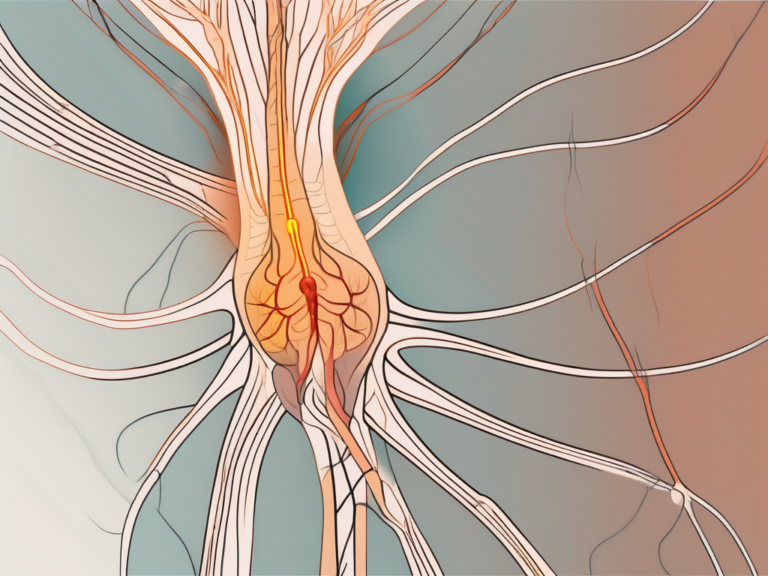
The removal procedure for sacral nerve stimulation begins with the patient being placed under anesthesia to ensure their comfort and safety throughout the surgery. Once the patient is properly sedated, the healthcare provider will proceed with the removal process.
A small incision is made near the location of the generator, which is typically placed in the lower back or buttock area. The healthcare provider carefully disconnects the leads from the nerves, ensuring minimal disruption to the surrounding tissues. Special care is taken to avoid any damage to the nerves or other structures in the area.
After the leads have been disconnected, the healthcare provider gently removes the device from the body. This delicate process requires precision and expertise to prevent any complications or injuries. Once the device has been successfully removed, the incision is closed with stitches or surgical glue, ensuring proper wound closure and minimizing the risk of infection.
Post-removal Care and Recovery
Following the removal of sacral nerve stimulation, patients may experience some soreness, bruising, or swelling around the incision site. These are normal side effects of the surgery and can be managed with pain medications and ice packs. It is important for patients to communicate any excessive pain or concerning symptoms to their healthcare provider.
Healthcare providers will provide specific instructions on how to care for the incision site, including proper wound care and hygiene practices. Patients should follow these guidelines diligently to promote healing and reduce the risk of infection. It is essential to give the body time to recover and gradually resume normal activities.
During the recovery period, patients may have follow-up appointments with their healthcare provider to monitor their progress and address any concerns. These appointments allow the healthcare team to ensure that the removal procedure was successful and that the patient is healing properly.
It is important for patients to be patient with their recovery process, as it may take some time for the body to fully heal and adjust after the removal of sacral nerve stimulation. By following the guidance of their healthcare provider and taking proper care of themselves, patients can increase their chances of a smooth recovery and a successful outcome.
Life After Sacral Nerve Stimulation Removal
After the removal of sacral nerve stimulation, individuals may experience physical, emotional, and psychological adjustments. Let’s explore some of these potential changes and considerations.
Physical Adjustments
Depending on the underlying condition being treated, individuals may need to explore alternative treatment options to manage their symptoms after sacral nerve stimulation removal. This can include medications, physical therapy, behavioral modifications, or other therapies recommended by their healthcare provider. It is important to work closely with a healthcare team to find the most suitable approach for each individual.
For some individuals, the removal of sacral nerve stimulation may result in a gradual return of symptoms. This can be a challenging adjustment, as they may have become accustomed to the relief provided by the device. It is important to monitor symptoms closely and communicate any changes to the healthcare team.
In some cases, individuals may find that alternative treatments or therapies are just as effective, if not more so, than sacral nerve stimulation. For example, physical therapy exercises and techniques can help strengthen the pelvic floor muscles and improve bladder or bowel control. Behavioral modifications, such as bladder training or dietary changes, may also play a significant role in managing symptoms.
Emotional and Psychological Implications
Removing sacral nerve stimulation may bring about emotional and psychological changes. Some individuals may experience feelings of disappointment, frustration, or anxiety about the potential return of symptoms. It can be helpful to seek support from healthcare professionals, loved ones, or support groups to navigate these emotional challenges and develop strategies for coping and adapting to life without the device.
It is important to remember that adjusting to life without sacral nerve stimulation is a process that takes time. It is normal to have mixed emotions and concerns about the future. Engaging in activities that promote relaxation and stress reduction, such as meditation, yoga, or hobbies, can be beneficial in managing these emotions.
Additionally, counseling or therapy sessions can provide a safe space to discuss fears, frustrations, and any other emotional challenges that may arise during this transition. A mental health professional can help individuals develop coping mechanisms and provide guidance on how to navigate the emotional and psychological implications of sacral nerve stimulation removal.
Alternative Treatments and Therapies
After the removal of sacral nerve stimulation, exploring alternative treatments or therapies may be necessary. Healthcare providers can help individuals explore other options tailored to their specific needs and circumstances. It is important to remember that what works for one person may not work for another, so patience and open-mindedness are key when considering alternative approaches.
Some alternative treatments that individuals may consider include acupuncture, herbal remedies, biofeedback, or electrical stimulation therapy. These approaches aim to address symptoms and improve overall well-being. It is crucial to consult with a healthcare professional before starting any alternative treatment to ensure its safety and effectiveness.
Furthermore, participating in clinical trials or research studies may be an option for individuals seeking alternative treatments. These studies can provide access to innovative therapies and allow individuals to contribute to the advancement of medical knowledge in the field of sacral nerve stimulation and related conditions.
It is crucial to note that the information provided in this article is for informational purposes only and should not be considered medical advice. If you are considering the removal of sacral nerve stimulation or have any concerns about your treatment, it is recommended to consult with a qualified healthcare professional who can assess your individual situation and provide guidance based on your specific needs and medical history.
In conclusion, the removal of sacral nerve stimulation can occur for various reasons, such as ineffectiveness, complications, or personal choice. If removal is deemed necessary, patients can expect a relatively straightforward procedure followed by a period of care and recovery. It is essential to consider alternative treatment options and address the physical, emotional, and psychological adjustments that may arise. Consulting with a healthcare professional is vital to ensure the best course of action for each individual’s unique circumstances and needs.