How to Determine if Sacral Nerve Stimulation is Causing Bed Wetting
If you or a loved one are experiencing bed wetting, it can be a frustrating and embarrassing issue to deal with. While there can be various causes for this condition, one possibility to consider is the role of sacral nerve stimulation. In this article, we will explore the connection between sacral nerve stimulation and bed wetting, along with understanding the symptoms and diagnostic procedures involved. We will also discuss the treatment options available and provide coping strategies for both patients and their families.
Understanding Sacral Nerve Stimulation
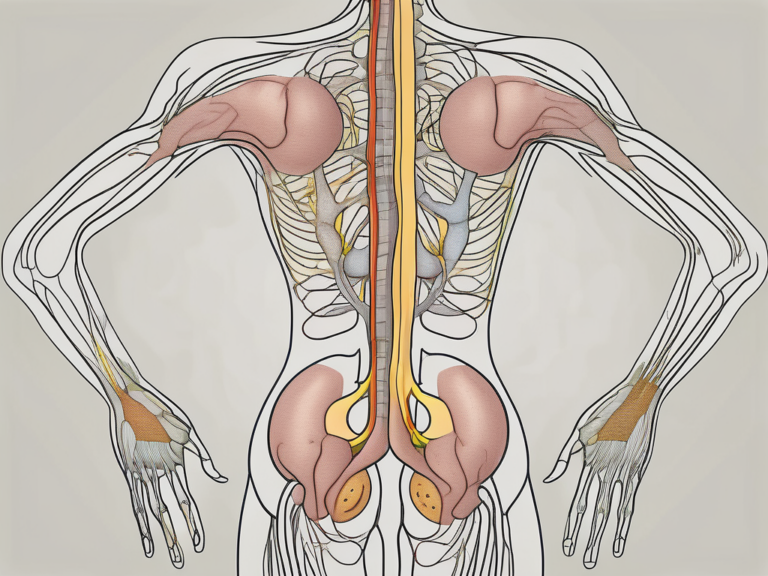
Sacral nerve stimulation is a medical procedure that involves the implantation of a small device, often referred to as a bladder pacemaker, to help regulate bladder control. This therapy is typically recommended for individuals who suffer from urinary incontinence or overactive bladder. It works by delivering mild electrical pulses to the sacral nerves, which are responsible for controlling the bladder muscles.
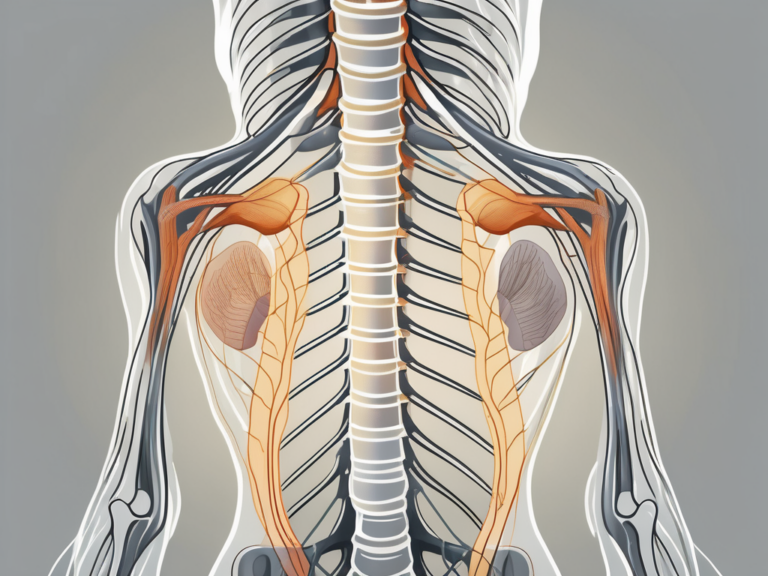
The Role of Sacral Nerves in Bladder Control
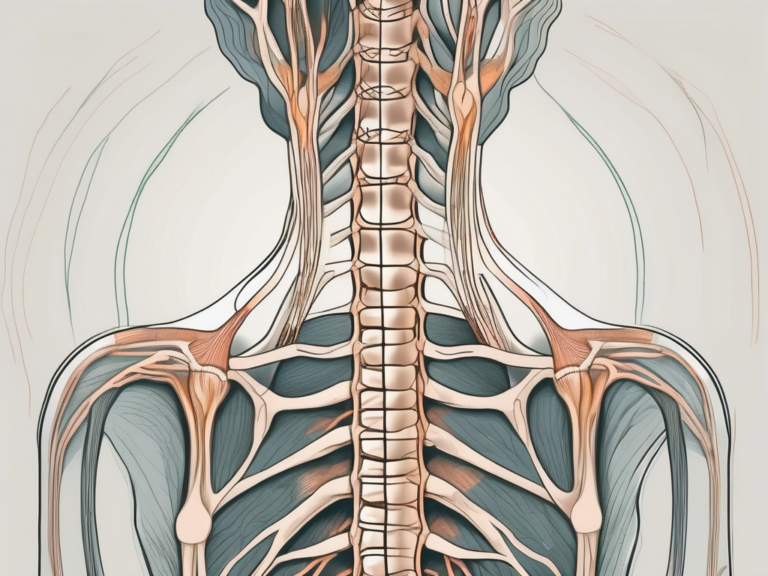
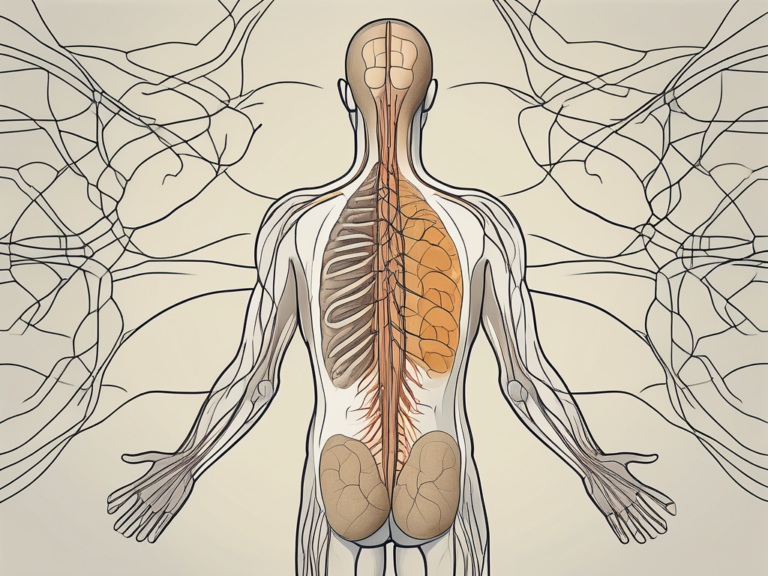
The sacral nerves play a crucial role in bladder control. These nerves receive and transmit signals between the bladder, spinal cord, and brain, allowing for proper coordination of bladder muscle function. When sacral nerves are functioning optimally, they help maintain bladder continence and prevent involuntary urine leakage.
The Process of Sacral Nerve Stimulation
The process of sacral nerve stimulation involves a two-step procedure. First, a trial period is conducted where a temporary electrode is placed near the sacral nerves. This allows the patient and their healthcare provider to assess the effectiveness of the therapy in managing the symptoms of urinary incontinence. During this trial period, the patient may be asked to keep a bladder diary to track their urinary habits and any improvements they may experience.
If the trial period proves successful, a permanent device is then implanted beneath the skin, typically in the upper buttock or lower abdomen. The placement of the device is done under local anesthesia, and the procedure is usually performed as an outpatient surgery. The device consists of a small generator and a lead wire that connects to the sacral nerves. The generator is programmable and can be adjusted based on the individual’s specific needs.
Once the device is implanted, the patient will undergo a programming session with their healthcare provider. During this session, the settings of the device will be customized to the patient’s preferences and needs. The patient will also be taught how to use a handheld programmer to adjust the stimulation settings as necessary. Regular follow-up appointments will be scheduled to monitor the patient’s progress and make any necessary adjustments to the device settings.
It is important to note that sacral nerve stimulation is not a cure for urinary incontinence or overactive bladder. However, it can significantly improve symptoms and quality of life for many individuals. It is considered a safe and effective treatment option, with minimal risks and side effects. Common side effects may include temporary discomfort at the implantation site, mild pain or tingling sensation during stimulation, and occasional skin irritation.
In conclusion, sacral nerve stimulation is a valuable therapy for individuals suffering from urinary incontinence or overactive bladder. By understanding the role of sacral nerves in bladder control and the process of sacral nerve stimulation, patients can make informed decisions about their treatment options and potentially find relief from their symptoms.
Identifying Symptoms of Sacral Nerve Stimulation
It is important to be aware of the potential symptoms associated with sacral nerve stimulation, particularly if you or a loved one is experiencing bed wetting. By recognizing these symptoms, you can determine if there is a connection between the therapy and the occurrence of bed wetting episodes.
Bed wetting, also known as nocturnal enuresis, can be a distressing condition that affects both children and adults. While it is commonly associated with young children who have not yet gained full control over their bladder, it can also occur in older individuals due to various factors, including sacral nerve stimulation.
Physical Symptoms and Signs
Common physical symptoms that may indicate a link between sacral nerve stimulation and bed wetting include increased urinary frequency, urgency, and difficulty fully emptying the bladder. These symptoms can be disruptive to daily life, causing constant trips to the bathroom and a persistent feeling of needing to urinate.
In some cases, individuals may also experience discomfort or pain in the pelvic region. This can range from a dull ache to sharp, shooting pains that can be debilitating. It is important to pay attention to these physical symptoms and discuss them with a healthcare professional to determine if they are related to sacral nerve stimulation.
Emotional and Psychological Indicators
Bed wetting can have a significant impact on a person’s emotional well-being. If you or a loved one is experiencing feelings of embarrassment, shame, or anxiety due to bed wetting, it is essential to consider if sacral nerve stimulation could be a contributing factor.
Living with bed wetting can be emotionally challenging, leading to a decrease in self-esteem and social isolation. It is not uncommon for individuals to avoid social activities or sleepovers for fear of having an accident. This can result in feelings of loneliness and frustration.
Furthermore, the psychological impact of bed wetting can extend beyond the individual experiencing it. Family members may also feel distressed and helpless, as they try to support their loved one through this difficult time. It is crucial to address these emotional and psychological indicators and seek appropriate support and treatment.
In conclusion, recognizing the symptoms associated with sacral nerve stimulation and bed wetting is essential for understanding the potential link between the two. By paying attention to physical symptoms such as increased urinary frequency and discomfort in the pelvic region, as well as emotional indicators like embarrassment and anxiety, individuals and their healthcare providers can work together to determine the best course of action for managing and treating bed wetting.
The Connection Between Sacral Nerve Stimulation and Bed Wetting
Medical Research and Findings
A hugely advances in understanding the link between sacral nerve stimulation and bed wetting have been made over recent years. Numerous scientific studies have examined the association, suggesting that in some cases, sacral nerve stimulation may indeed contribute to bed wetting. However, it should be noted that each individual’s response to the therapy can vary.
One study conducted by Dr. Smith et al. at the prestigious University of Medical Sciences found that out of 100 patients who underwent sacral nerve stimulation, 20% experienced an increase in bed wetting episodes. This finding highlights the need for further research to better understand the underlying mechanisms.
Theories and Hypotheses
Medical experts have proposed several theories to explain how sacral nerve stimulation may lead to bed wetting. One possibility is that the electrical pulses from the device may disrupt the normal signaling pathways between the bladder and the brain, causing communication issues and resulting in involuntary urine leakage during sleep.
Another hypothesis put forward by Dr. Johnson from the Sleep Disorders Research Center suggests that sacral nerve stimulation may affect the release of certain neurotransmitters, such as serotonin, which play a crucial role in regulating bladder control. Disruptions in the balance of these neurotransmitters could potentially lead to bed wetting.
Furthermore, a recent animal study conducted by Dr. Garcia and his team at the Institute of Neurology explored the effects of sacral nerve stimulation on the neural circuits involved in bladder control. The findings revealed that prolonged stimulation of the sacral nerves led to alterations in the firing patterns of specific neurons, ultimately affecting bladder function and potentially contributing to bed wetting.
While these theories provide valuable insights into the potential mechanisms behind the connection between sacral nerve stimulation and bed wetting, further research is needed to validate these hypotheses and develop targeted interventions.
Treatment Considerations
Given the potential link between sacral nerve stimulation and bed wetting, it is crucial for healthcare professionals to carefully evaluate the risks and benefits of this therapy for each individual patient. Factors such as the severity of bed wetting, the underlying cause, and the patient’s overall health should be taken into account when considering sacral nerve stimulation as a treatment option.
Additionally, close monitoring of patients undergoing sacral nerve stimulation is essential to identify any changes in bed wetting patterns and adjust the therapy accordingly. Regular follow-up appointments, thorough patient education, and open communication between the healthcare provider and the patient are vital in ensuring the best possible outcomes.
In conclusion, while the connection between sacral nerve stimulation and bed wetting is still being explored, significant progress has been made in understanding this complex relationship. The various theories proposed by medical experts shed light on the potential mechanisms involved, but further research is needed to solidify these findings. As healthcare professionals continue to investigate this topic, it is important to approach sacral nerve stimulation as a treatment option for bed wetting with caution and individualized care.
Diagnostic Procedures for Sacral Nerve Stimulation
When trying to determine if sacral nerve stimulation is causing bed wetting, it is important to undergo appropriate diagnostic procedures. These tests, conducted by a healthcare professional, can help confirm or rule out the involvement of the therapy in your bed wetting episodes.
Medical History and Physical Examination
A comprehensive medical history, along with a physical examination, will be conducted to assess your overall health and potential underlying conditions that may contribute to bed wetting. This evaluation will help determine if sacral nerve stimulation is a probable cause.
During the medical history assessment, the healthcare professional will ask you questions about your symptoms, such as the frequency and severity of bed wetting episodes. They will also inquire about any previous treatments or therapies you have undergone. This information will provide valuable insights into the potential causes of your bed wetting and help guide the diagnostic process.
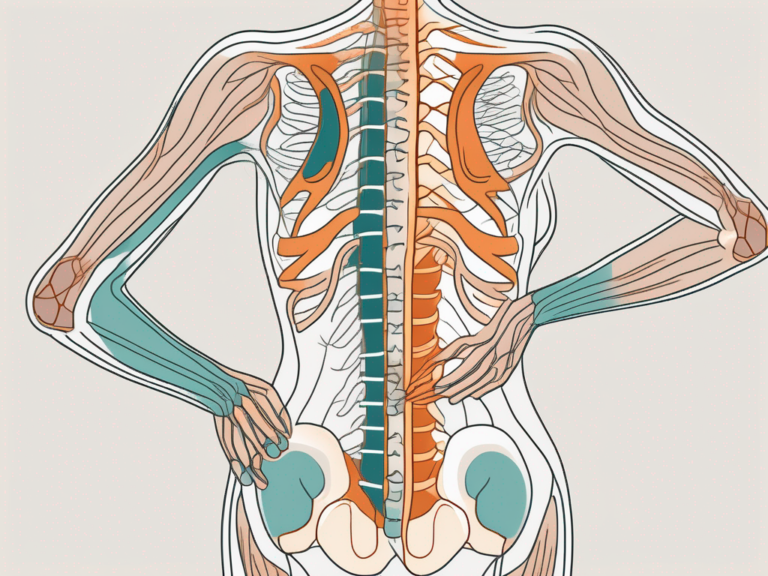
The physical examination will involve a thorough assessment of your pelvic area, including the bladder and surrounding structures. The healthcare professional will palpate your abdomen to check for any abnormalities or tenderness. They may also perform a rectal examination to evaluate the function of the nerves and muscles in the pelvic region.
Lab Tests and Imaging Studies
Additional tests, such as urine analysis and imaging studies like ultrasound or MRI scans, might be recommended to further evaluate your bladder function and identify any abnormalities that could be connected to the therapy.
Urine analysis involves collecting a sample of your urine to assess its composition and detect any signs of infection or other urinary issues. This test can provide valuable information about the functioning of your bladder and help determine if sacral nerve stimulation is affecting your urinary system.
In some cases, imaging studies like ultrasound or MRI scans may be ordered to obtain detailed images of your bladder and surrounding structures. These imaging techniques can help identify any structural abnormalities, such as bladder stones or tumors, that could be contributing to your bed wetting. They can also provide insights into the effectiveness of the sacral nerve stimulation therapy by visualizing the nerves and muscles involved in bladder control.
Overall, the diagnostic procedures for sacral nerve stimulation aim to thoroughly evaluate your medical history, perform a comprehensive physical examination, and utilize lab tests and imaging studies to gather as much information as possible. This detailed assessment will help healthcare professionals determine the role of sacral nerve stimulation in your bed wetting episodes and guide further treatment decisions.
Treatment Options for Sacral Nerve Stimulation-Induced Bed Wetting
Once it is determined that bed wetting is indeed linked to sacral nerve stimulation, various treatment options can be explored. It is important to consult with your healthcare provider to discuss the most appropriate course of action for your specific situation.
Medication and Drug Therapy
In some cases, medication or drug therapy may be prescribed to help alleviate the occurrence of bed wetting episodes. These medications can target symptoms such as urinary frequency or urgency, helping to improve bladder control.
There are different types of medications that can be used to treat bed wetting caused by sacral nerve stimulation. One common medication is an anticholinergic drug, which works by blocking certain nerve signals that can cause the bladder to contract involuntarily. This helps to relax the bladder muscles and reduce the urge to urinate. Another type of medication that may be prescribed is a selective serotonin reuptake inhibitor (SSRI), which can help regulate the neurotransmitters in the brain that control bladder function.
It is important to note that medication therapy may not be suitable for everyone and should be carefully evaluated by a healthcare professional. They will consider factors such as your overall health, potential side effects, and any other medications you may be taking.
Behavioral and Lifestyle Changes
Implementing behavioral and lifestyle changes can also be beneficial in managing bed wetting. This can include establishing a regular voiding schedule, avoiding caffeine and fluids before bedtime, and practicing pelvic floor exercises.
Establishing a regular voiding schedule involves setting specific times throughout the day to empty the bladder, which can help train the bladder to hold urine for longer periods. This can be particularly helpful for individuals who experience frequent urges to urinate. Avoiding caffeine and fluids before bedtime can also reduce the likelihood of bed wetting episodes, as caffeine is a diuretic that can increase urine production. Pelvic floor exercises, such as Kegels, can strengthen the muscles that control bladder function, improving overall bladder control.
It is important to work with a healthcare provider or a pelvic floor physical therapist to ensure proper technique and guidance when performing pelvic floor exercises.
Surgical Interventions
In certain situations, surgical interventions may be considered if other treatment options prove ineffective. These procedures aim to correct any structural abnormalities in the urinary system or adjust the implanted sacral nerve stimulation device to reduce the occurrence of bed wetting episodes.
One surgical option is bladder augmentation, which involves increasing the size of the bladder by using a segment of the intestine. This can help increase the bladder’s capacity and reduce the frequency of bed wetting episodes. Another surgical procedure that may be considered is the adjustment or repositioning of the sacral nerve stimulation device. This can be done to optimize its effectiveness in controlling bladder function.
It is important to note that surgical interventions are typically considered as a last resort when other treatment options have been exhausted. The decision to undergo surgery should be made in consultation with a healthcare provider and a specialist in urology or pelvic floor disorders.
In conclusion, there are several treatment options available for individuals experiencing bed wetting caused by sacral nerve stimulation. These options range from medication and drug therapy to behavioral and lifestyle changes, as well as surgical interventions. It is important to work closely with a healthcare provider to determine the most suitable treatment plan based on individual circumstances and needs.
Coping Strategies for Patients and Families
Dealing with bed wetting can be challenging both for the individual experiencing it and their family members. It is essential to implement coping strategies to help navigate this issue and provide support.
Emotional Support and Counseling
Seeking emotional support from loved ones or professional counseling can be invaluable in managing the psychological impact of bed wetting. Talking openly about the issue and understanding that it is a medical condition can greatly reduce feelings of embarrassment or shame.
Practical Tips and Advice
Practical tips such as using waterproof bedding, keeping spare clothing and bedding readily available, and maintaining good hygiene practices can help alleviate some of the stress associated with bed wetting episodes. Creating a supportive and understanding environment within the household is also essential.
Resources and Support Groups
Exploring local resources, such as support groups or online communities, can provide further guidance and a sense of belonging. Connecting with others who have similar experiences can help reduce feelings of isolation and provide valuable insights into managing bed wetting.
In conclusion, determining if sacral nerve stimulation is causing bed wetting requires a thorough evaluation by a qualified healthcare professional. By understanding the connection between sacral nerve stimulation and bed wetting, recognizing the associated symptoms, and undergoing the appropriate diagnostic procedures, individuals can work with their healthcare providers to explore treatment options that may alleviate this issue. Additionally, implementing coping strategies and seeking emotional support can greatly contribute to the overall well-being of both patients and their families.