How to Stimulate the Sacral Nerve: A Comprehensive Guide
The sacral nerve is an essential part of the nervous system, playing a crucial role in various bodily functions. Stimulating the sacral nerve can have a range of benefits, but it is important to understand its anatomy and function before exploring the techniques. In this comprehensive guide, we will delve into the intricacies of sacral nerve stimulation, its importance, preparation, techniques, post-stimulation care, and address frequently asked questions, ensuring you have a thorough understanding of this topic.
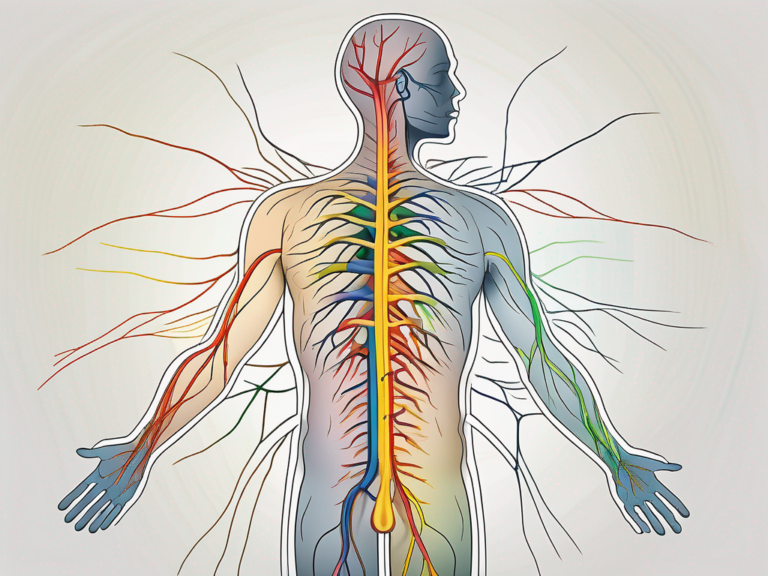
Understanding the Sacral Nerve
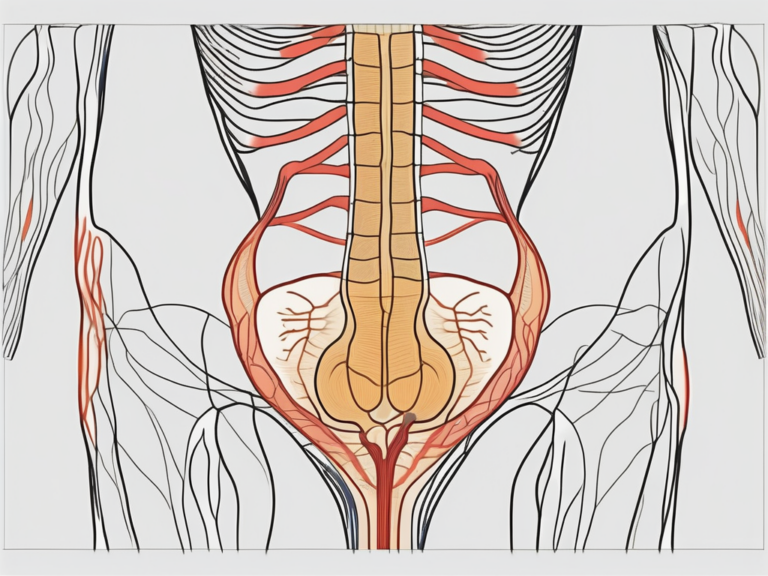
The sacral nerve is located in the lower back and consists of nerve fibers that originate from the sacral plexus. It plays a vital role in controlling the functioning of the pelvic organs, including the bladder, rectum, and sexual organs. Understanding the anatomy and function of the sacral nerve is crucial in comprehending the significance of stimulating it.
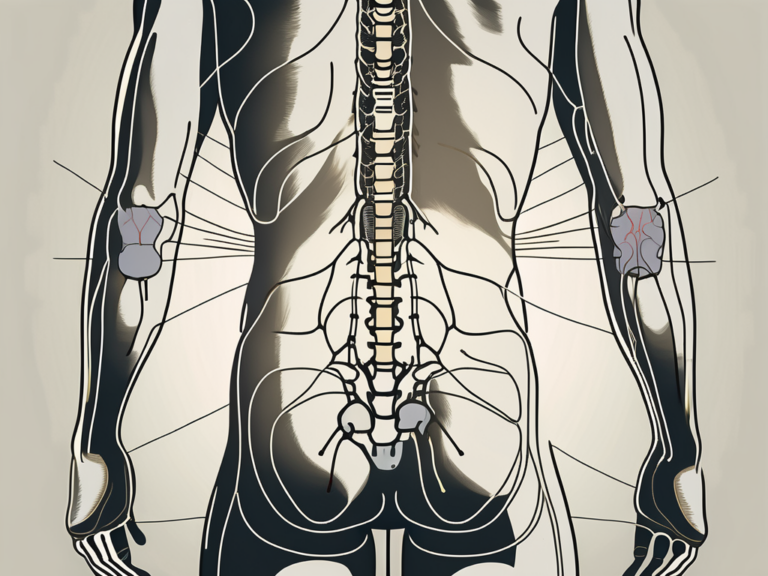
Anatomy of the Sacral Nerve
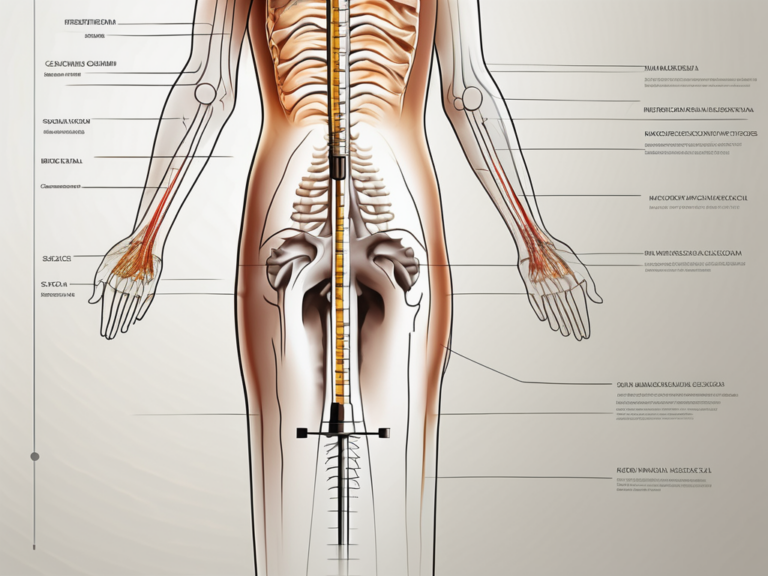
The sacral nerve consists of several nerve roots that arise from the spinal cord’s lower region. These roots then merge to form the sacral plexus, a complex network of nerves. From the sacral plexus, various nerves extend to the pelvic area and control specific functions.
Within the sacral plexus, there are five pairs of sacral nerves, known as S1 to S5. Each pair of nerves branches out to different parts of the pelvic region, ensuring the proper functioning of various organs. The S1 nerve, for example, innervates the gluteal muscles, while the S2 nerve supplies the muscles of the posterior thigh and lower leg.
As the sacral nerves extend further into the pelvis, they give rise to the pelvic splanchnic nerves. These nerves are responsible for controlling the smooth muscles of the pelvic organs, including the bladder, rectum, and reproductive organs. The intricate network of nerves within the sacral plexus ensures precise communication between the brain and the pelvic organs.
Function of the Sacral Nerve
The sacral nerve plays a pivotal role in regulating urinary and bowel functions, as well as sexual function. It helps control the muscles responsible for bladder contraction and relaxation, fecal continence, and sexual arousal. Dysfunction of the sacral nerve can lead to a variety of issues, such as urinary incontinence, fecal incontinence, and sexual dysfunction.
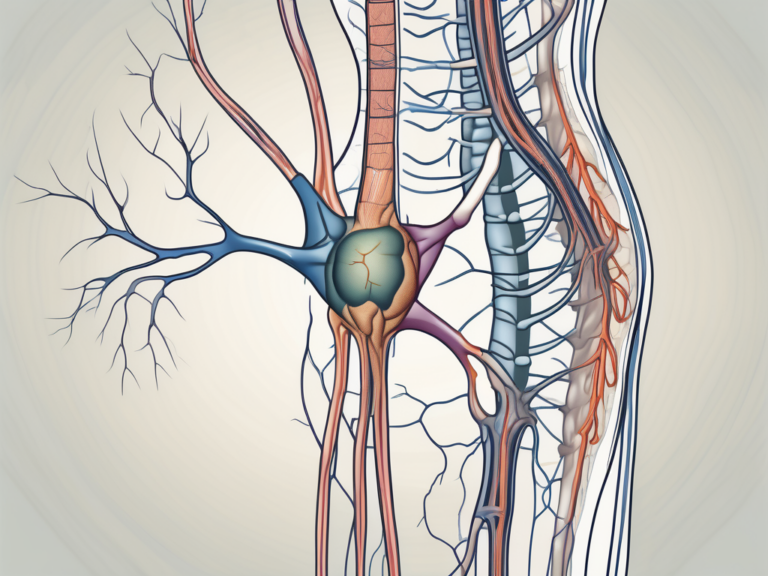
When the sacral nerve is stimulated, it can have therapeutic effects on various pelvic disorders. Sacral nerve stimulation, also known as sacral neuromodulation, involves the use of an implantable device that delivers electrical impulses to the sacral nerves. This stimulation can help regulate the activity of the pelvic muscles and alleviate symptoms associated with urinary and bowel dysfunction.
In addition to its role in pelvic organ function, the sacral nerve is also involved in modulating pain signals. By stimulating the sacral nerve, it is possible to reduce chronic pain in the pelvic region. This has led to the development of sacral nerve stimulation as a treatment option for chronic pelvic pain syndromes, such as interstitial cystitis and chronic prostatitis.
Furthermore, the sacral nerve has been found to have an impact on sexual function. Stimulation of the sacral nerve can enhance sexual arousal and improve sexual satisfaction. This has led to the exploration of sacral nerve stimulation as a potential treatment for sexual dysfunction, such as erectile dysfunction and female sexual arousal disorder.
Overall, the sacral nerve is a crucial component of the nervous system that regulates the functioning of the pelvic organs. Its intricate anatomy and multifaceted functions make it a target for therapeutic interventions aimed at improving urinary and bowel function, alleviating chronic pain, and enhancing sexual well-being.
Importance of Sacral Nerve Stimulation
Sacral nerve stimulation has gained recognition as an effective treatment for several conditions related to sacral nerve dysfunction. By stimulating the sacral nerve, it is possible to improve bladder control, reduce urinary and fecal incontinence, and alleviate chronic pelvic pain. This technique offers a non-invasive or minimally invasive alternative to traditional treatments, potentially enhancing the quality of life for many individuals.
The sacral nerve, also known as the S3 nerve, plays a crucial role in the regulation of various bodily functions. It is responsible for transmitting signals between the brain and the pelvic organs, including the bladder, bowel, and pelvic floor muscles. When this nerve becomes dysfunctional, it can lead to a range of debilitating symptoms, affecting both physical and emotional well-being.
One of the primary benefits of sacral nerve stimulation is its ability to improve bladder control. For individuals suffering from overactive bladder or urinary incontinence, this treatment can provide significant relief. By modulating the nerve signals responsible for bladder function, sacral nerve stimulation helps restore normal urinary patterns, reducing the frequency and urgency of bathroom visits.
In addition to urinary incontinence, sacral nerve stimulation has also proven effective in treating fecal incontinence. This condition, characterized by the inability to control bowel movements, can be embarrassing and severely impact a person’s daily life. Sacral nerve stimulation works by strengthening the muscles responsible for bowel control, allowing individuals to regain control and improve their overall bowel function.
Health Benefits of Sacral Nerve Stimulation
Sacral nerve stimulation has demonstrated remarkable benefits for patients facing urinary and fecal incontinence, overactive bladder, or chronic pelvic pain. By modulating the nerve signals responsible for these conditions, this technique can help individuals regain control over their bodily functions and alleviate discomfort.
Chronic pelvic pain is another condition that can be effectively managed with sacral nerve stimulation. This type of pain, often originating from the pelvic region, can be debilitating and significantly impact a person’s quality of life. By stimulating the sacral nerve, this treatment helps to block pain signals and provide relief, allowing individuals to engage in daily activities without constant discomfort.
Furthermore, sacral nerve stimulation offers a non-invasive or minimally invasive alternative to traditional treatments such as medication or surgery. This is particularly beneficial for individuals who may not be suitable candidates for more invasive procedures or who prefer to explore less invasive options first. By avoiding extensive surgical interventions, patients can experience faster recovery times, reduced risk of complications, and improved overall well-being.
Potential Risks and Complications
Although sacral nerve stimulation is generally considered safe, it is crucial to be aware of potential risks and complications. These may include infection, pain at the implantation site, discomfort or numbness, device malfunction, or allergic reactions to materials used in the procedure. To mitigate these risks, it is important to consult with a medical professional experienced in sacral nerve stimulation.
Infection is one of the most common risks associated with any surgical procedure, including sacral nerve stimulation. However, with proper preoperative preparation and postoperative care, the risk of infection can be minimized. It is essential to follow all postoperative instructions provided by the healthcare team to ensure optimal healing and reduce the chances of infection.
Pain at the implantation site is another potential complication of sacral nerve stimulation. This discomfort is usually temporary and can be managed with pain medication or other conservative measures. However, if the pain persists or worsens, it is important to seek medical attention to rule out any underlying issues.
Device malfunction is a rare but possible complication of sacral nerve stimulation. This can occur due to various factors, such as battery failure or electrode displacement. Regular follow-up appointments with the healthcare provider are essential to monitor the functioning of the device and address any potential issues promptly.
Lastly, allergic reactions to materials used in the sacral nerve stimulation procedure are rare but can occur. It is crucial to inform the healthcare team about any known allergies or sensitivities to ensure appropriate materials are used during the implantation process.
In conclusion, sacral nerve stimulation offers a valuable treatment option for individuals suffering from sacral nerve dysfunction. By improving bladder control, reducing urinary and fecal incontinence, and alleviating chronic pelvic pain, this technique can significantly enhance the quality of life for many patients. However, it is important to consider the potential risks and complications associated with the procedure and consult with a knowledgeable healthcare professional before undergoing sacral nerve stimulation.
Preparing for Sacral Nerve Stimulation
Prior to undergoing sacral nerve stimulation, several essential steps must be taken to ensure a safe and effective procedure. Seeking medical consultation and obtaining an accurate diagnosis are crucial in determining whether this treatment is suitable for your specific condition.
Medical Consultation and Diagnosis
When considering sacral nerve stimulation, consulting with a healthcare professional is highly recommended. They will conduct a thorough examination, review your medical history, and ascertain whether you are an appropriate candidate for this treatment. Additionally, they may recommend alternative treatments or tests to rule out underlying causes of your symptoms.
During the medical consultation, the healthcare professional will take the time to listen to your concerns and symptoms. They will ask you detailed questions about your medical history, including any previous treatments you have tried and their outcomes. This information will help them determine whether sacral nerve stimulation is the right option for you.
After the initial discussion, the healthcare professional will perform a physical examination. They will carefully assess the affected area and may conduct various tests to gather more information about your condition. These tests may include imaging scans, such as MRI or CT scans, to get a better understanding of the nerve pathways and structures involved.
Based on the findings from the examination and tests, the healthcare professional will provide you with an accurate diagnosis. They will explain the underlying cause of your symptoms and discuss the potential benefits and risks of sacral nerve stimulation as a treatment option.
Pre-Stimulation Preparations
Prior to the actual sacral nerve stimulation procedure, your healthcare team will provide detailed instructions and guidelines to follow. These may include dietary restrictions, medication adjustments, or specific preparatory activities. Adhering to these recommendations will help ensure a successful procedure and minimize potential complications.
One important aspect of pre-stimulation preparations is dietary restrictions. Your healthcare team may advise you to avoid certain foods or beverages that could interfere with the procedure or affect the effectiveness of the treatment. They will provide you with a list of foods to avoid and recommend alternatives to ensure you maintain a balanced diet during this period.
In addition to dietary restrictions, medication adjustments may be necessary. Certain medications can interfere with the procedure or increase the risk of complications. Your healthcare team will review your current medication regimen and make any necessary changes to ensure your safety during the sacral nerve stimulation procedure.
Furthermore, your healthcare team may recommend specific preparatory activities to optimize the outcome of the procedure. These activities may include pelvic floor exercises or relaxation techniques to help relax the muscles in the pelvic region and improve the effectiveness of the treatment.
It is important to follow all the instructions provided by your healthcare team during the pre-stimulation preparations. This will help create an optimal environment for the procedure and increase the chances of a successful outcome.
Techniques for Sacral Nerve Stimulation
When it comes to stimulating the sacral nerve, there are a variety of techniques available, each with its own unique approach and benefits. These techniques range from non-surgical methods to more invasive surgical interventions, providing options for individuals based on their specific needs and preferences.
Non-Surgical Methods
For individuals who prefer non-surgical approaches or have less severe conditions, there are several non-invasive or minimally invasive techniques for sacral nerve stimulation. One such method is transcutaneous electrical nerve stimulation (TENS), which involves the use of external devices to deliver low-voltage electrical currents to the sacral nerve. This gentle stimulation can help alleviate symptoms related to bladder or bowel control issues.
Another non-surgical technique is percutaneous nerve evaluation (PNE), which involves the temporary placement of electrodes near the sacral nerve. This allows for the evaluation of the nerve’s response to stimulation before considering more permanent options. Temporary electrode placement can provide valuable information to healthcare professionals and help guide further treatment decisions.
Temporary electrodes can also be used as a standalone non-surgical method for sacral nerve stimulation. These electrodes are placed externally and can provide relief for individuals experiencing bladder or bowel control issues. While temporary electrodes are not a long-term solution, they can offer temporary relief and serve as a stepping stone towards more permanent interventions.
Surgical Methods
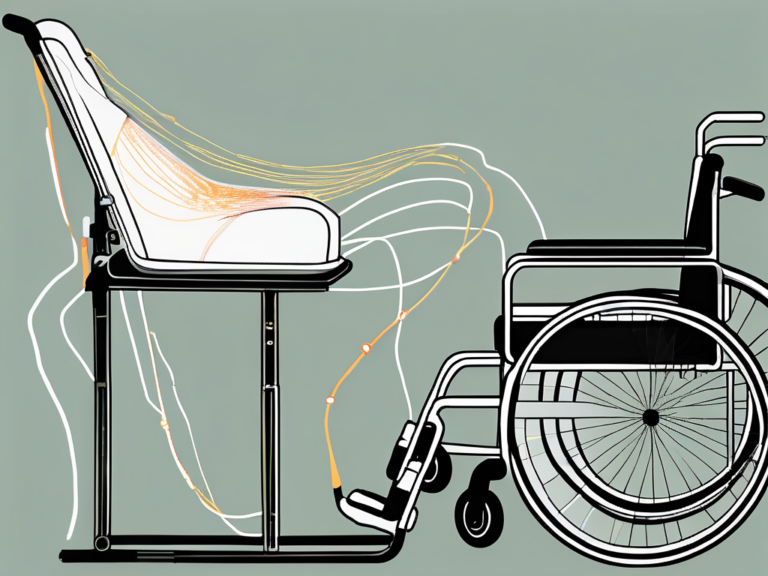
In cases where non-surgical techniques do not provide satisfactory results, surgical interventions may be necessary. Surgical methods for sacral nerve stimulation typically involve the implantation of a neurostimulator device, which delivers electrical impulses directly to the sacral nerve.
During the surgical procedure, an experienced surgeon carefully places the neurostimulator device in a strategic location, ensuring optimal stimulation of the sacral nerve. The device is typically implanted under the skin, and its electrodes are positioned near the sacral nerve to provide targeted stimulation. This surgical approach allows for precise control over the electrical impulses delivered to the nerve, offering potential relief for individuals suffering from bladder or bowel control issues.
It is important to note that surgical methods for sacral nerve stimulation require careful consideration of potential risks and benefits. Before undergoing surgery, individuals should consult with their healthcare professionals to fully understand the procedure, potential complications, and expected outcomes.
In conclusion, the techniques for sacral nerve stimulation offer a range of options for individuals seeking relief from bladder or bowel control issues. From non-surgical methods like TENS and temporary electrode placement to surgical interventions involving the implantation of a neurostimulator device, these techniques provide opportunities for improved quality of life and symptom management.
Post-Stimulation Care and Maintenance
After undergoing sacral nerve stimulation, appropriate care and maintenance are necessary to maximize the treatment’s benefits and ensure optimal long-term outcomes.
Recovery and Rehabilitation
Following sacral nerve stimulation surgery, a period of recovery and rehabilitation is necessary. This may involve restrictions on physical activities, wound care, and regular follow-up appointments with your healthcare professional. Adhering to these post-stimulation guidelines is vital in achieving the best possible outcome.
Long-Term Care and Follow-Up
Sacral nerve stimulation requires ongoing care and periodic follow-up visits with your healthcare team. Regular evaluations of the device’s function, adjustments in stimulation settings if necessary, and addressing any concerns or complications are essential to ensure the longevity of the treatment’s benefits.
Frequently Asked Questions about Sacral Nerve Stimulation
Despite the comprehensive exploration of sacral nerve stimulation, questions may still arise. Here, we address two commonly asked questions regarding this technique.
Is Sacral Nerve Stimulation Painful?
Sacral nerve stimulation is generally well-tolerated, and discomfort during the procedure is minimized through the use of anesthesia. However, individual experiences may vary, and it is essential to discuss any concerns or potential pain management strategies with your healthcare professional.
How Often Should the Sacral Nerve be Stimulated?
The frequency and duration of sacral nerve stimulation are determined on an individual basis, depending on the specific condition being treated and the response to the treatment. Your healthcare professional will determine the most appropriate stimulation parameters, which will be programmed into the neurostimulator device during the initial setup and adjusted if necessary during follow-up appointments.
In conclusion, stimulating the sacral nerve offers a comprehensive approach to address various conditions and improve the overall quality of life. By understanding the anatomy, function, techniques, and post-stimulation care, individuals considering this treatment can make informed decisions in consultation with healthcare professionals. Remember, seeking specialized medical advice is crucial for accurate diagnosis and tailoring treatment to individual needs. With the advancements in sacral nerve stimulation, relief from urinary and fecal incontinence, chronic pelvic pain, and related issues may be within reach for many individuals.