What Doctor Treats Sacral Nerve Damage?
If you are experiencing symptoms of sacral nerve damage, it is important to consult with the right healthcare professional who can provide the appropriate diagnosis and treatment. In this article, we will discuss the different types of doctors involved in treating sacral nerve damage, the diagnostic procedures used to identify it, the available treatment options, the importance of follow-up care, and preventive measures and lifestyle adjustments that can support nerve health.
Understanding Sacral Nerve Damage
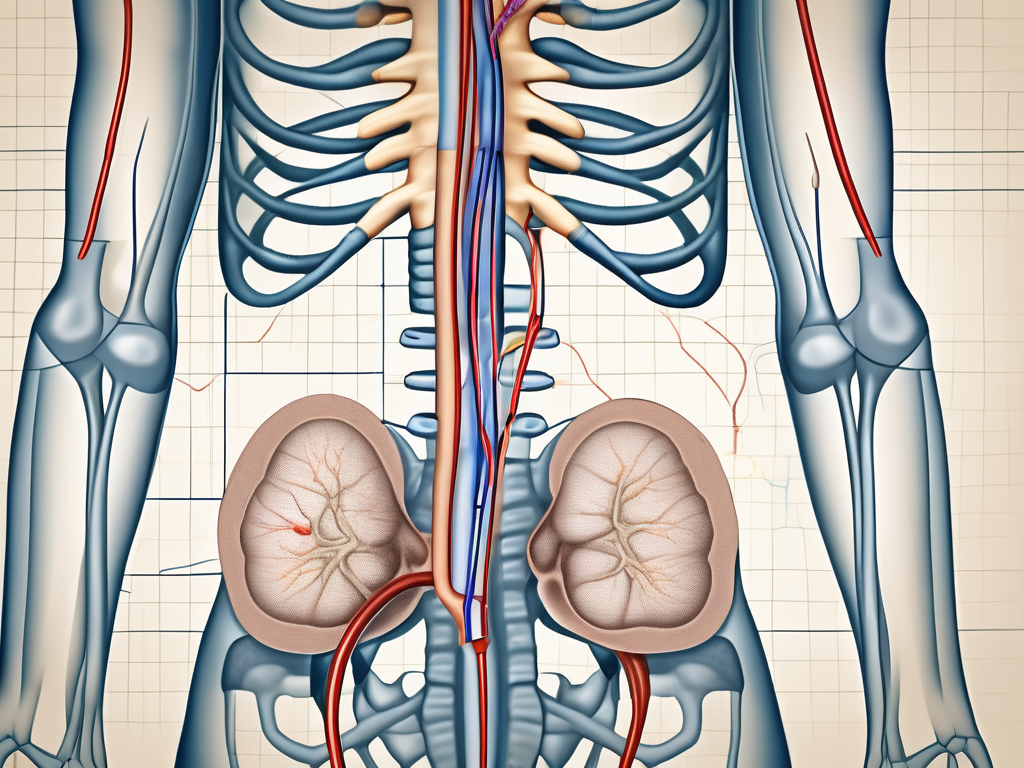
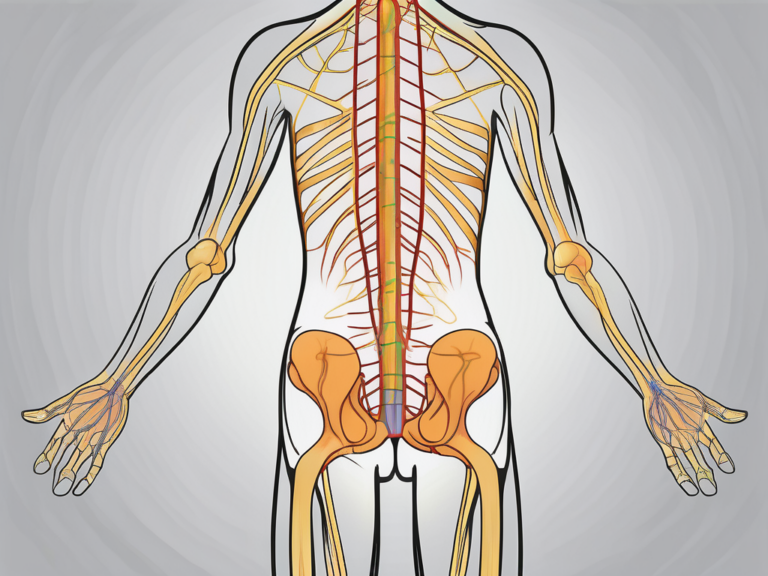
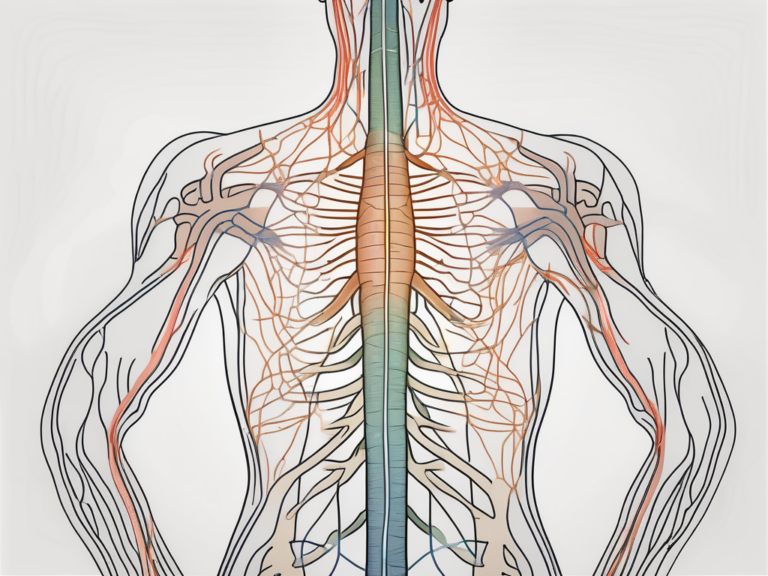
Sacral nerve damage refers to any injury or dysfunction affecting the sacral nerves, which are located in the lower part of the spinal cord. These nerves play a crucial role in transmitting signals between the brain and pelvic organs, muscles, and sensory areas of the lower abdomen and groin.
The sacral nerve is responsible for controlling various bodily functions, including bladder and bowel control, sexual function, and sensation in the pelvic area. It also assists in the proper functioning of the muscles in the legs, feet, and toes. When the sacral nerve is damaged, it can lead to a range of symptoms and complications.
One important aspect to understand about sacral nerve damage is the impact it can have on an individual’s quality of life. The loss of bladder and bowel control can be particularly challenging, as it can lead to embarrassment, social isolation, and a decreased sense of independence. Additionally, sexual dysfunction can have a profound effect on relationships and self-esteem.
The Role of the Sacral Nerve in the Body
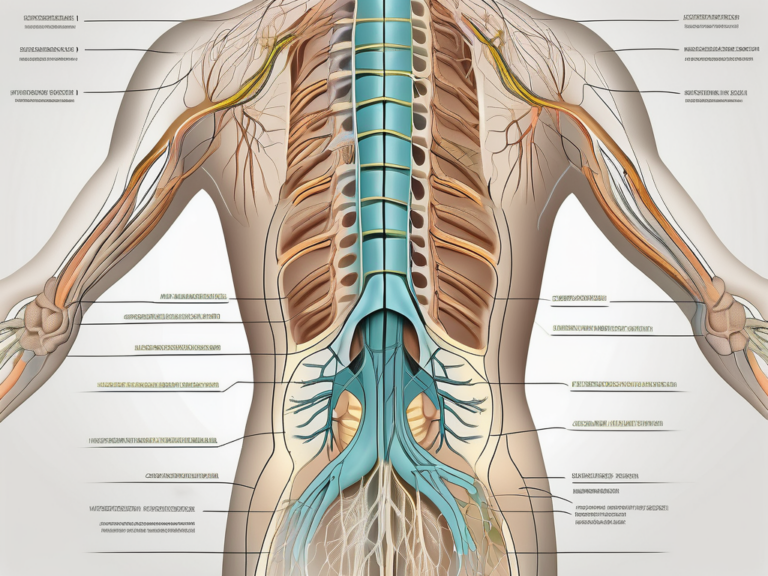
The sacral nerve is a complex network of nerves that branches out from the lower part of the spinal cord. It consists of five pairs of nerves, known as S1 to S5, which innervate different areas of the body. These nerves work together to ensure the proper functioning of the pelvic organs, muscles, and sensory areas.
For example, the sacral nerve plays a crucial role in controlling the muscles involved in urination and defecation. It sends signals from the brain to the bladder and bowel, instructing them to contract or relax at the appropriate times. This coordination allows for the efficient elimination of waste from the body.
In addition to its role in bladder and bowel control, the sacral nerve also plays a key role in sexual function. It is responsible for transmitting sensory information from the genitals to the brain, allowing for the experience of pleasure and arousal. It also controls the muscles involved in sexual activity, such as those responsible for erection and ejaculation in males.
Common Causes of Sacral Nerve Damage
There are several potential causes of sacral nerve damage, each with its own set of risk factors and complications. One common cause is trauma or injury to the lower back or pelvic region. This can occur as a result of a fall, car accident, or sports-related injury. The force of the impact can compress or damage the sacral nerves, leading to dysfunction.
Infections can also cause sacral nerve damage. Urinary tract infections and sexually transmitted infections, such as herpes or gonorrhea, can spread to the sacral nerves and cause inflammation or damage. This can result in pain, numbness, or other symptoms in the pelvic area.
Other medical conditions can also contribute to sacral nerve damage. For example, diabetes can cause nerve damage throughout the body, including the sacral nerves. Multiple sclerosis, an autoimmune disease that affects the central nervous system, can also lead to nerve damage in the sacral region.
Surgical complications can also result in sacral nerve damage. Procedures that involve the lower back or pelvic area, such as spinal surgery or pelvic surgery, carry a risk of nerve injury. This can occur due to accidental damage during the procedure or as a result of scar tissue formation.
Symptoms Indicating Sacral Nerve Damage
Signs of sacral nerve damage can vary depending on the location and severity of the injury. Common symptoms include pain or discomfort in the lower back or pelvic area, numbness or tingling in the legs, feet, or groin, muscle weakness or paralysis, urinary or bowel dysfunction, and sexual dysfunction.
It is important to note that the symptoms of sacral nerve damage can range from mild to severe, and may worsen over time if left untreated. In some cases, individuals may experience a loss of sensation or motor function in the affected areas, making it difficult to perform daily activities.
If you experience any of these symptoms, it is important to seek medical attention for a proper evaluation. A healthcare professional can perform a thorough examination, order diagnostic tests, and develop a treatment plan tailored to your specific needs. Early intervention is key to preventing further damage and improving outcomes.
The Different Types of Doctors Involved
When it comes to treating sacral nerve damage, there are several types of doctors who may be involved in your care. Each specialist brings unique expertise and knowledge to ensure comprehensive and effective treatment.
Neurologists and Sacral Nerve Damage
Neurologists are medical specialists who diagnose and treat disorders of the nervous system, including sacral nerve damage. They have extensive training in evaluating nerve function, performing neurological examinations, and interpreting diagnostic tests such as nerve conduction studies or electromyography.
When you visit a neurologist for sacral nerve damage, they will conduct a thorough assessment to determine the extent of the damage and identify any underlying causes. They will carefully evaluate your symptoms, medical history, and perform a physical examination focused on neurological function. This comprehensive approach helps them develop an accurate diagnosis and create an individualized treatment plan.
Based on their evaluation, neurologists may recommend non-surgical treatments such as physical therapy, pain management techniques, or medications to manage symptoms. They may also refer you to other specialists, such as orthopedic surgeons or rheumatologists, for further evaluation or treatment if necessary.
The Role of Orthopedic Surgeons
Orthopedic surgeons specialize in the musculoskeletal system and may be involved in the treatment of sacral nerve damage, particularly if there is an underlying orthopedic condition or injury that requires surgical intervention.
When you consult an orthopedic surgeon for sacral nerve damage, they will thoroughly assess your condition through a combination of physical examination, imaging studies, and other diagnostic tests. They will focus on identifying any structural abnormalities or injuries that may be causing or contributing to the nerve damage.
If surgery is deemed necessary, orthopedic surgeons can perform procedures to relieve pressure on the nerves or repair damaged structures. These may include spinal fusion, decompression surgery, or other specialized techniques tailored to your specific needs. Orthopedic surgeons work closely with other members of your healthcare team to ensure a comprehensive and coordinated approach to your treatment.
When to Consult a Rheumatologist
Rheumatologists are doctors who specialize in the diagnosis and treatment of conditions that affect the joints, muscles, and connective tissues. While sacral nerve damage is not typically within their primary scope of practice, they may be consulted if there is an underlying autoimmune condition contributing to nerve dysfunction.
When you see a rheumatologist for sacral nerve damage, they will conduct a detailed evaluation to identify any autoimmune conditions that may be affecting your nerves. They will review your medical history, perform a physical examination, and order relevant laboratory tests to assess your overall health and immune system function.
If an autoimmune condition is identified, the rheumatologist will work closely with you to manage the underlying condition and provide guidance on appropriate treatment options. This may involve a combination of medications, lifestyle modifications, and ongoing monitoring to ensure optimal control of the autoimmune disease and minimize nerve damage.
While rheumatologists may not be the primary doctors involved in the treatment of sacral nerve damage, their expertise in autoimmune conditions can be invaluable in managing the overall health of patients with underlying autoimmune disorders.
Diagnostic Procedures for Sacral Nerve Damage
When evaluating sacral nerve damage, healthcare professionals may utilize various diagnostic procedures to determine the cause and extent of the injury.
Sacral nerve damage can result from a variety of causes, including trauma, infections, tumors, or degenerative conditions. To accurately diagnose and treat this condition, healthcare professionals employ a range of diagnostic techniques.
Physical Examinations and Tests
A thorough physical examination is often the first step in evaluating sacral nerve damage. During this examination, healthcare professionals will assess your medical history, looking for any factors that may contribute to nerve damage, such as previous injuries or underlying medical conditions.
Additionally, a comprehensive neurological exam will be conducted to evaluate the functioning of the sacral nerves. This may involve assessing your reflexes, muscle strength, sensation, and coordination. By carefully examining these factors, doctors can identify any signs of nerve damage and determine the severity of the condition.
In some cases, healthcare professionals may order additional tests to further investigate the cause of the nerve damage. Blood tests can be conducted to rule out underlying conditions, such as diabetes or vitamin deficiencies, which can contribute to nerve damage. These tests can provide valuable information that helps guide the diagnostic process.
Imaging studies are another valuable tool in diagnosing sacral nerve damage. X-rays can provide a detailed view of the spine, allowing doctors to identify any structural abnormalities or fractures that may be affecting the sacral nerves. Magnetic Resonance Imaging (MRI) scans use powerful magnets and radio waves to create detailed images of the body’s internal structures. This non-invasive procedure can help identify abnormalities, such as herniated discs or spinal stenosis, which may be compressing the sacral nerves.
In some cases, Computed Tomography (CT) scans may also be used to visualize the affected area. CT scans combine X-ray images taken from different angles to create cross-sectional images of the body. This can provide healthcare professionals with a detailed view of the sacral nerves and surrounding structures, aiding in the diagnosis and treatment planning process.
Imaging Techniques for Sacral Nerve Damage
Imaging techniques play a crucial role in diagnosing sacral nerve damage. By providing detailed information about the spine and surrounding structures, these techniques help healthcare professionals formulate an appropriate treatment plan.
An MRI scan is particularly useful in identifying abnormalities that may be causing sacral nerve damage. This imaging technique uses a strong magnetic field and radio waves to create detailed images of the body’s internal structures. By visualizing the sacral nerves and surrounding tissues, an MRI scan can help doctors identify any compression or damage to the nerves.
In addition to MRI scans, other imaging techniques such as X-rays and CT scans can also be used to assess sacral nerve damage. X-rays provide a two-dimensional view of the spine, allowing doctors to identify any fractures or structural abnormalities that may be affecting the sacral nerves. CT scans, on the other hand, provide a more detailed view by combining multiple X-ray images taken from different angles. This can help healthcare professionals visualize the sacral nerves and surrounding structures in three dimensions, aiding in the diagnosis and treatment planning process.
Overall, the use of imaging techniques in diagnosing sacral nerve damage is essential. These non-invasive procedures provide valuable information about the extent of the injury, helping healthcare professionals determine the most appropriate course of treatment for each individual patient.
Treatment Options for Sacral Nerve Damage
The treatment of sacral nerve damage depends on the underlying cause, severity of the injury, and individual patient factors. Treatment options can range from non-surgical interventions to surgical procedures.
Medications and Non-Surgical Treatments
In many cases, nonsurgical treatments can help manage the symptoms associated with sacral nerve damage. Medications such as analgesics or anti-inflammatory drugs may be prescribed to alleviate pain or reduce inflammation. Physical therapy or rehabilitation programs may also be recommended to strengthen muscles, improve mobility, and enhance overall function. Additionally, lifestyle modifications, such as avoiding activities that exacerbate symptoms or implementing relaxation techniques, may provide relief.
When it comes to medications, there are several options available. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen can help reduce pain and inflammation. For more severe pain, opioids may be prescribed, but these should be used with caution due to their potential for addiction. Other medications, such as anticonvulsants or antidepressants, may be used to target specific symptoms or provide pain relief.
Physical therapy is a crucial component of non-surgical treatment for sacral nerve damage. A skilled physical therapist can design a personalized exercise program to target the affected muscles and improve range of motion. This may include exercises to strengthen the pelvic floor muscles, improve bladder and bowel control, and enhance overall mobility. In addition to exercises, physical therapists may also use techniques such as electrical stimulation or ultrasound therapy to promote healing and reduce pain.
Rehabilitation programs can also include other non-surgical treatments, such as acupuncture or chiropractic care. These alternative therapies aim to restore balance and promote healing in the body. Acupuncture involves the insertion of thin needles into specific points on the body to stimulate the nervous system and release natural pain-relieving chemicals. Chiropractic care focuses on the alignment of the spine and other joints to improve nerve function and alleviate pain.
Surgical Interventions for Sacral Nerve Damage
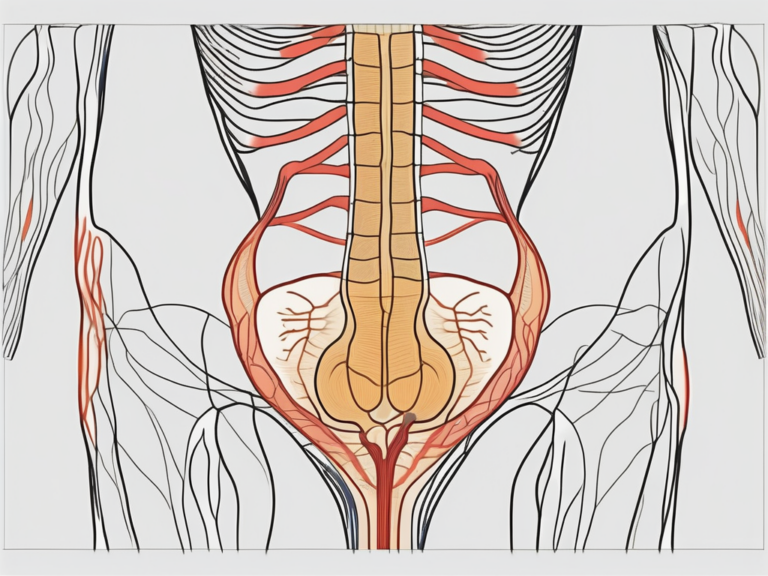
If conservative treatments are ineffective or if the nerve damage is severe, surgical intervention may be necessary. The specific surgical procedure will depend on the underlying cause and the extent of the damage. Surgery may involve decompressing the nerves, removing any structures that are compressing the nerves, or repairing damaged nerve tissue. It is important to note that surgery is typically considered a last resort and is only recommended when conservative measures have been exhausted.
There are several surgical options available for sacral nerve damage. One common procedure is nerve decompression, which involves removing any structures that are compressing the nerves and relieving the pressure. This can be done through minimally invasive techniques or open surgery, depending on the severity of the damage. Another surgical option is nerve grafting, where a healthy nerve is taken from another part of the body and used to repair the damaged nerve. This can help restore function and improve symptoms.
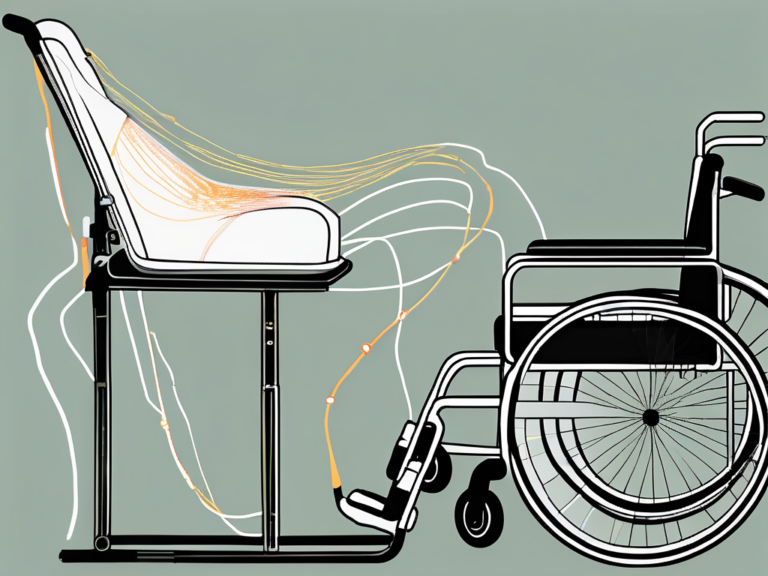
In some cases, sacral nerve stimulation may be recommended. This involves implanting a device that delivers electrical impulses to the sacral nerves, helping to regulate bladder and bowel function. This can be an effective treatment option for individuals who have not responded to other treatments.
Rehabilitation and Physical Therapy
Following surgical intervention or as part of a non-surgical treatment plan, rehabilitation and physical therapy can be valuable in promoting recovery and restoring functionality. These programs focus on strengthening the affected muscles, improving coordination and balance, and addressing any residual pain or mobility issues.
Rehabilitation and physical therapy after surgery typically start with gentle exercises and gradually progress to more challenging activities as the patient’s strength and mobility improve. The goal is to help the patient regain independence and return to their normal daily activities. Physical therapists may use a variety of techniques, such as manual therapy, therapeutic exercises, and modalities like heat or cold therapy, to facilitate healing and improve outcomes.
In addition to physical therapy, occupational therapy may also be beneficial for individuals with sacral nerve damage. Occupational therapists can help patients develop strategies to manage daily activities, such as dressing, bathing, and cooking, despite any limitations caused by the nerve damage. They may recommend assistive devices or modifications to the home environment to enhance safety and independence.
It is important to note that the recovery process for sacral nerve damage can vary greatly from person to person. Some individuals may experience significant improvement with conservative treatments, while others may require more extensive interventions. The key is to work closely with a healthcare team to develop a personalized treatment plan that addresses the specific needs and goals of the individual.
The Importance of Follow-Up Care
After initial treatment for sacral nerve damage, it is crucial to attend regular follow-up appointments with your healthcare provider. This allows them to monitor your progress, assess the effectiveness of the chosen treatment plan, and make any necessary adjustments. Follow-up care also provides an opportunity to address any new symptoms or concerns that may arise.
Regular Check-ups and Monitoring
Regular check-ups are essential to ensure that the sacral nerve damage is properly managed and to identify any potential complications or recurrence of symptoms. During these visits, your doctor may perform neurological examinations, order repeat diagnostic tests if needed, and provide guidance on maintaining optimal nerve health.
Long-Term Management of Sacral Nerve Damage
While some individuals may experience complete recovery, others may require ongoing management of their sacral nerve damage. Long-term management typically involves a combination of lifestyle adjustments, continued physical therapy, and regular monitoring by your healthcare team to prevent complications and promote well-being.
Preventive Measures and Lifestyle Adjustments
While it may not be possible to prevent all cases of sacral nerve damage, there are measures individuals can take to support nerve health and reduce the risk of injury or further damage.
Exercises to Strengthen the Sacral Nerve
Engaging in regular exercises that target the pelvic area, lower back, and surrounding muscles can help strengthen the sacral nerve. Strengthening exercises may include pelvic floor exercises, core-strengthening exercises, and gentle stretching routines. It is important to consult with a healthcare professional or physical therapist to determine the appropriate exercises for your condition.
Dietary Changes to Support Nerve Health
A balanced diet rich in essential nutrients can contribute to overall nerve health. Including foods that are high in omega-3 fatty acids, B vitamins, antioxidants, and minerals can support nerve function. Consult with a registered dietitian or healthcare provider to develop a personalized nutrition plan.
Stress Management and Mental Health Considerations
Chronic stress can have a negative impact on nerve health. Engaging in stress management techniques such as meditation, mindfulness, or seeking support from mental health professionals can help reduce stress levels and promote overall well-being.
While this article provides valuable information on the doctors who treat sacral nerve damage and the available treatment options, it is essential to remember that each case is unique. Consulting with a healthcare professional is crucial in order to receive an accurate diagnosis, personalized treatment plan, and appropriate medical advice.