Where Does the Last Sacral Nerve Exit?
The last sacral nerve, also known as S5, is an essential component of the sacral plexus, a network of nerves located at the base of the spine. Understanding the exit point of this nerve is crucial for medical professionals and patients alike. In this article, we will explore the anatomy of the sacral nerve, the role it plays in our overall health, and the implications of its exit point. Please note that while this article aims to provide helpful information, it is not a substitute for medical advice, and we encourage you to consult with a healthcare professional for personalized guidance.
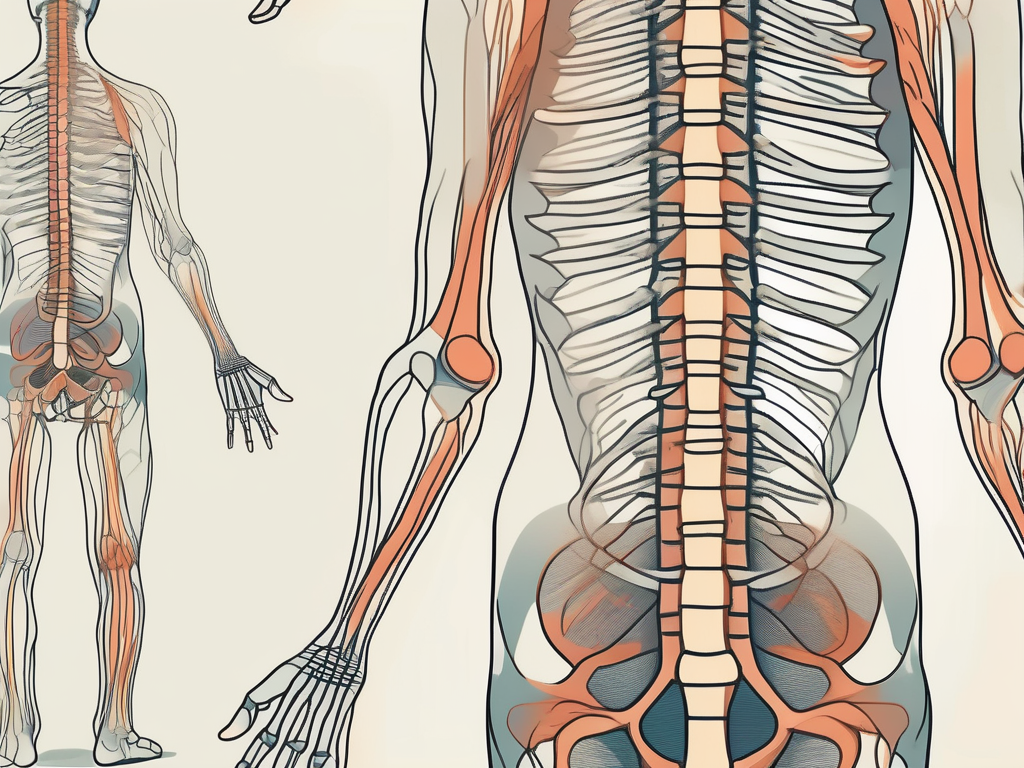
Understanding the Sacral Nerve: An Overview
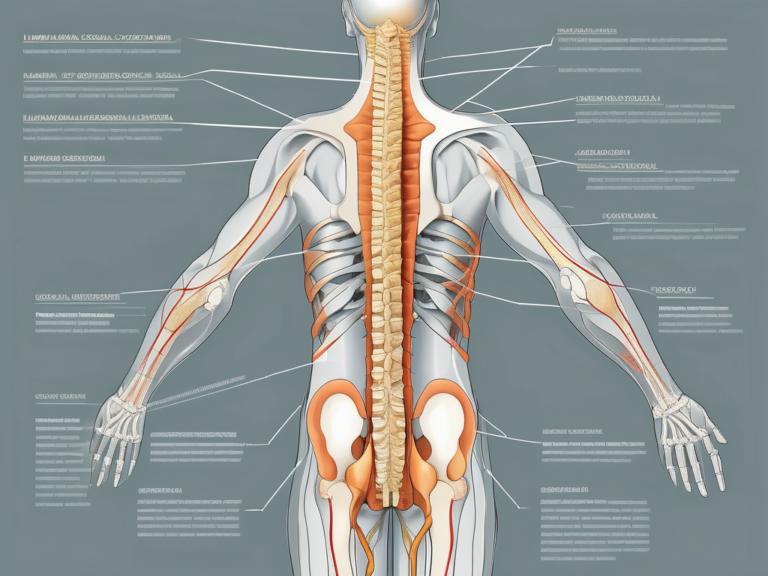
The sacral nerve is one of the five pairs of nerves that emerge from the spinal cord. It originates from the sacral region, specifically from the sacrum – the triangular bone located at the base of the spine. This nerve is responsible for facilitating communication between the central nervous system, which includes the brain and the spinal cord, and various organs and muscles in the pelvic region.
The sacral nerve plays a crucial role in our everyday lives, although it often goes unnoticed. It quietly carries out its duties, ensuring that our bodily functions in the pelvic region are properly regulated. Without the sacral nerve, simple tasks like walking, controlling our bladder, and experiencing sexual pleasure would be challenging, if not impossible.
Anatomy of the Sacral Nerve
The sacral nerve is composed of multiple smaller nerves that emerge from the sacral plexus. These nerves work collectively to transmit sensory information, such as touch and pain, from the pelvic region to the brain, and motor signals from the brain to the muscles in the pelvis and lower limbs.
Imagine a complex network of nerves, intricately woven together like a tapestry, forming the sacral plexus. Within this network, the sacral nerve courses through the pelvis along with other nerves, such as the sciatic nerve, which is the longest nerve in the body. Together, these nerves create a symphony of communication, allowing us to perform essential functions with ease.
Like a conductor leading an orchestra, the sacral nerve coordinates the movements of various muscles in the pelvic region. It ensures that the muscles involved in bladder and bowel control work harmoniously, preventing embarrassing accidents and maintaining our dignity. Furthermore, the sacral nerve innervates the muscles of the lower limbs, enabling us to walk, run, and engage in physical activities that bring us joy.
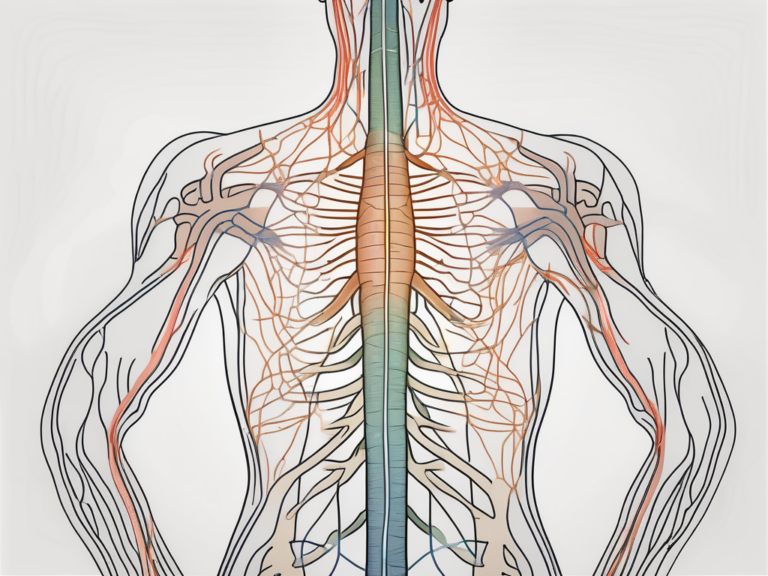
Function of the Sacral Nerve
As mentioned earlier, the sacral nerve is responsible for maintaining proper functioning of the pelvic region. It controls the muscles involved in bladder and bowel control, contributes to sexual function, and innervates the muscles of the lower limbs, allowing for voluntary movement.
But the sacral nerve’s role doesn’t end there. It also carries sensory information from the pelvic region back to the brain, providing us with a rich tapestry of sensations. Through the sacral nerve, we can perceive the gentle touch of a loved one, the warmth of a cozy embrace, and the pleasure that comes from intimate moments.
Moreover, the sacral nerve acts as a messenger, relaying important signals from the brain to the pelvic organs. It ensures that our reproductive system functions properly, allowing us to experience the joys of parenthood if we so desire. Additionally, the sacral nerve plays a vital role in sexual function, allowing us to experience pleasure and intimacy in our relationships.
So, the next time you walk effortlessly, control your bladder without a second thought, or experience the pleasure of touch, remember to thank the sacral nerve. This unsung hero quietly works behind the scenes, ensuring that our lives are filled with comfort, joy, and the ability to engage in the activities we love.
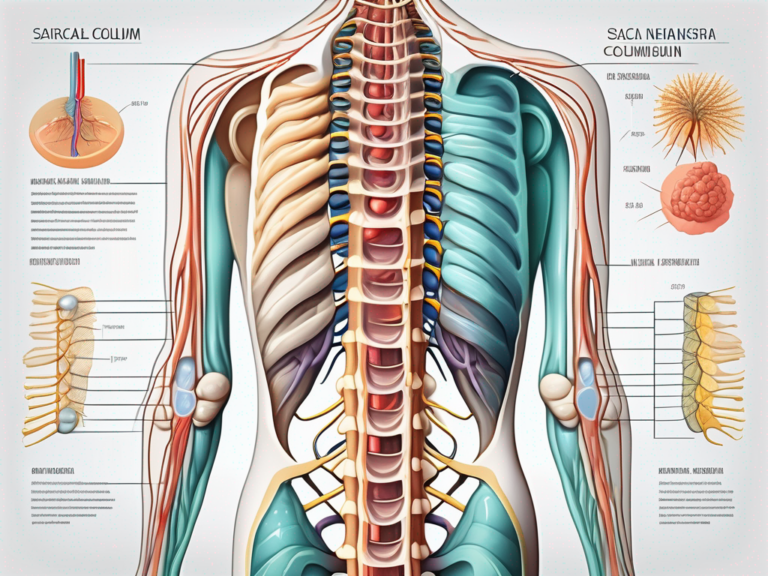
The Sacral Plexus: A Closer Look
The sacral plexus is a complex network of nerves formed by the merging of several nerve roots that exit the sacrum. These nerve roots, known as the anterior and posterior divisions, give rise to various branches that ultimately form the sacral nerve.
The sacral plexus is a fascinating structure that plays a crucial role in the functioning of the pelvic region. Let’s delve deeper into its components and understand how it contributes to our overall well-being.
Components of the Sacral Plexus
The sacral plexus consists of multiple nerves, each with its own unique functions and responsibilities. These nerves work in harmony to ensure the optimal functioning of the pelvic region.
One of the major nerves within the sacral plexus is the sciatic nerve. This nerve is the longest and thickest nerve in the human body and is responsible for innervating the muscles of the lower limbs. It plays a crucial role in our ability to move and feel sensations in this area.
Another important nerve within the sacral plexus is the pudendal nerve. This nerve provides sensation to the external genitalia and controls the muscles involved in bowel and bladder function. Without the pudendal nerve, our ability to control these essential bodily functions would be compromised.
In addition to the sciatic and pudendal nerves, the sacral plexus also includes the superior gluteal nerve and the inferior gluteal nerve. These nerves innervate the muscles of the buttocks, allowing us to perform movements such as walking, running, and sitting.
Lastly, the sacral plexus is completed by the last sacral nerve, also known as S5. This nerve is responsible for transmitting both sensory and motor signals from the pelvic region. It plays a vital role in our overall functionality and well-being.
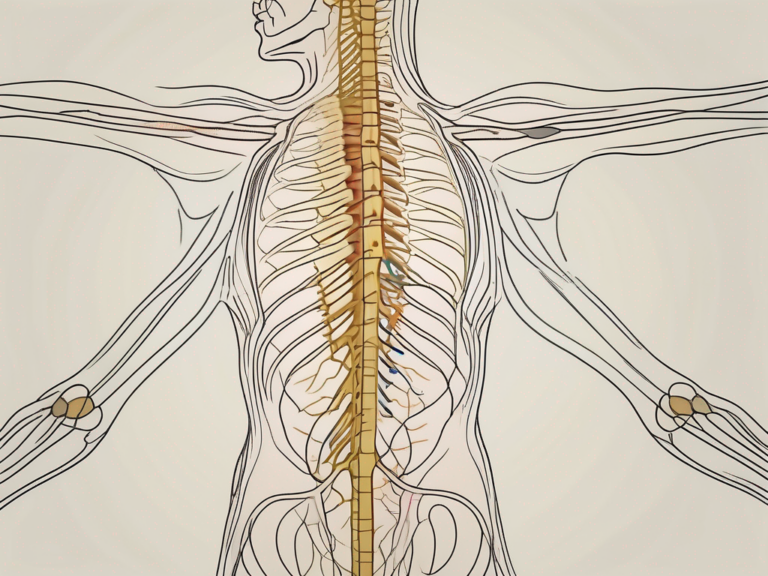
Role of the Sacral Plexus in Nerve Exit
The sacral plexus consists of both sensory and motor fibers, which are essential for the transmission of signals between the pelvic region and the brain.
Once the nerve fibers reach the exit point in the sacrum, the sacral plexus branches out to form the individual nerves, including the last sacral nerve. This branching allows for a more efficient distribution of signals, ensuring that the pelvic region receives the necessary sensory information and motor commands.
Through the last sacral nerve, the sacral plexus enables the transmission of sensory information from the pelvic region to the brain. This includes sensations such as touch, temperature, and pain. Additionally, the motor fibers of the sacral plexus transmit signals from the brain to the pelvic muscles, allowing for voluntary control and coordination of movements in this area.
Overall, the sacral plexus and its intricate network of nerves are essential for the proper functioning of the pelvic region. Without this complex system, we would experience difficulties in controlling our bowel and bladder functions, as well as in performing movements of the lower limbs and buttocks.
Understanding the sacral plexus and its components gives us a deeper appreciation for the complexity and interconnectedness of the human body. It serves as a reminder of the remarkable design and functionality of our nervous system.
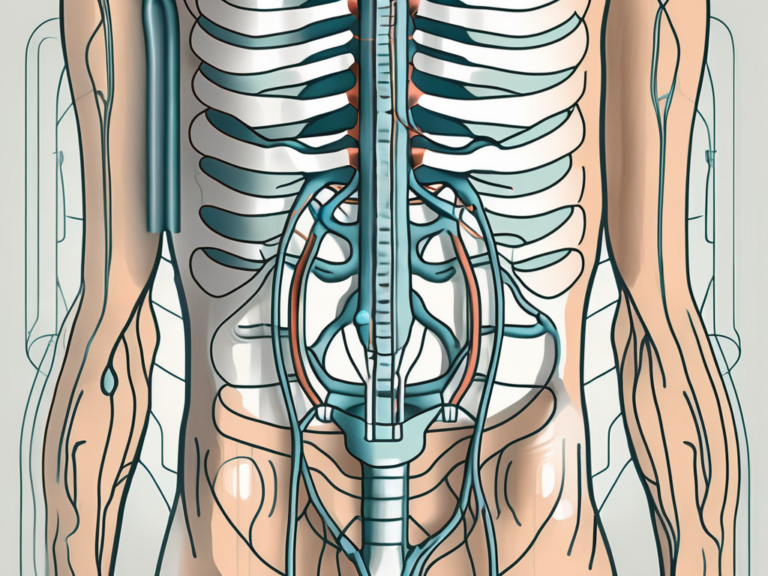
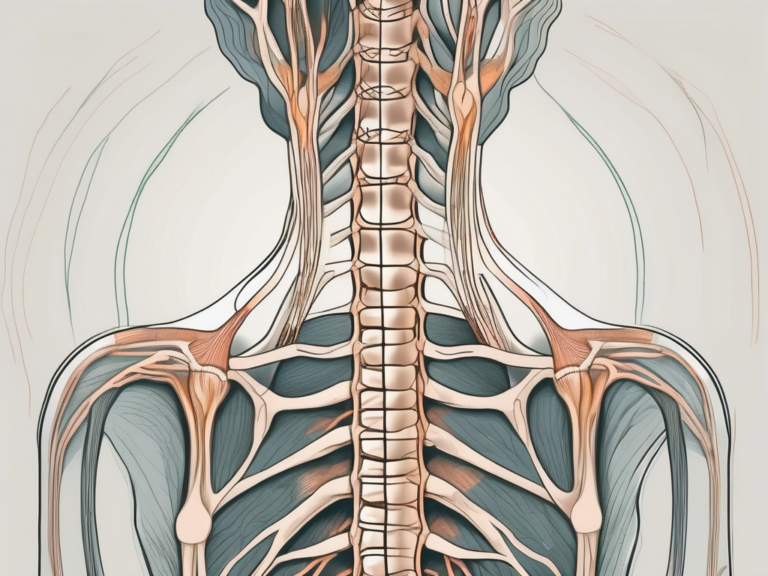
The Exit Point of the Last Sacral Nerve
The exit point of the last sacral nerve is an anatomical feature that medical professionals consider when diagnosing and treating certain conditions related to the pelvic region. Locating the exit point accurately is crucial for determining the cause of symptoms and implementing appropriate treatment strategies.
Identifying the Exit Point
The last sacral nerve typically exits the sacrum through the sacral foramen, which are small openings in the bone. It emerges alongside other nerves from the sacral plexus and continues to course its way to the target muscles and organs in the pelvic region.
Medical professionals employ various techniques to identify the exit point of the last sacral nerve. One such technique is the use of medical imaging, such as magnetic resonance imaging (MRI) and computed tomography (CT) scans. These imaging techniques provide detailed images of the sacrum and the associated nerves, aiding in the identification of the exit point.
However, it is important to note that while medical imaging can provide valuable information, it is the expertise of medical professionals that allows for accurate identification of the exit point of the last sacral nerve. Through years of training and experience, healthcare providers develop the skills necessary to interpret the imaging results and pinpoint the precise location of the nerve’s exit point.
Significance of the Exit Point
The exit point of the last sacral nerve holds significance in various medical conditions. For instance, in cases of sacral nerve root compression or injury, the precise location of the exit point helps healthcare providers determine the specific nerve roots involved, facilitating appropriate treatment decisions.
Understanding the exit point is also vital for procedures such as epidural injections. These injections aim to provide pain relief by targeting specific nerve roots. By knowing the exit point of the last sacral nerve, medical professionals can accurately guide the needle to the desired location, ensuring the medication is delivered precisely and maximizing its therapeutic effect.
Furthermore, the exit point of the last sacral nerve plays a role in the diagnosis and treatment of conditions affecting the pelvic region. Conditions such as sciatica, pelvic pain, and urinary incontinence can be influenced by the functioning of the sacral nerves. Identifying the exit point allows medical professionals to assess the health and integrity of the nerve, aiding in the development of appropriate treatment plans.
In conclusion, the exit point of the last sacral nerve is a crucial anatomical feature that medical professionals consider when diagnosing and treating conditions related to the pelvic region. Accurate identification of the exit point enables healthcare providers to determine the cause of symptoms and implement appropriate treatment strategies, leading to improved patient outcomes.
Implications of Sacral Nerve Exit on Health
The exit point of the last sacral nerve plays a pivotal role in maintaining optimal health and function of the pelvic region. Let’s explore some of the implications and conditions related to its exit point.
The sacral nerve, also known as the S5 nerve, emerges from the sacral spinal cord and exits the spinal column through the sacral foramen. This exit point is crucial for the transmission of nerve signals to and from the pelvic region. It serves as a communication pathway between the brain and the various organs and structures in the pelvis, including the bladder, rectum, and reproductive organs.
Disorders Related to Sacral Nerve Exit
Disorders affecting the sacral nerve and its exit point can result in various symptoms and functional impairments. Common conditions include sciatica, which causes pain, tingling, and weakness in the lower back, buttock, and leg; cauda equina syndrome, a rare but serious condition that requires immediate medical attention; and pudendal neuralgia, characterized by chronic pelvic pain and discomfort.
Sciatica occurs when the sciatic nerve, which originates from the sacral nerve roots, becomes compressed or irritated. This can happen due to a herniated disc, spinal stenosis, or other spinal abnormalities. The resulting symptoms can range from mild discomfort to debilitating pain that radiates down the leg.
Cauda equina syndrome is a medical emergency that occurs when the nerve roots at the lower end of the spinal cord become compressed. This compression can lead to severe back pain, numbness or weakness in the legs, loss of bladder or bowel control, and even paralysis if left untreated. Immediate medical intervention is necessary to prevent permanent damage.
Pudendal neuralgia is a condition that affects the pudendal nerve, which originates from the sacral nerve roots and supplies sensation to the genital area. It can cause chronic pelvic pain, discomfort during sexual intercourse, and urinary or bowel dysfunction. The exact cause of pudendal neuralgia is often unknown, but it can be associated with trauma, nerve entrapment, or inflammation.
If you experience any symptoms related to these conditions, we strongly recommend consulting with a healthcare professional for a thorough evaluation and appropriate management. They can provide a proper diagnosis, recommend treatment options, and offer guidance tailored to your specific situation.
Treatment Options for Sacral Nerve Disorders
Once a diagnosis has been made, treatment options for sacral nerve disorders may include a variety of approaches. These can range from conservative measures, such as pain medications, physical therapy, and lifestyle modifications, to more invasive interventions like nerve blocks or surgical procedures.
Conservative treatments aim to alleviate symptoms and improve function without the need for invasive procedures. Physical therapy can help strengthen the muscles surrounding the sacral nerve exit point, improve flexibility, and reduce pain. Pain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or muscle relaxants, may be prescribed to manage pain and inflammation. Lifestyle modifications, such as avoiding activities that exacerbate symptoms or using ergonomic supports, can also be beneficial.
In cases where conservative treatments are ineffective or the condition is severe, more invasive interventions may be considered. Nerve blocks, which involve injecting medication near the affected nerve to block pain signals, can provide temporary relief. Surgical procedures, such as decompression or nerve release surgeries, may be necessary to alleviate compression or remove any entrapment causing the symptoms.
It is essential to discuss the potential risks, benefits, and expected outcomes of each treatment option with your healthcare provider. They will review your medical history, conduct a thorough examination, and take into consideration your individual circumstances when formulating a treatment plan that suits your needs.
Future Research Directions in Sacral Nerve Study
The study of the sacral nerve and its exit point continues to evolve, with ongoing research aimed at expanding our understanding and improving patient outcomes. Let’s take a brief look at two potential areas of future research.
Unanswered Questions in Sacral Nerve Anatomy
Though we have made significant strides in elucidating the anatomy and function of the sacral nerve, there are still unanswered questions that warrant further investigation. For instance, researchers are exploring the precise mechanisms of nerve regeneration after injury, as well as the neural pathways responsible for pain perception in the pelvic region.
Understanding the mechanisms of nerve regeneration is crucial for developing effective treatment strategies for patients with sacral nerve injuries. By unraveling the intricate processes involved in nerve regrowth, researchers can potentially identify therapeutic targets to enhance and accelerate the healing process. This knowledge can pave the way for innovative interventions, such as regenerative medicine techniques or nerve grafting procedures, to restore function and improve the quality of life for patients.
Furthermore, investigating the neural pathways responsible for pain perception in the pelvic region can provide valuable insights into the management of chronic pain conditions. By deciphering the complex network of nerves involved in transmitting pain signals, researchers can develop targeted therapies to alleviate pain and improve the overall well-being of patients suffering from sacral nerve-related disorders.
Potential Innovations in Sacral Nerve Treatment
Advancements in technology and medical research are continuously reshaping the landscape of healthcare. In the realm of sacral nerve treatment, potential innovations may include the development of more precise and minimally invasive surgical techniques, improved imaging modalities for enhanced visualization of nerve structures, and the advent of targeted drug therapies.
Minimally invasive surgical techniques hold great promise for sacral nerve treatment. These procedures, such as laparoscopic or robotic-assisted surgeries, offer several advantages over traditional open surgeries, including smaller incisions, reduced postoperative pain, shorter hospital stays, and faster recovery times. By refining and expanding the application of these techniques, surgeons can minimize surgical trauma and optimize patient outcomes.
Moreover, advancements in imaging modalities can provide clinicians with detailed and accurate visualizations of the sacral nerve and surrounding structures. Techniques such as magnetic resonance imaging (MRI) and computed tomography (CT) scans can help identify anatomical variations, detect nerve compression or damage, and guide surgical interventions with precision. The integration of advanced imaging technologies into routine clinical practice can significantly improve diagnostic accuracy and aid in treatment planning.
Additionally, the development of targeted drug therapies specifically designed to modulate sacral nerve function shows promise in the field of sacral nerve treatment. These therapies can potentially address various sacral nerve-related conditions, such as urinary incontinence or sexual dysfunction, by selectively targeting the underlying neural pathways involved. By tailoring medications to act on specific receptors or signaling molecules, researchers aim to achieve more effective and personalized treatment approaches.
In conclusion, the future of sacral nerve study holds exciting possibilities for advancing our knowledge and improving patient care. Further research into unanswered questions in sacral nerve anatomy and the exploration of potential innovations in treatment modalities can lead to groundbreaking discoveries and transformative interventions. By continuously pushing the boundaries of scientific understanding, we can strive towards better outcomes and enhanced quality of life for individuals affected by sacral nerve-related conditions.
Conclusion
In conclusion, understanding the exit point of the last sacral nerve is crucial for healthcare professionals and individuals seeking to comprehend the implications of sacral nerve activity on overall health. The anatomy and functionality of the sacral nerve and its exit point play a vital role in various pelvic functions, and disorders related to this area can have a significant impact on one’s quality of life.
If you suspect any issues with your sacral nerve or experience related symptoms, we strongly advise consulting with a healthcare professional who can provide expert evaluation and guidance. They can help determine the underlying cause of your symptoms and recommend appropriate treatment options tailored to your needs. Remember, a thorough assessment from a medical professional is essential in optimizing your health and well-being.