How to Perform Sacral Nerve Stimulation: A Step-by-Step Guide
Sacral nerve stimulation is a procedure that offers hope to patients suffering from a range of pelvic floor dysfunctions, such as urinary or fecal incontinence. In this comprehensive guide, we will walk you through the entire process of performing sacral nerve stimulation, from understanding the science behind it to the post-procedure care and monitoring. It is important to note that this article is not intended to provide medical advice. If you or someone you know is considering sacral nerve stimulation, it is crucial to consult with a healthcare professional.
Understanding Sacral Nerve Stimulation
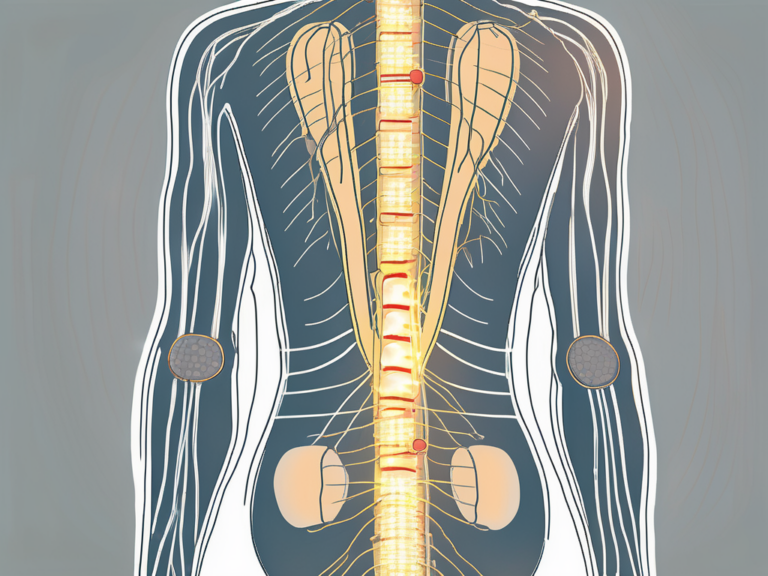
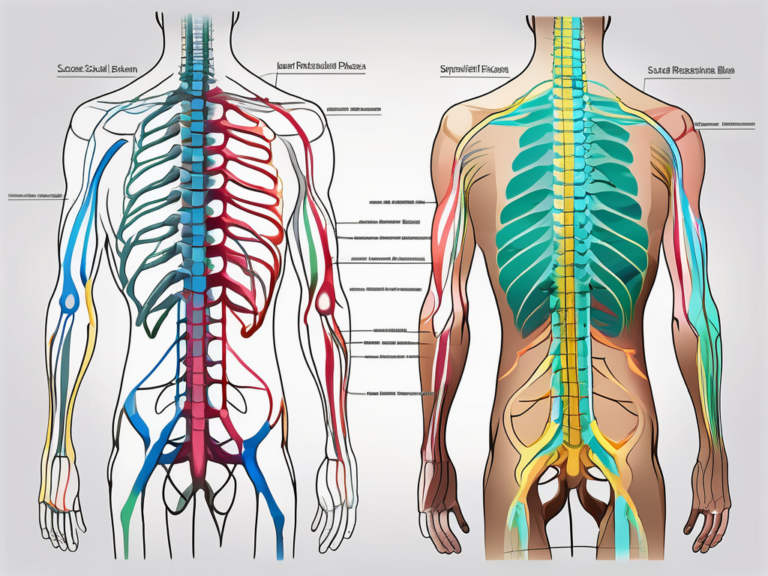
Sacral nerve stimulation is a minimally invasive procedure that involves the implantation of a small device that delivers electrical impulses to the sacral nerves. These sacral nerves play a crucial role in controlling the pelvic floor muscles, which are responsible for urinary and fecal continence. By stimulating these nerves, sacral nerve stimulation can help restore bladder and bowel control in patients who have not responded to conservative treatments.
When it comes to understanding sacral nerve stimulation, it is important to delve into the science behind this innovative procedure. The precise mechanisms by which sacral nerve stimulation works are still not fully understood, but researchers have made significant progress in unraveling its effects on the body. It is believed that the electrical impulses generated by the implantable device modulate the sacral nerves’ activity, leading to improved control over the pelvic floor muscles. These impulses can be adjusted to suit each patient’s individual needs, with the goal of achieving optimal bladder and bowel function.
The Science Behind Sacral Nerve Stimulation
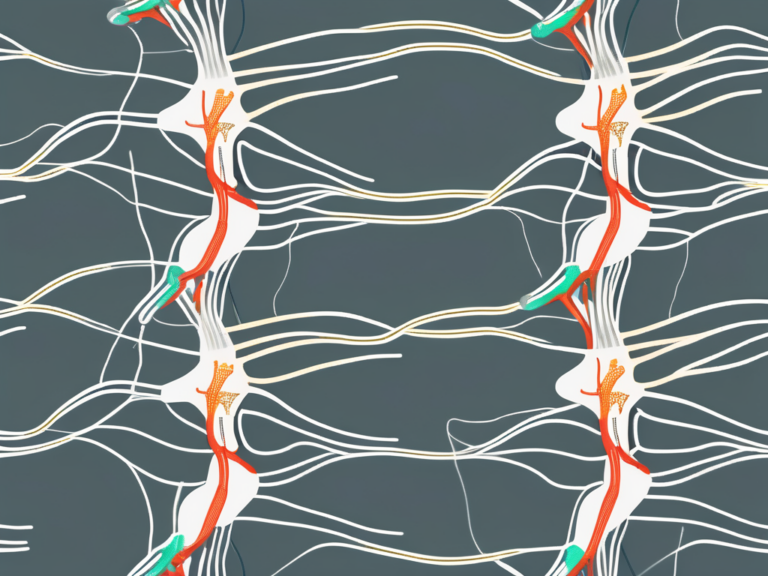
Researchers have conducted various studies to shed light on the science behind sacral nerve stimulation. One study published in the Journal of Urology found that the electrical stimulation of the sacral nerves increases the release of neurotransmitters in the spinal cord, which in turn enhances the communication between the nerves and the pelvic floor muscles. This improved communication allows for better coordination and control, ultimately leading to improved continence.
Another study published in the journal Neuromodulation: Technology at the Neural Interface explored the effects of sacral nerve stimulation on the brain. The researchers used functional magnetic resonance imaging (fMRI) to observe the brain activity of patients undergoing sacral nerve stimulation. They found that the electrical impulses not only affected the sacral nerves but also triggered changes in the brain regions associated with bladder and bowel control. This suggests that sacral nerve stimulation may have a multifaceted impact on the body, involving both peripheral and central nervous system responses.
Benefits and Risks of Sacral Nerve Stimulation
Sacral nerve stimulation offers several potential benefits for patients struggling with pelvic floor disorders. Firstly, it can significantly improve urinary and fecal continence, resulting in a better quality of life. Many patients who have undergone sacral nerve stimulation have reported a reduction in frequency and severity of incontinence episodes, allowing them to regain control over their bodily functions.
Secondly, sacral nerve stimulation is a reversible procedure, with the ability to remove or deactivate the device if necessary. This flexibility provides patients with the reassurance that they can explore alternative treatment options in the future if needed.
However, like any medical intervention, sacral nerve stimulation also carries risks. Infection is a potential complication that can occur after the implantation of the device. It is important for patients to follow strict hygiene protocols and monitor the incision site for any signs of infection. Additionally, device-related complications, such as lead migration or battery failure, may occur in some cases. It is crucial for patients to be aware of these risks and discuss them with their healthcare provider before undergoing the procedure.
Furthermore, sacral nerve stimulation may have undesired side effects. Some patients may experience discomfort or pain at the implantation site, while others may notice changes in bowel or bladder function. These side effects are typically temporary and can be managed with proper medical guidance.
Therefore, it is crucial to carefully weigh the potential benefits against the risks before undergoing sacral nerve stimulation. Patients should have a thorough discussion with their healthcare provider to ensure they have a comprehensive understanding of the procedure and its potential outcomes.
Preparing for Sacral Nerve Stimulation
Before embarking on the sacral nerve stimulation procedure, thorough preparation is necessary. This includes ensuring that the necessary equipment and tools are readily available and adhering to patient preparation guidelines to optimize the chances of a successful outcome.
Sacral nerve stimulation is a minimally invasive procedure that has shown promising results in the treatment of various conditions, including overactive bladder and fecal incontinence. To ensure a smooth and successful procedure, healthcare professionals must have the necessary equipment and tools at their disposal.
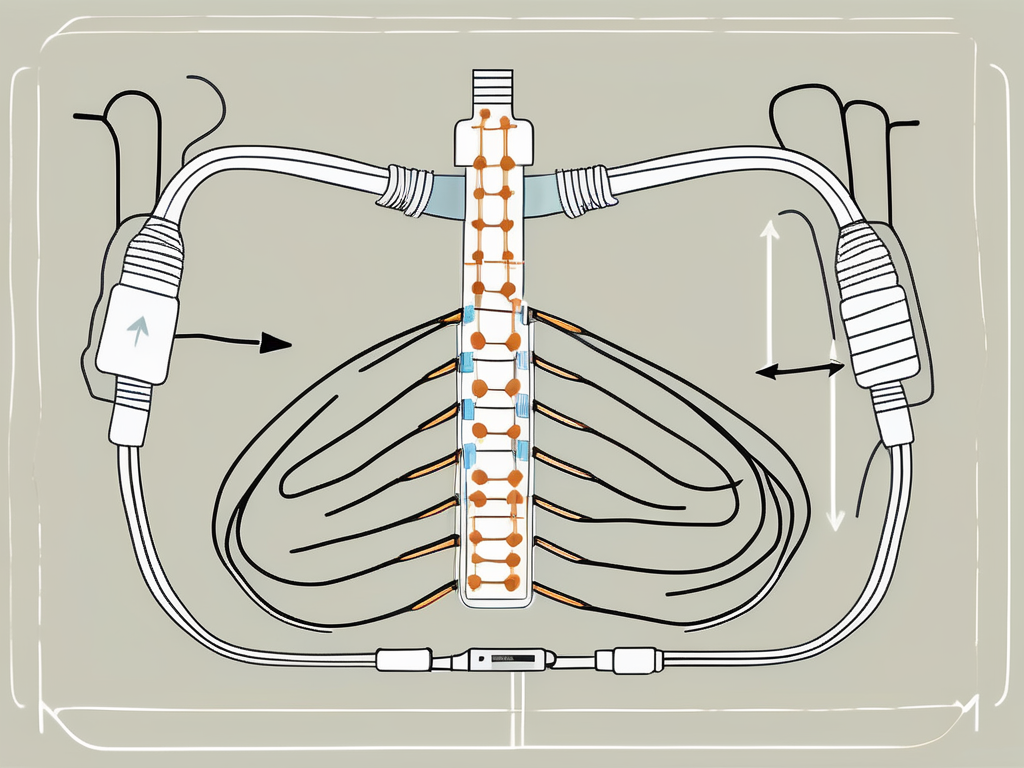
Necessary Equipment and Tools
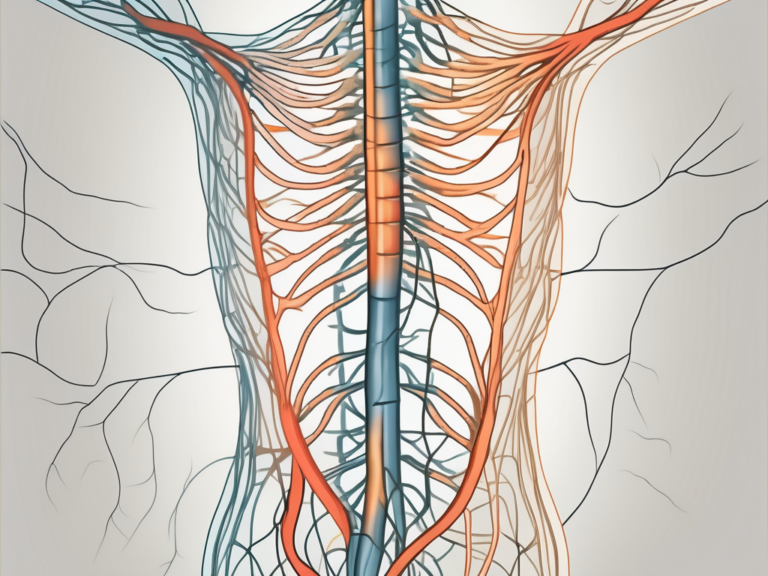
Performing sacral nerve stimulation requires specific equipment and tools that facilitate the implantation of the device and subsequent adjustments. These may include a stimulator generator, electrode leads, and a programming device. These tools are essential for accurately placing the electrode leads and programming the stimulator generator to deliver the appropriate electrical impulses.
The stimulator generator is a small device that is implanted under the skin, typically in the buttock area. It is responsible for generating the electrical impulses that stimulate the sacral nerves, which in turn regulate bladder and bowel function. The electrode leads are thin wires that are placed near the sacral nerves and connected to the stimulator generator. These leads deliver the electrical impulses to the nerves, effectively modulating their activity.
Prior to the procedure, healthcare professionals should ensure that they have access to these items and that they are in optimal working condition. Regular maintenance and calibration of the equipment are crucial to ensure accurate and effective stimulation.
Patient Preparation Guidelines
Prior to the sacral nerve stimulation procedure, patients must be adequately prepared to maximize the chances of a successful outcome. This may include undergoing a thorough medical evaluation to assess their overall health and suitability for the procedure.
During the medical evaluation, healthcare professionals will review the patient’s medical history, perform a physical examination, and may order additional tests. These tests may include urodynamic studies, which provide valuable information about the patient’s bladder and bowel function. Urodynamic studies involve measuring various parameters, such as bladder pressure and flow rate, to assess the underlying cause of the patient’s symptoms.
It is essential that patients fully understand the procedure, its potential benefits and risks, and have realistic expectations. Open communication between the healthcare professional and the patient is vital throughout the entire process. Patients should feel comfortable asking questions and expressing any concerns they may have.
Furthermore, patients should be informed about the post-procedure care and follow-up appointments. Regular follow-up visits are necessary to monitor the effectiveness of the sacral nerve stimulation and make any necessary adjustments to the settings of the stimulator generator.
In conclusion, thorough preparation is crucial for a successful sacral nerve stimulation procedure. Healthcare professionals must ensure that they have the necessary equipment and tools, while patients need to be adequately prepared and informed about the procedure. By following these guidelines, the chances of achieving positive outcomes are significantly increased.
Detailed Procedure of Sacral Nerve Stimulation
The sacral nerve stimulation procedure consists of several key steps, each of which plays a crucial role in achieving optimal outcomes for the patient. By following these steps carefully, healthcare professionals can ensure that they are conducting the procedure accurately and safely.
Step 1: Positioning the Patient
Prior to beginning the procedure, the patient should be placed in a comfortable position. This may involve lying on their back or slightly elevated, depending on the healthcare professional’s preference and the patient’s specific circumstances. Proper positioning is essential to ensure both the patient’s comfort and the healthcare professional’s ease of access to the targeted area.
During the positioning process, the healthcare professional will take into consideration the patient’s body type, any physical limitations they may have, and the specific requirements of the procedure. The goal is to create an environment that allows for optimal visualization and access to the sacral nerve.
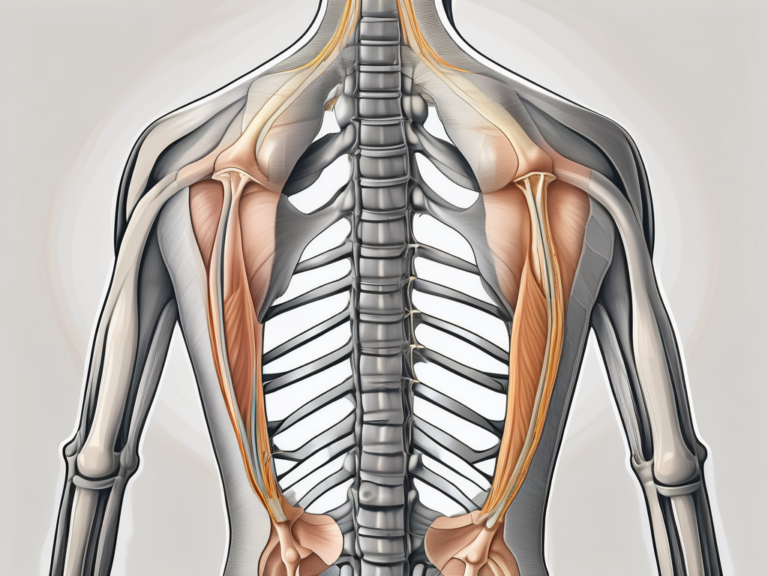
Step 2: Identifying the Sacral Nerve
Once the patient is appropriately positioned, the healthcare professional must locate the sacral nerve. This can be achieved by palpating the area and utilizing anatomical landmarks as a guide. Careful attention should be given to identifying the correct nerve bundle to ensure accurate electrode placement.
During the process of identifying the sacral nerve, the healthcare professional may use imaging techniques such as ultrasound or fluoroscopy to enhance visualization. These tools provide real-time images that aid in locating the nerve and help guide the placement of the electrode with precision.
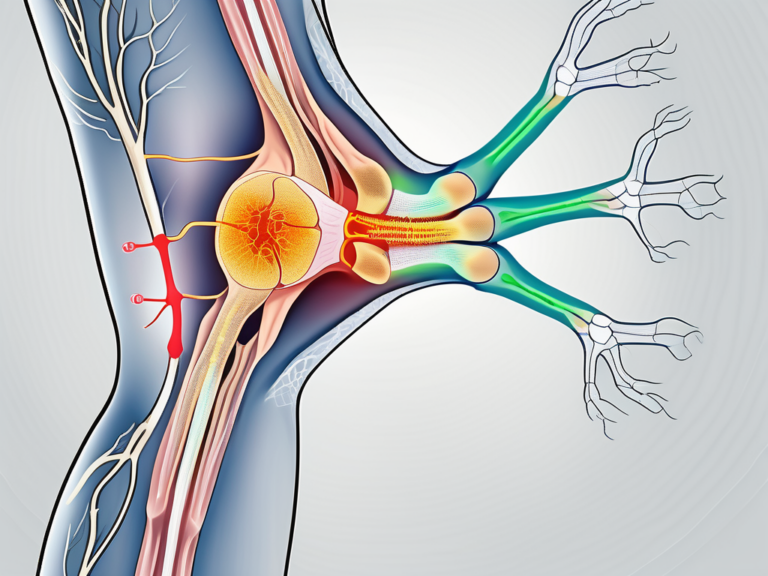
Step 3: Inserting the Electrode
With the sacral nerve identified, the healthcare professional must then insert the electrode. This typically involves making a small incision and carefully maneuvering the electrode to the desired location. Great care should be taken during this step to minimize any potential damage or discomfort to the patient.
The insertion of the electrode requires a delicate touch and a thorough understanding of the anatomy of the sacral region. The healthcare professional will navigate through layers of tissue, ensuring that the electrode is placed in close proximity to the sacral nerve. This precise placement is crucial for effective stimulation and optimal outcomes.
Step 4: Testing and Adjusting the Stimulation
Once the electrode is successfully inserted, the healthcare professional will proceed to test and adjust the stimulation. This entails connecting the electrode to the stimulator generator, which allows for the modulation of the electrical impulses based on the patient’s feedback. The healthcare professional will work closely with the patient to determine the optimal settings that provide the desired symptom relief while minimizing any side effects.
During the testing phase, the healthcare professional will carefully monitor the patient’s response to the stimulation. This may involve assessing changes in pain levels, muscle contractions, or other relevant indicators. The goal is to find the right balance of stimulation that effectively targets the sacral nerve and provides the desired therapeutic effect.
Throughout the adjustment process, the healthcare professional will maintain open communication with the patient, encouraging them to provide feedback on their experience. This collaborative approach ensures that the stimulation settings are tailored to the individual patient’s needs and preferences.
Post-Procedure Care and Monitoring
Following the sacral nerve stimulation procedure, appropriate post-procedure care and monitoring are essential to ensure the patient’s well-being and long-term success.
After the procedure, the patient may experience some discomfort or swelling at the implantation site. This is a normal response to the procedure and should subside gradually over time. Healthcare professionals should provide clear instructions on managing post-procedural pain, wound care, and any necessary activity restrictions.
It is important for patients to follow these instructions closely and promptly seek medical attention if they experience any concerning symptoms, such as excessive bleeding or signs of infection. The healthcare team will provide detailed information on what to expect during the recovery period and how to address any complications that may arise.
While immediate symptom relief may be noticeable, the long-term success of sacral nerve stimulation often requires ongoing follow-up appointments. These appointments allow healthcare professionals to monitor the patient’s progress, make any necessary adjustments to the stimulation settings, and address any concerns or complications that may arise.
During the follow-up appointments, the healthcare professional will assess the patient’s response to the procedure and evaluate the effectiveness of the stimulation. They will carefully review the patient’s symptoms and discuss any changes or improvements that have been observed.
Regular communication between the patient and the healthcare professional is crucial to ensure optimal outcomes. Patients should report any changes in symptoms or concerns they may have during the recovery period. This open line of communication allows the healthcare team to provide appropriate guidance and support.
In addition to monitoring the patient’s progress, the healthcare professional may need to make adjustments to the stimulation settings. This is done to optimize the therapy and ensure the patient continues to experience the desired symptom relief. The adjustments are made based on the patient’s feedback and the healthcare professional’s expertise.
It is important for patients to attend all scheduled follow-up appointments and communicate any changes or concerns they may have. These appointments are an opportunity to address any questions or issues that may arise and to ensure the patient’s long-term success with sacral nerve stimulation.
Troubleshooting Common Issues
Although sacral nerve stimulation has proven to be effective for many patients, it is not without its challenges. Some patients may experience specific issues that require troubleshooting and additional interventions.
When it comes to sacral nerve stimulation, healthcare professionals must be prepared to address a range of potential complications and challenges. While the procedure has shown great promise in improving symptoms and quality of life, it is important to recognize that not every patient will have the same experience. This means that troubleshooting and making adjustments to the treatment plan may be necessary in order to achieve the desired results.
Dealing with Ineffective Stimulation
In some cases, the initial stimulation settings may not provide sufficient symptom relief for the patient. This can be frustrating for both the patient and the healthcare professional involved in their care. However, it is important to approach this challenge with patience and a willingness to explore alternative options.
When faced with ineffective stimulation, healthcare professionals must work closely with the patient to determine alternative settings that may better address their individual needs. This may involve adjusting the frequency, intensity, or duration of the stimulation, or even exploring different electrode placements. It is essential to have open lines of communication with the patient in order to track progress and implement any necessary modifications.
Additionally, it is important to consider other factors that may be contributing to the lack of symptom relief. This could include underlying medical conditions, lifestyle factors, or even psychological factors such as stress or anxiety. By taking a holistic approach to patient care, healthcare professionals can ensure that all aspects of the patient’s well-being are being addressed.
Addressing Patient Discomfort or Complications
While sacral nerve stimulation is generally well-tolerated, some patients may experience discomfort or complications following the procedure. It is crucial for patients to promptly report any unexpected symptoms to their healthcare professional, as early intervention can often prevent further complications.
Depending on the nature and severity of the discomfort or complications, additional interventions may be necessary to address the issue effectively. This could include medication adjustments, physical therapy, or even surgical intervention in rare cases. The specific course of action will depend on the individual patient and their unique circumstances.
It is also important for healthcare professionals to provide patients with the necessary support and resources to manage any discomfort or complications they may experience. This may include education on self-care techniques, access to support groups or counseling services, and ongoing monitoring to ensure that any issues are promptly addressed.
By being proactive in addressing patient discomfort or complications, healthcare professionals can help to minimize any negative impact on the patient’s overall treatment experience. This, in turn, can improve patient satisfaction and outcomes.
Future Developments in Sacral Nerve Stimulation
The field of sacral nerve stimulation continues to evolve, with ongoing research and technological advancements aimed at further improving patient outcomes and expanding the potential applications of this procedure.
Technological Advancements
Advances in technology have led to the development of new and improved sacral nerve stimulation devices. These advancements may include smaller, more comfortable implants, enhanced programming capabilities, and improved battery life. Healthcare professionals should stay abreast of these technological developments to provide their patients with the most up-to-date options.
New Research and Findings
Ongoing research and studies are continuously uncovering new findings about the effectiveness and safety of sacral nerve stimulation. This includes identifying patient selection criteria, refining stimulation protocols, and exploring its potential benefits in a broader range of pelvic floor dysfunctions. Staying informed about the latest research can help healthcare professionals make evidence-based decisions when considering sacral nerve stimulation as a treatment option.
In conclusion, sacral nerve stimulation is a promising procedure for patients with pelvic floor dysfunctions. By understanding the science behind it, adequately preparing for the procedure, and providing appropriate post-procedure care, healthcare professionals can maximize the chances of successful outcomes. However, it is crucial for patients to seek guidance from a healthcare professional, who can guide them through the process and ensure individualized care. Consultation with a healthcare professional is a vital step in determining if sacral nerve stimulation is the right course of action for each individual patient.