How Many Patients Have Been Paralyzed by a Sacral Nerve Stimulator?
Sacral nerve stimulation (SNS) is a medical procedure that has shown promise in treating various conditions, but concerns have been raised regarding the occurrence of paralysis in some patients. In this article, we will delve into the topic of paralysis associated with sacral nerve stimulators, exploring the procedure, analyzing statistics, discussing risk factors, and examining the medical community’s response.
Understanding Sacral Nerve Stimulation
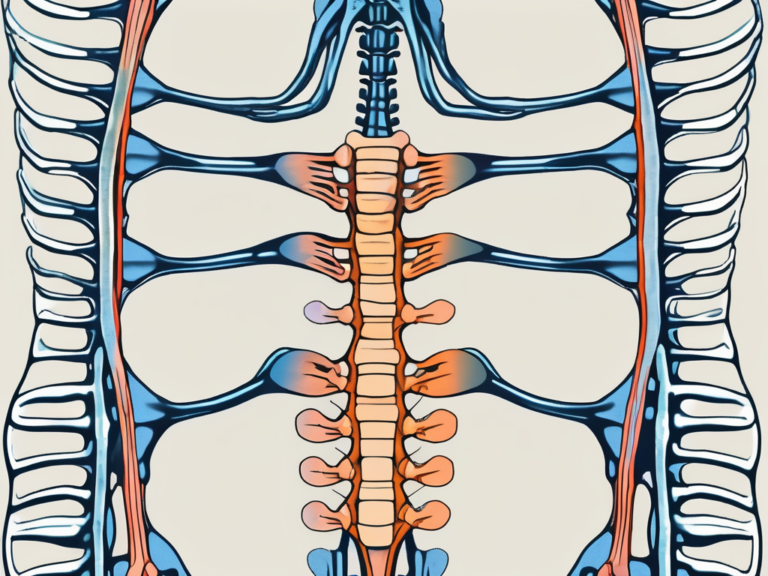
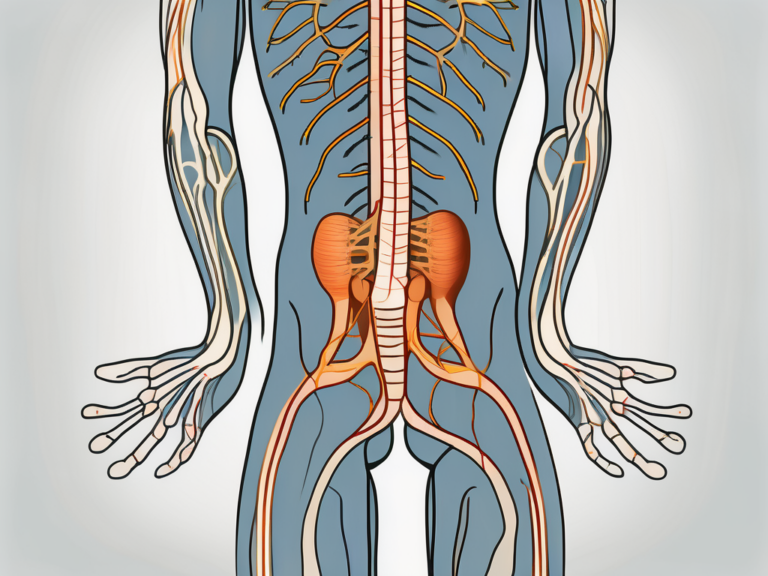
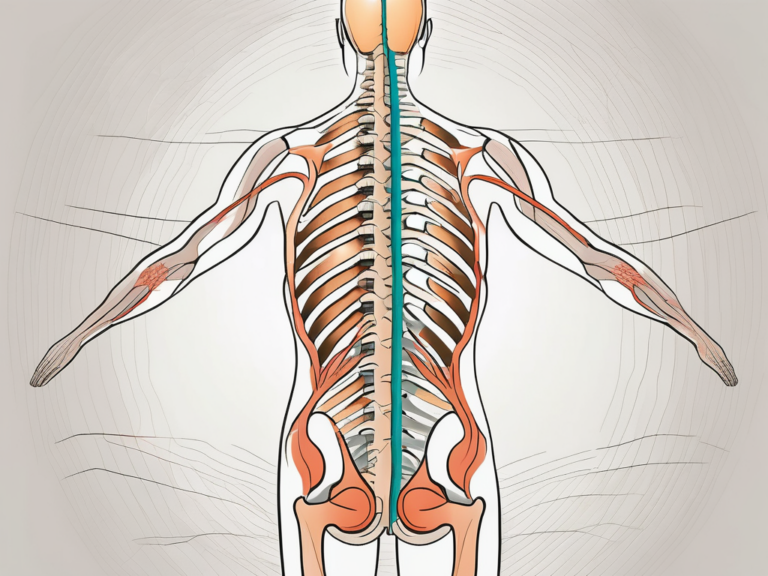
Before addressing the issue of paralysis, it is crucial to understand the purpose and procedure of sacral nerve stimulation. SNS is a treatment method primarily used for individuals with urinary and bowel dysfunction. It involves the placement of a device near the sacral nerves, which regulate bladder and bowel control.
The Purpose of Sacral Nerve Stimulators
The primary purpose of sacral nerve stimulation is to improve bladder and bowel function in patients who have not responded to other treatments. By directly modulating the sacral nerve signals, SNS aims to restore control and alleviate symptoms such as urinary or fecal incontinence.
Urinary incontinence is a common condition that can significantly impact a person’s quality of life. It can lead to embarrassment, social isolation, and a loss of independence. Sacral nerve stimulation offers hope to those who have not found relief from traditional treatments like medication or physical therapy.
Bowel dysfunction, including fecal incontinence, can also have a profound effect on a person’s well-being. It can cause feelings of shame and anxiety, making it difficult for individuals to engage in social activities or maintain a normal daily routine. Sacral nerve stimulation provides a potential solution for those struggling with these issues.
By targeting the sacral nerves, which play a crucial role in controlling bladder and bowel function, sacral nerve stimulators offer a unique approach to treating these conditions. The electrical impulses delivered by the device help to restore proper nerve signaling, allowing patients to regain control over their bodily functions.
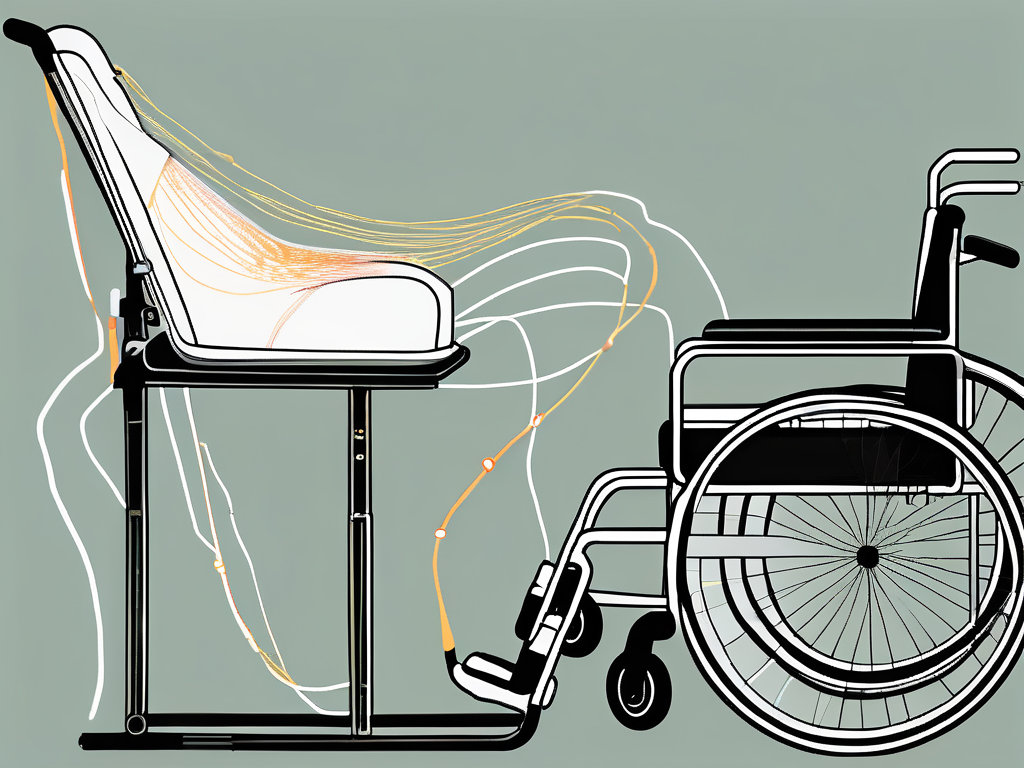
The Procedure of Sacral Nerve Stimulation
The procedure involves the implantation of a small device under the patient’s skin. This device is connected to leads that are placed near the sacral nerves through a minimally invasive surgery. Once implanted, the device delivers mild electrical impulses to the nerves, enabling better control over bladder and bowel functions.
During the surgery, the patient is typically placed under general anesthesia to ensure their comfort. The surgeon makes small incisions near the sacral nerves and carefully inserts the leads into the targeted area. The leads are then connected to the device, which is usually implanted in the buttock or lower abdomen.
After the surgery, patients may experience some discomfort or soreness at the incision sites. However, this can usually be managed with over-the-counter pain medication. It is important to follow the surgeon’s post-operative instructions, which may include avoiding strenuous activities and keeping the incision sites clean and dry.
Once the device is activated, patients may need to undergo a programming session to optimize its settings. This involves working closely with a healthcare professional who will adjust the electrical impulses to achieve the best results. The programming session may be done in a clinic or hospital setting and can be tailored to the individual’s specific needs.
It is important to note that sacral nerve stimulation is not a cure for urinary or bowel dysfunction. However, it can provide significant improvement in symptoms and quality of life for many patients. Regular follow-up appointments with the healthcare team are essential to monitor progress and make any necessary adjustments to the device settings.
In conclusion, sacral nerve stimulation is a valuable treatment option for individuals with urinary and bowel dysfunction. By directly targeting the sacral nerves, this procedure aims to restore control and alleviate symptoms, offering hope and improved quality of life for those who have not found relief from other treatments.
The Link Between Sacral Nerve Stimulation and Paralysis
While sacral nerve stimulation has shown positive outcomes for many patients, there have been reports of paralysis occurring in some cases. It is essential to explore the medical theories behind this occurrence and examine documented cases to gain a comprehensive understanding of the issue.
Medical Theories Behind the Paralysis
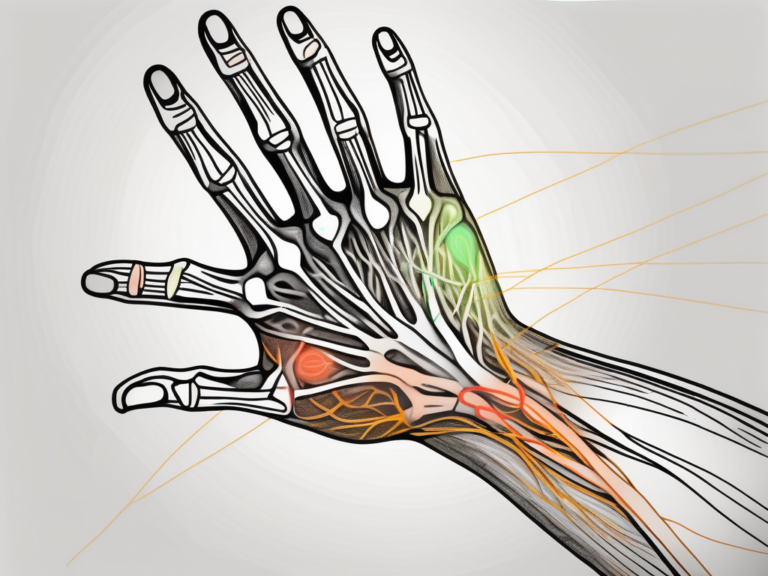
Medical professionals have put forth several theories to explain the occurrence of paralysis in some patients undergoing sacral nerve stimulation. One theory suggests that direct damage to the nerves during the implantation procedure may lead to paralysis. This theory is based on the fact that the sacral nerves are delicate and can be easily damaged during surgery. If the nerves are injured, it can result in paralysis or loss of function in the affected area.
Another theory posits that the electrical stimulation itself may cause adverse effects, including paralysis, in rare cases. The electrical impulses delivered to the sacral nerves can potentially disrupt the normal functioning of the nerves, leading to paralysis. This theory is still being investigated, and more research is needed to determine the exact mechanism by which electrical stimulation can cause paralysis.
Reported Cases of Paralysis Post-Procedure
While paralysis is considered a rare complication of sacral nerve stimulation, there have been documented cases. It is important to note that these cases represent a small percentage of the overall number of patients who undergo this procedure.
One documented case involved a 45-year-old woman who underwent sacral nerve stimulation for the treatment of urinary incontinence. Following the procedure, she experienced sudden paralysis in her lower limbs. Further investigation revealed that the paralysis was caused by nerve damage during the implantation process. The patient underwent additional surgeries to repair the damaged nerves and regain function in her legs.
Another reported case involved a 62-year-old man who developed paralysis in his left arm after sacral nerve stimulation for the treatment of chronic pelvic pain. The paralysis was attributed to the electrical stimulation itself, as no direct nerve damage was observed during the procedure. The patient underwent physical therapy and rehabilitation to regain strength and mobility in his arm.
These cases highlight the importance of careful patient selection and thorough pre-operative evaluation in minimizing the risk of paralysis following sacral nerve stimulation. It is crucial for medical professionals to assess the potential benefits and risks of the procedure on a case-by-case basis and inform patients about the possibility of paralysis as a rare complication.
Analyzing the Statistics of Paralysis in Sacral Nerve Stimulation Patients
To gain a clearer understanding of the prevalence of paralysis related to sacral nerve stimulation, statistical analysis can provide valuable insights. Examining global statistics and considering the age and gender distribution of paralysis cases can help assess the overall risk associated with the procedure.
Global Statistics on Paralysis Cases
Statistical data on paralysis cases post-sacral nerve stimulation can help us evaluate the scope of the issue. Collecting and analyzing data from different regions across the globe can provide a broader perspective on the occurrence of paralysis in relation to the procedure.
When analyzing global statistics, it is important to consider various factors that may contribute to the prevalence of paralysis. These factors can include the availability and accessibility of healthcare facilities, the quality of surgical procedures, and the overall health and lifestyle of the population. By examining these variables, researchers can gain a comprehensive understanding of the global paralysis statistics related to sacral nerve stimulation.
Furthermore, it is crucial to compare the paralysis rates between different countries and regions. This comparison can help identify any geographical patterns or disparities in the occurrence of paralysis. Factors such as cultural practices, genetic predispositions, and variations in healthcare systems can all contribute to differences in paralysis rates. By analyzing these variations, medical professionals can develop targeted interventions and strategies to reduce the risk of paralysis in sacral nerve stimulation patients.
Age and Gender Distribution in Paralysis Cases
Understanding the age and gender distribution of paralysis cases can shed light on potential risk factors associated with sacral nerve stimulation. By identifying patterns and demographic trends, medical professionals can develop informed guidelines to manage these risks effectively.
Age plays a significant role in the occurrence of paralysis post-sacral nerve stimulation. Research has shown that older individuals may be more susceptible to paralysis due to factors such as reduced muscle strength, slower healing processes, and age-related degenerative changes. By analyzing the age distribution of paralysis cases, healthcare providers can tailor their treatment plans and post-operative care to address the specific needs of different age groups.
Gender is another important factor to consider when analyzing paralysis cases. Studies have suggested that there may be gender differences in the risk of paralysis following sacral nerve stimulation. Hormonal variations, anatomical differences, and disparities in muscle mass and strength between males and females can all contribute to these gender-specific risks. By understanding these differences, medical professionals can develop personalized approaches to minimize the risk of paralysis in both male and female patients.
In conclusion, statistical analysis of paralysis cases related to sacral nerve stimulation provides valuable insights into the prevalence and risk factors associated with the procedure. By examining global statistics and considering the age and gender distribution of paralysis cases, medical professionals can develop evidence-based guidelines and interventions to ensure the safety and well-being of sacral nerve stimulation patients.
The Risk Factors and Precautions
While paralysis is a rare occurrence, it is essential to identify potential risk factors and take appropriate precautions to minimize the chances of this complication. Identifying and addressing these factors can help enhance patient safety and ensure positive outcomes.
Paralysis, a condition characterized by the loss of muscle function in certain parts of the body, can have severe consequences on a patient’s quality of life. It can result in the loss of mobility, independence, and the ability to perform daily activities. Therefore, understanding the risk factors and implementing precautions is crucial in preventing this debilitating condition.
Identifying Potential Risk Factors
Medical experts are constantly researching and identifying potential risk factors that may contribute to paralysis in some patients. Factors such as the patient’s medical history, anatomy, and underlying conditions are being studied to better understand their correlation with the occurrence of paralysis post-sacral nerve stimulation.
Medical history plays a significant role in determining the likelihood of paralysis. Patients with a history of neurological disorders, spinal cord injuries, or previous surgeries in the pelvic region may be at a higher risk. Additionally, the anatomical structure of the patient’s spine and nerves can also influence the susceptibility to paralysis.
Furthermore, underlying conditions such as diabetes, autoimmune disorders, or infections can weaken the body’s immune system and make it more vulnerable to complications. These factors are carefully assessed by medical professionals to identify patients who may be at a higher risk of paralysis.
Precautions to Minimize Risks
Medical professionals are adopting precautionary measures to minimize the risks associated with sacral nerve stimulation. These may include thorough patient evaluations, meticulous surgical techniques, and close monitoring post-procedure. Following these precautions can help reduce the occurrence of complications, including paralysis.
Prior to the procedure, a comprehensive evaluation is conducted to assess the patient’s overall health and identify any potential risk factors. This evaluation may involve a detailed medical history review, physical examinations, and diagnostic tests to ensure that the patient is a suitable candidate for sacral nerve stimulation.
During the surgical procedure, medical professionals employ meticulous techniques to minimize the risk of nerve damage and subsequent paralysis. Advanced imaging technologies, such as fluoroscopy, may be used to guide the placement of electrodes with precision and accuracy. Surgeons take great care to avoid any unnecessary trauma to the nerves and surrounding tissues.
Post-procedure, close monitoring of the patient’s condition is essential to detect any signs of complications promptly. Regular follow-up appointments allow medical professionals to assess the patient’s progress, address any concerns, and make necessary adjustments to the treatment plan if needed.
In conclusion, while paralysis is a rare complication of sacral nerve stimulation, it is crucial to understand the potential risk factors and implement appropriate precautions. Medical professionals are continuously researching and refining their techniques to minimize the occurrence of paralysis and ensure the safety and well-being of their patients.
The Medical Community’s Response
The occurrence of paralysis related to sacral nerve stimulation has prompted responses from neurologists and surgeons, leading to changes in the approach to this procedure. It is important to understand the perspectives of the medical community to stay informed about the current practices in the field.
Neurologists and surgeons, upon recognizing the occurrence of paralysis, have expressed concerns and conducted investigations into the matter. They have collaborated to review cases, identify potential causes, and share findings to improve the safety and efficacy of sacral nerve stimulation.
One of the key reactions from the medical community has been the establishment of dedicated research teams and task forces to specifically address the issue of paralysis associated with sacral nerve stimulation. These teams consist of experts from various disciplines, including neurology, surgery, and biomedical engineering. Their collective expertise and collaboration have been instrumental in understanding the underlying mechanisms and developing strategies to mitigate the risk of paralysis.
Through extensive research and analysis, neurologists and surgeons have identified several potential factors that contribute to the occurrence of paralysis in some patients. These factors include the positioning of the electrodes, the intensity of stimulation, and individual patient characteristics. By gaining a deeper understanding of these factors, medical professionals have been able to refine and modify the surgical techniques and methodologies used in sacral nerve stimulation procedures.
The changes in sacral nerve stimulation practices have not only focused on the surgical aspect but also on preoperative and postoperative care. Neurologists and surgeons have emphasized the importance of thorough patient evaluation and risk assessment before proceeding with the procedure. This includes a comprehensive medical history review, physical examinations, and diagnostic tests to identify any potential contraindications or risk factors that may increase the likelihood of paralysis.
Furthermore, postoperative care has also been enhanced to closely monitor patients for any signs of paralysis or other complications. Regular follow-up visits, imaging studies, and functional assessments are conducted to ensure early detection and prompt intervention if any issues arise. This proactive approach has significantly improved patient outcomes and reduced the incidence of paralysis associated with sacral nerve stimulation.
In addition to these changes in practice, the medical community has also prioritized patient education and informed consent. Neurologists and surgeons now provide detailed information to patients about the potential risks and benefits of sacral nerve stimulation, including the rare possibility of paralysis. This allows patients to make well-informed decisions and actively participate in their own healthcare journey.
In conclusion, the occurrence of paralysis related to sacral nerve stimulation has sparked a comprehensive response from the medical community. Neurologists and surgeons have collaborated to investigate the causes and implement changes in surgical techniques and patient care. These efforts have not only improved the safety and efficacy of sacral nerve stimulation but also empowered patients with knowledge to make informed decisions about their treatment options.
The Future of Sacral Nerve Stimulation
As the medical community continues to address the concerns surrounding paralysis in SNS patients, research and technological advancements offer hope for a safer future. By embracing innovative approaches, emphasizing patient education, and encouraging informed consent, the field of sacral nerve stimulation is poised for further progress.
Technological Advancements to Reduce Risks
Ongoing research and development in the field of sacral nerve stimulation are focused on technological advancements that can minimize risks and maximize the efficacy of the procedure. These advancements may include improved implantable devices, optimized stimulation parameters, and enhanced surgical techniques.
The Role of Patient Education and Informed Consent
Empowering patients with knowledge about the potential risks and benefits of sacral nerve stimulation is paramount. Ensuring that patients are fully informed, actively involved in their treatment decisions, and aware of the available alternatives can help them make informed choices while consulting with their healthcare providers.
In conclusion, while the occurrence of paralysis related to sacral nerve stimulation is rare, it is essential to be aware of potential risks and remain informed about the ongoing efforts in the medical community to address this concern. Consulting with a medical professional is always advised for individuals considering sacral nerve stimulation or experiencing complications following the procedure. Through continued research, precautionary measures, and collaborative efforts, medical experts are working towards enhancing patient safety and improving the outcomes of this valuable treatment option.