How to Stimulate the Sacral Nerve: A Comprehensive Guide
The sacral nerve plays a crucial role in our overall well-being. Understanding how to stimulate this nerve can have profound effects on our health and quality of life. In this comprehensive guide, we will delve into the anatomy and function of the sacral nerve, explore the importance of sacral nerve stimulation, discuss the preparations required, examine various techniques for stimulation, and provide essential post-stimulation care and maintenance tips. Finally, we will address some frequently asked questions about sacral nerve stimulation.
Understanding the Sacral Nerve
The sacral nerve is a key component of our nervous system, originating from the lower end of the spinal cord. It is responsible for transmitting signals to and from the organs and muscles within the pelvic region. Proper functioning of the sacral nerve is essential for bladder and bowel control, sexual function, and overall pelvic stability.
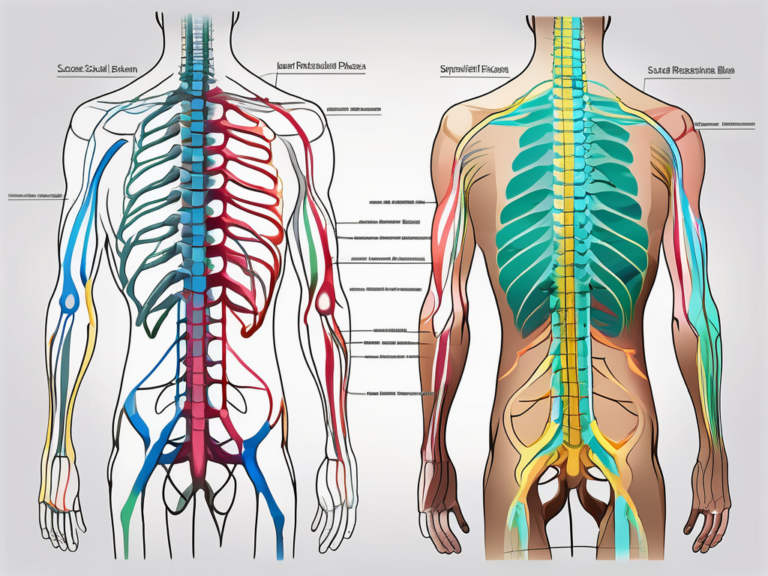
Anatomy of the Sacral Nerve
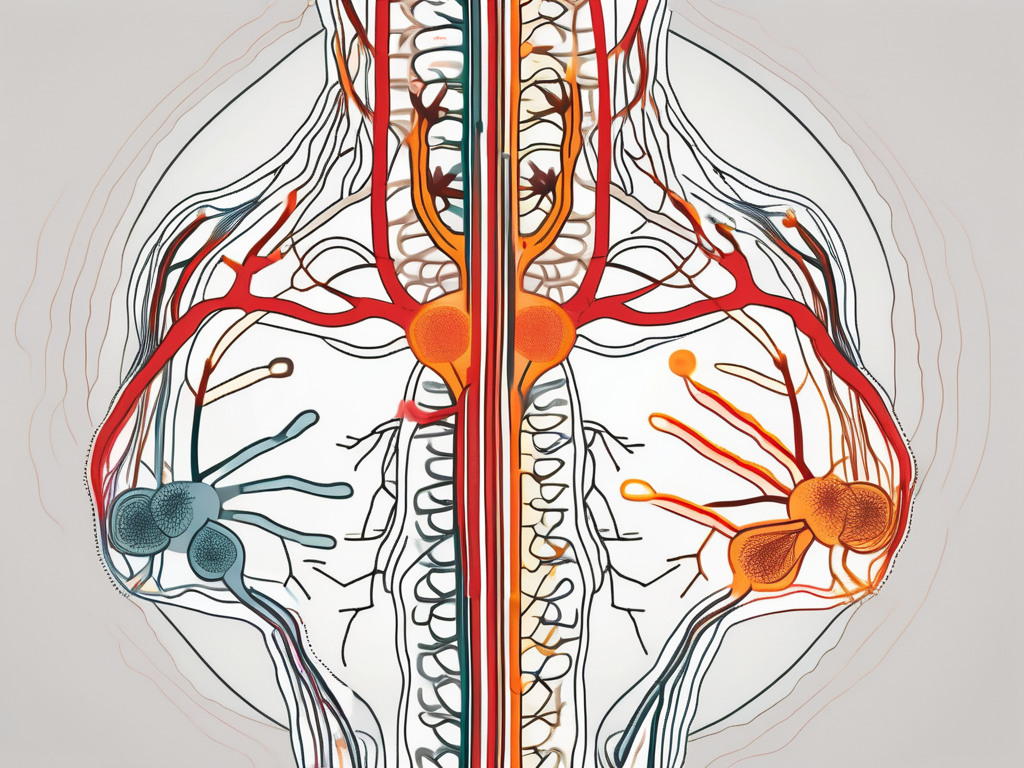
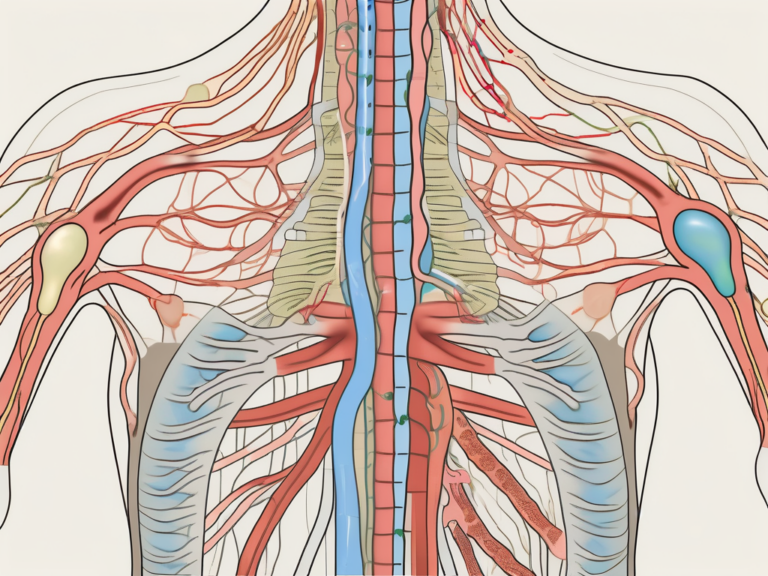
The sacral nerve consists of a network of nerves that branch out from the spinal cord, specifically from the sacral region. These nerves innervate various pelvic organs, including the bladder, rectum, and reproductive organs. They also connect to the muscles of the pelvic floor, contributing to their proper coordination and control.
Within the sacral nerve network, there are different types of nerve fibers that serve distinct functions. Some nerve fibers are responsible for transmitting sensory information, while others are involved in motor control. This intricate network ensures the efficient communication between the brain and the pelvic region.
As the sacral nerve branches out from the spinal cord, it forms a complex web of interconnected nerves. These nerves extend to different parts of the pelvic region, reaching every nook and cranny of the organs and muscles within. This extensive network allows for precise and coordinated control of the pelvic functions.
Function of the Sacral Nerve
The sacral nerve carries both sensory and motor signals. Sensory signals transmit information about bladder and bowel fullness, pain, and sexual arousal. These signals are crucial for maintaining awareness of bodily functions and responding appropriately to stimuli.
Motor signals, on the other hand, stimulate the contraction and relaxation of the pelvic muscles, facilitating bowel movements, urination, and sexual activity. The sacral nerve plays a vital role in coordinating the intricate dance of muscles involved in these activities, ensuring their smooth and efficient execution.
Additionally, the sacral nerve is involved in maintaining pelvic stability. It provides the necessary support and control for the pelvic floor muscles, which are responsible for maintaining the position of the pelvic organs and preventing prolapse.
Furthermore, the sacral nerve contributes to the regulation of blood flow in the pelvic region. It helps to control the dilation and constriction of blood vessels, ensuring adequate blood supply to the pelvic organs and tissues.
In summary, the sacral nerve is a complex and essential component of our nervous system. Its intricate anatomy and multifaceted functions enable proper bladder and bowel control, sexual function, and overall pelvic stability. Understanding the role of the sacral nerve helps us appreciate the remarkable coordination and control required for these fundamental bodily functions.
Importance of Sacral Nerve Stimulation
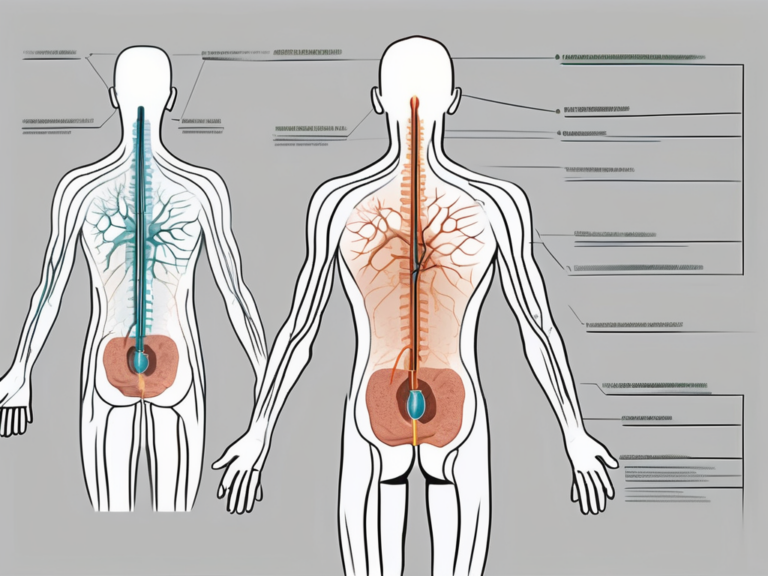
Sacral nerve stimulation is a revolutionary medical technique that offers numerous health benefits for individuals with conditions affecting the pelvic region. By stimulating the sacral nerve, we can effectively manage or alleviate symptoms such as urinary incontinence, fecal incontinence, urinary retention, chronic pelvic pain, and sexual dysfunction.
The sacral nerve, also known as the S3 nerve, plays a crucial role in controlling the muscles and organs in the pelvic area. When this nerve is not functioning optimally, it can lead to a variety of distressing symptoms that significantly impact a person’s quality of life. Sacral nerve stimulation works by delivering electrical impulses to the sacral nerve, helping to restore normal function and alleviate these symptoms.
Health Benefits of Sacral Nerve Stimulation
The health benefits of sacral nerve stimulation are vast and can have a profound impact on a person’s well-being. One of the primary benefits is the improvement in bladder and bowel control. Many individuals with conditions such as overactive bladder or fecal incontinence experience frequent episodes of leakage, which can be embarrassing and disruptive. Sacral nerve stimulation has been shown to significantly reduce these episodes, allowing individuals to regain control over their bodily functions.
In addition to improving bladder and bowel control, sacral nerve stimulation can also help in relieving chronic pelvic pain. Chronic pelvic pain is a complex condition that can have various underlying causes, such as endometriosis, interstitial cystitis, or pelvic floor dysfunction. By stimulating the sacral nerve, this technique can help alleviate the pain and discomfort associated with these conditions, providing much-needed relief to individuals who have been suffering for extended periods.
Furthermore, sacral nerve stimulation has been found to have a positive impact on sexual function. Many individuals with pelvic conditions experience sexual dysfunction, which can strain relationships and negatively affect overall well-being. By improving pelvic muscle function and reducing pain, sacral nerve stimulation can enhance sexual pleasure and intimacy, allowing individuals to regain a fulfilling and satisfying sex life.
Overall, sacral nerve stimulation has the potential to enhance the overall quality of life for individuals with conditions affecting the pelvic region. It can provide relief from distressing symptoms, improve bodily functions, and restore a sense of control and normalcy.
However, it is crucial to consult with a medical professional to determine if sacral nerve stimulation is the right course of treatment for your specific condition. Each individual is unique, and a thorough evaluation by a healthcare provider is necessary to ensure that this technique is appropriate and safe.
Potential Risks and Complications
While sacral nerve stimulation can be highly successful in improving symptoms and enhancing quality of life, it is essential to acknowledge that any medical procedure carries some risks. It is crucial to have a comprehensive understanding of the potential risks and complications associated with sacral nerve stimulation before making a decision.
One common risk associated with sacral nerve stimulation is infection. As with any surgical procedure, there is a risk of infection at the implant site. However, healthcare providers take extensive precautions to minimize this risk, such as using sterile techniques and prescribing antibiotics when necessary.
Pain at the implant site is another potential complication. Some individuals may experience discomfort or tenderness at the site where the device is implanted. However, this discomfort is usually temporary and can be managed with pain medication or other interventions as needed.
Device malfunction is another risk to consider. While rare, there is a possibility that the sacral nerve stimulation device may malfunction or fail to work as intended. Regular follow-up appointments with a healthcare provider can help monitor the device’s function and address any issues that may arise.
Lead migration or damage is also a potential complication. The leads, which are the wires that deliver the electrical impulses to the sacral nerve, may shift or become damaged over time. This can lead to a loss of effectiveness or discomfort. Regular monitoring and adjustments by a healthcare provider can help ensure that the leads are properly positioned and functioning optimally.
It is crucial to discuss these potential risks and complications with your doctor before proceeding with the sacral nerve stimulation procedure. Your healthcare provider will be able to provide you with detailed information specific to your situation and help you make an informed decision about your treatment options.
Preparing for Sacral Nerve Stimulation
Before undergoing sacral nerve stimulation, it is crucial to consult with a healthcare professional who specializes in this field. They will perform a thorough medical evaluation and diagnosis to determine if sacral nerve stimulation is an appropriate treatment option for your condition.
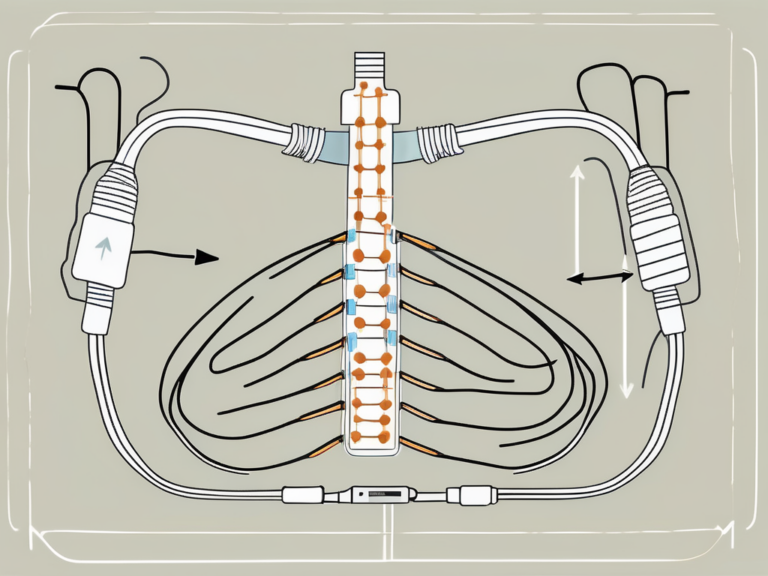
Sacral nerve stimulation is a procedure that involves the implantation of a small device, similar to a pacemaker, to deliver electrical impulses to the sacral nerves. These nerves play a crucial role in controlling the bladder, bowel, and pelvic floor muscles. By stimulating these nerves, sacral nerve stimulation can help manage conditions such as overactive bladder, urinary retention, and fecal incontinence.
Medical Consultation and Diagnosis
Your doctor will review your medical history, conduct a physical examination, and may order additional tests or imaging studies to assess the extent of your sacral nerve dysfunction. This comprehensive evaluation will help determine if sacral nerve stimulation is the right treatment option for you.
During the consultation, it is important to provide your doctor with detailed information about your symptoms, including the frequency and severity of your bladder or bowel dysfunction. This will help them understand the impact of your condition on your daily life and tailor the treatment accordingly.
Your doctor may also ask about any previous treatments you have tried, such as medications or behavioral therapies. This information will help them assess the effectiveness of these treatments and determine if sacral nerve stimulation is a suitable next step.
Furthermore, your doctor will discuss the potential benefits and risks of sacral nerve stimulation with you. They will explain the procedure in detail, including the surgical implantation of the device and the potential side effects or complications that may arise. It is important to ask any questions or express any concerns you may have during this consultation.
Pre-Stimulation Preparations
Prior to the procedure, your doctor may advise you to make certain lifestyle changes or adjustments. These recommendations are aimed at optimizing the success of sacral nerve stimulation and improving your overall health.
One common recommendation is to manage your weight. Excess weight can put additional pressure on the pelvic floor muscles and worsen symptoms of bladder or bowel dysfunction. Your doctor may provide guidance on healthy eating habits and exercise routines to help you achieve and maintain a healthy weight.
In addition, quitting smoking is often advised before undergoing sacral nerve stimulation. Smoking can impair blood flow and delay the healing process, which may affect the success of the procedure. Your doctor can provide resources and support to help you quit smoking if needed.
Maintaining a healthy diet and exercise regimen is also important. A balanced diet rich in fruits, vegetables, and whole grains can support overall health and improve bladder and bowel function. Regular exercise, such as pelvic floor exercises and aerobic activities, can strengthen the pelvic floor muscles and enhance the effectiveness of sacral nerve stimulation.
It is crucial to follow your doctor’s recommendations and prepare yourself physically and mentally for the sacral nerve stimulation procedure. By taking these steps, you can increase the likelihood of a successful outcome and improve your quality of life.
Techniques for Sacral Nerve Stimulation
When it comes to sacral nerve stimulation, there are a variety of techniques available to address different conditions and individual needs. These techniques range from non-invasive methods that can be performed at home to more invasive procedures that require the expertise of a healthcare professional.
Non-Invasive Methods
One of the non-invasive techniques for sacral nerve stimulation is transcutaneous electrical nerve stimulation (TENS). This method involves the application of mild electrical currents to the sacral nerve area through adhesive electrodes placed on the skin. TENS can be a convenient option as it can be performed at home under the guidance of a healthcare professional. It may provide temporary relief for certain conditions such as pelvic pain or overactive bladder.
Another non-invasive method is percutaneous tibial nerve stimulation (PTNS). This technique involves the insertion of a thin needle near the ankle to stimulate the tibial nerve, which is connected to the sacral nerve. The stimulation is done using a small device that delivers electrical impulses. PTNS is often used for individuals with overactive bladder or urinary incontinence and can be performed in an outpatient setting.
In addition to TENS and PTNS, there are other non-invasive approaches that can be explored. These include acupuncture, which involves the insertion of thin needles into specific points on the body to stimulate nerve activity, and biofeedback, which uses sensors to monitor and provide feedback on muscle activity in the pelvic region.
Invasive Methods
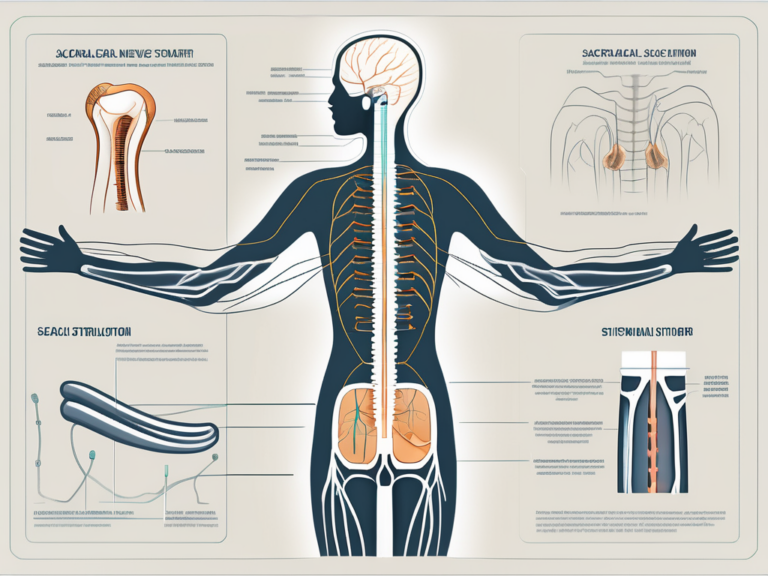
Invasive methods for sacral nerve stimulation are typically considered when non-invasive techniques have not provided sufficient relief or for individuals with more severe or chronic conditions. One of the commonly used invasive methods is sacral nerve neuromodulation, also known as sacral nerve stimulation (SNS).
SNS involves the implantation of a small device, similar to a pacemaker, under the skin near the sacral nerve region. This device delivers electrical impulses to the sacral nerve, modulating its activity and helping to alleviate symptoms. The procedure to implant the device is performed by a qualified healthcare professional and requires careful monitoring and follow-up care.
Another invasive method is dorsal root ganglion (DRG) stimulation. DRG stimulation involves the placement of electrodes near the dorsal root ganglion, which is a cluster of nerve cells located along the spinal cord. By targeting the specific area where the pain signals are transmitted, DRG stimulation can provide more targeted pain relief for conditions such as chronic pelvic pain or complex regional pain syndrome.
It is important to note that invasive methods for sacral nerve stimulation are typically considered after a thorough evaluation of the individual’s condition and a trial period of non-invasive techniques. The decision to undergo an invasive procedure should be made in consultation with a healthcare provider who can assess the potential benefits and risks.
In conclusion, sacral nerve stimulation offers a range of techniques that can be tailored to individual needs. Whether through non-invasive methods like TENS or more invasive procedures like SNS or DRG stimulation, these techniques aim to provide relief and improve the quality of life for individuals with conditions affecting the sacral nerve region.
Post-Stimulation Care and Maintenance
After undergoing sacral nerve stimulation, proper post-stimulation care and maintenance are vital for optimal outcomes and long-term success.
Recovery and Rehabilitation
Following the procedure, you will likely experience some discomfort and swelling at the implant site. Your doctor will provide specific post-operative instructions, such as wound care and activity restrictions, to support your recovery. It is essential to adhere to these guidelines and to attend follow-up appointments to monitor your progress closely.
Long-Term Care and Follow-Up
Regular follow-up appointments with your healthcare provider are crucial to evaluate the effectiveness of sacral nerve stimulation and to assess any potential complications. They will help adjust the stimulation settings and provide guidance on maintaining the implanted device properly. If you experience any issues or changes in your symptoms, it is essential to contact your doctor immediately for further evaluation.
Frequently Asked Questions about Sacral Nerve Stimulation
Is Sacral Nerve Stimulation Painful?
Sacral nerve stimulation itself should not be painful. However, some individuals may experience a mild tingling sensation, warmth, or a sensation of pressure around the stimulation site during the procedure or when the device is activated. It is essential to communicate any discomfort or concerns to your healthcare provider.
How Often Should the Sacral Nerve be Stimulated?
The frequency and duration of sacral nerve stimulation vary depending on your specific condition and treatment plan. Your healthcare provider will determine the optimal parameters for your device and provide instructions on how to adjust them if needed. It is crucial to follow their guidance and report any changes in your symptoms during the follow-up appointments.
In conclusion, sacral nerve stimulation is a valuable treatment option for individuals with pelvic dysfunctions. By understanding the anatomy, function, and importance of the sacral nerve, and by following the appropriate preparations, techniques, and post-stimulation care, individuals can potentially experience significant improvements in their quality of life. It is essential, however, to consult with a healthcare professional to determine if sacral nerve stimulation is the right approach for your specific condition. With the guidance of medical experts, you can make informed decisions and embark on a journey towards a better, more comfortable life.