How Much Sacral Nerve Stimulation is Needed: A Comprehensive Guide
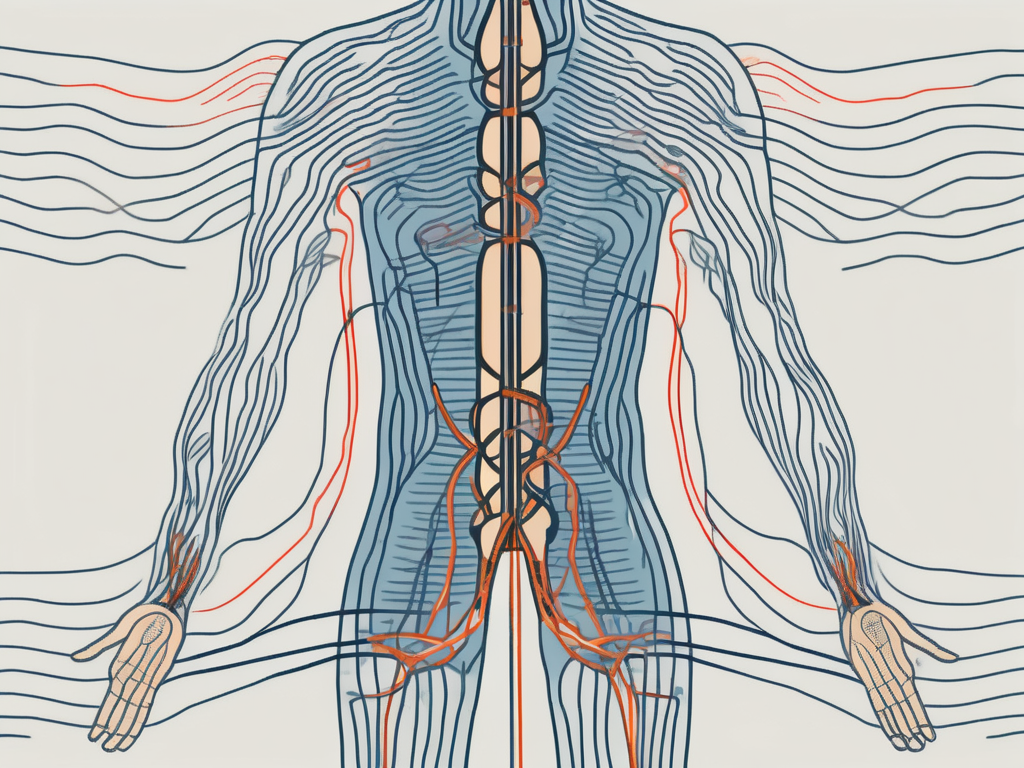
Sacral Nerve Stimulation (SNS) is a medical treatment used to alleviate various conditions affecting the sacral nerves in the body. These nerves play a crucial role in the functioning of the pelvic organs, including the bladder and bowels. By modulating the electrical impulses in the sacral nerves, SNS can provide relief from symptoms such as urinary and fecal incontinence, overactive bladder, and pelvic pain.
Understanding Sacral Nerve Stimulation
The Role of Sacral Nerves in the Body
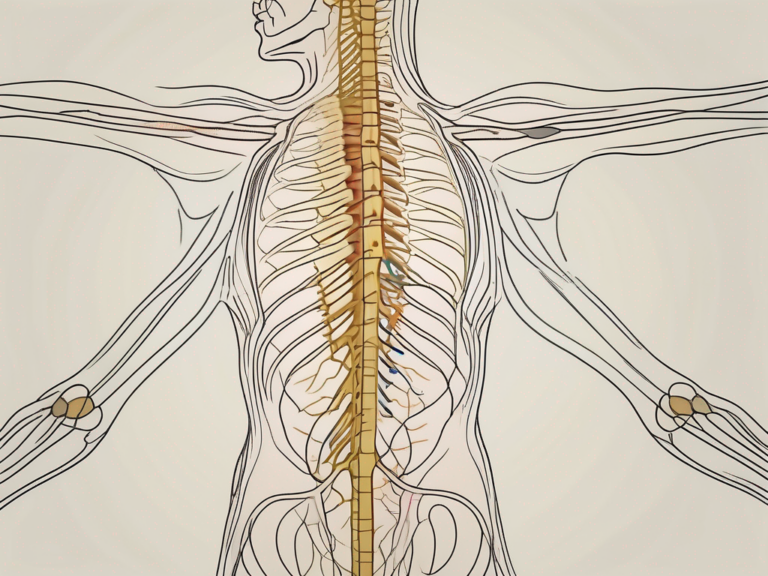
The sacral nerves, located in the lower part of the spinal cord, play a crucial role in the overall functioning of the human body. These nerves are responsible for transmitting signals between the brain and the pelvic organs, ensuring proper communication and coordination.
One of the primary functions of the sacral nerves is to control the bladder and bowel muscles. These nerves send signals to the muscles, instructing them to contract or relax, allowing for proper urination and defecation. Without the sacral nerves, these essential bodily functions would be compromised, leading to urinary and bowel dysfunctions.
In addition to controlling muscle movements, the sacral nerves also regulate sensations in the pelvic region. They enable individuals to perceive and interpret various sensations, such as pressure, pain, and temperature, in the lower abdomen and pelvic area.
The Basics of Sacral Nerve Stimulation
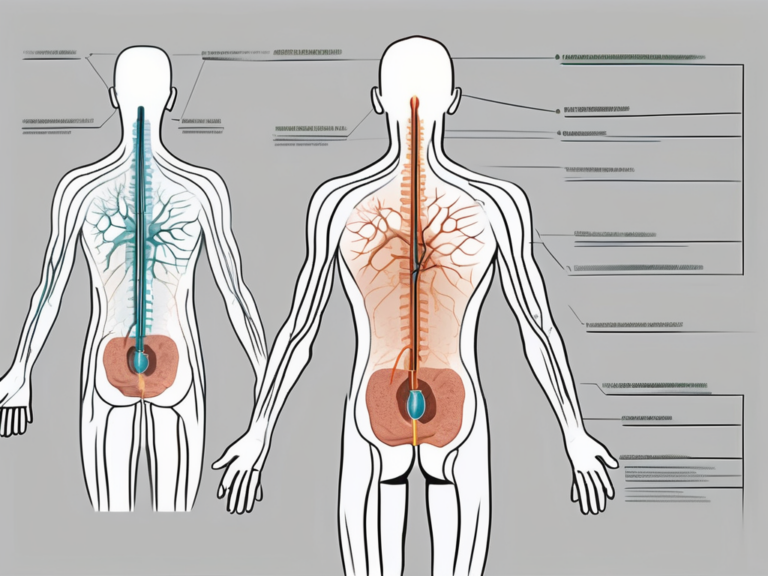
Sacral Nerve Stimulation, also known as sacral neuromodulation, is a medical procedure that aims to restore normal communication between the brain and the pelvic organs. It involves the implantation of a device called a neurostimulator, which delivers mild electrical pulses to the sacral nerves.
During the surgical procedure, the neurostimulator is carefully placed under the skin in the buttock or lower abdomen. This placement ensures that the device remains discreet and comfortable for the patient. Once implanted, the neurostimulator is connected to thin wires, called leads, which are strategically positioned near the sacral nerves.
When the neurostimulator is activated, it generates electrical pulses that stimulate the sacral nerves. These electrical pulses help to modulate the nerve activity, effectively restoring the normal functioning of the pelvic organs. By improving the communication between the brain and the pelvic region, sacral nerve stimulation can alleviate symptoms associated with urinary and bowel dysfunctions.
It is important to note that sacral nerve stimulation is a reversible treatment option. The neurostimulator can be easily turned on or off, adjusted, or completely removed if necessary. This flexibility allows healthcare professionals to customize the treatment according to each patient’s specific needs and preferences.
Furthermore, sacral nerve stimulation is considered a safe and effective treatment option for individuals who have not responded well to other conservative therapies. It offers hope and improved quality of life for those who have been struggling with urinary and bowel dysfunctions.
In conclusion, sacral nerve stimulation is a remarkable medical procedure that harnesses the power of electrical pulses to restore normal communication between the brain and the pelvic organs. By understanding the role of sacral nerves in the body and the basics of this innovative treatment, individuals can make informed decisions about their healthcare options and potentially find relief from urinary and bowel dysfunctions.
Determining the Need for Sacral Nerve Stimulation
Identifying Symptoms that Require Stimulation
Before considering sacral nerve stimulation, it’s crucial to identify the symptoms that may benefit from this treatment. Common indications include urinary and fecal incontinence, urgency, frequency, and incomplete emptying of the bladder or bowels. These symptoms can significantly impact an individual’s quality of life and may not respond to conservative therapies.
Individuals experiencing urinary incontinence may find themselves constantly worried about embarrassing leaks and accidents. The constant need to wear protective pads or diapers can be frustrating and restrict their daily activities. Similarly, those with fecal incontinence may feel embarrassed and isolated, as they struggle to control their bowel movements.
Furthermore, individuals dealing with urgency and frequency may experience a constant urge to urinate, even when their bladder is not full. This can disrupt their sleep, work, and social life, leading to increased stress and anxiety.
Incomplete emptying of the bladder or bowels can also be a distressing symptom. It may result in a feeling of constant discomfort, as if there is always something left behind. This can lead to recurring urinary tract infections and other complications.
However, it’s essential to consult with a healthcare professional who can provide a proper evaluation and diagnosis. Only a trained physician can determine if sacral nerve stimulation is an appropriate treatment option for your specific condition.
Medical Conditions that Benefit from Stimulation
Sacral nerve stimulation has shown promising results in various medical conditions, including:
- Overactive bladder
- Urinary retention
- Bladder pain syndrome/Interstitial cystitis
- Fecal incontinence
- Chronic pelvic pain
Overactive bladder is a condition characterized by a sudden and uncontrollable urge to urinate, often resulting in urinary incontinence. This can be highly disruptive to an individual’s daily routine and social life, causing embarrassment and anxiety.
Urinary retention, on the other hand, refers to the inability to empty the bladder completely. This can lead to discomfort, frequent urinary tract infections, and even kidney damage if left untreated.
Bladder pain syndrome, also known as interstitial cystitis, is a chronic condition that causes bladder pain and a frequent need to urinate. The pain can be intense and may significantly impact an individual’s quality of life.
Fecal incontinence, as mentioned earlier, is the inability to control bowel movements. This can lead to embarrassing accidents and a constant fear of leakage, affecting an individual’s self-esteem and social interactions.
Chronic pelvic pain is a complex condition that can have various causes, including nerve damage. It can result in persistent pain in the pelvic region, affecting daily activities and overall well-being.
These conditions can significantly impact an individual’s daily life, causing discomfort and affecting their emotional well-being. Sacral nerve stimulation may offer relief and improve the overall quality of life for those affected.
The Process of Sacral Nerve Stimulation
Pre-Stimulation Evaluation and Preparation
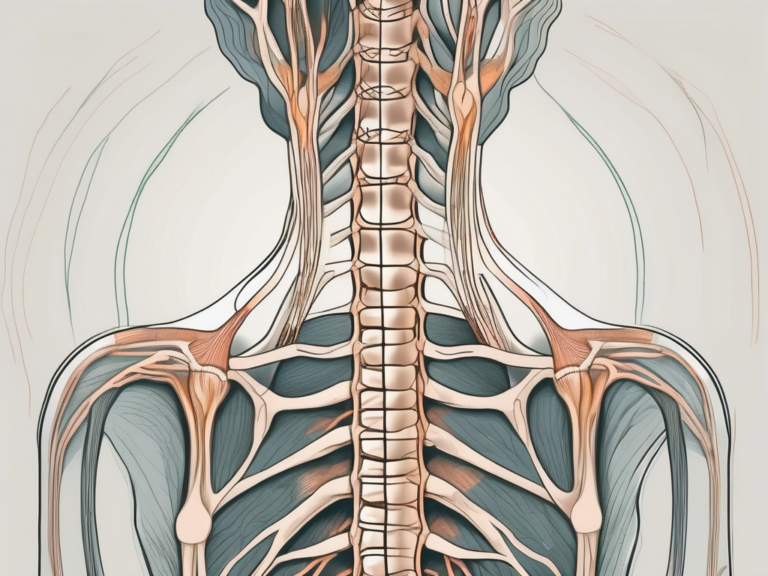
Before undergoing sacral nerve stimulation, a comprehensive assessment is necessary to determine the appropriateness of the treatment. This evaluation typically involves a detailed medical history, physical examination, urodynamic testing, and possibly additional investigations such as imaging studies.
During the medical history assessment, the healthcare provider will inquire about the patient’s symptoms, previous treatments, and any underlying medical conditions. This information helps in understanding the patient’s specific needs and tailoring the treatment accordingly.
The physical examination involves a thorough examination of the pelvic region, including the genitals, to assess any anatomical abnormalities or signs of nerve dysfunction. Additionally, the healthcare provider may perform a neurological examination to evaluate the function of the sacral nerves and surrounding structures.
Urodynamic testing is a crucial part of the evaluation process. It involves measuring various parameters related to bladder and bowel function, such as bladder capacity, pressure during voiding, and the ability to control urine flow. These tests help in identifying the underlying cause of the patient’s symptoms and determining if sacral nerve stimulation is a suitable treatment option.
Once deemed a suitable candidate, the patient and healthcare provider can discuss the potential benefits, risks, and expectations associated with sacral nerve stimulation. The patient’s particular goals and desires should also be taken into consideration during this process. Open communication between the patient and healthcare provider is essential to ensure that the treatment plan aligns with the patient’s needs and expectations.
The Procedure of Sacral Nerve Stimulation
The implantation of the neurostimulator is performed in a hospital or outpatient setting under local or general anesthesia. The choice of anesthesia depends on the patient’s preference, the complexity of the procedure, and the healthcare provider’s recommendation.
During the procedure, one or two thin leads, equipped with electrode contacts, are inserted near the sacral nerves. These leads are carefully guided using fluoroscopy or ultrasound imaging to ensure accurate placement. The electrode contacts are strategically positioned to target the specific nerves involved in bladder and bowel control.
Once the leads are in place, they are connected to the neurostimulator, which is placed under the skin, usually in the lower abdomen or buttock area. The neurostimulator is a small device that generates electrical impulses to stimulate the sacral nerves. It is programmable, allowing the healthcare provider to adjust the stimulation settings according to the patient’s needs.
Following the surgery, a trial period is often conducted where the neurostimulator’s settings are adjusted to find the optimal stimulation levels. This trial period typically lasts for a few days to several weeks, during which the patient closely monitors their symptoms and provides feedback to the healthcare provider. This feedback helps in fine-tuning the stimulation parameters to achieve the best possible outcomes.
If the trial period is successful in alleviating symptoms and improving the patient’s quality of life, a permanent neurostimulator may be implanted. The permanent implantation involves a similar procedure to the trial, but with the intention of long-term use. The patient can expect ongoing follow-up appointments to ensure the neurostimulator’s optimal functioning and make any necessary adjustments.
Factors Influencing the Amount of Stimulation Needed
Individual Health Factors
Every individual has unique health considerations that may influence the amount of sacral nerve stimulation needed. Factors such as age, overall health, medical history, and any coexisting medical conditions can impact the treatment outcome. It’s crucial for the healthcare provider to consider these factors when determining the optimal stimulation levels.
Age plays a significant role in determining the amount of stimulation needed. Older individuals may require higher levels of stimulation due to age-related changes in nerve sensitivity. On the other hand, younger individuals may respond well to lower levels of stimulation due to their more robust nerve function.
Overall health is another crucial factor to consider. Individuals with chronic health conditions, such as diabetes or cardiovascular disease, may require higher levels of stimulation to overcome the effects of their underlying condition. Conversely, individuals with excellent overall health may require lower levels of stimulation to achieve the desired therapeutic effect.
Medical history also plays a role in determining the amount of stimulation needed. Individuals with a history of nerve damage or previous surgeries in the pelvic region may require higher levels of stimulation to compensate for any loss of nerve function. Conversely, individuals with a clean medical history may respond well to lower levels of stimulation.
Coexisting medical conditions can further complicate the stimulation requirements. For example, individuals with urinary incontinence and chronic pain may require higher levels of stimulation to address both conditions simultaneously. The healthcare provider must carefully assess and manage these coexisting conditions to determine the optimal stimulation levels.
Severity of Symptoms and Medical Condition
The severity of symptoms and the underlying medical condition requiring sacral nerve stimulation will also impact the amount of stimulation needed. In some cases, individuals may require higher levels of stimulation to achieve optimal symptom relief, while others may respond well to lower levels. The healthcare provider will carefully adjust the neurostimulator settings to meet the individual’s specific needs.
The severity of symptoms is a crucial factor in determining the amount of stimulation required. Individuals with severe symptoms, such as frequent and uncontrollable bladder contractions or chronic pelvic pain, may require higher levels of stimulation to effectively manage their condition. Conversely, individuals with milder symptoms may find relief with lower levels of stimulation.
The underlying medical condition also plays a significant role. For example, individuals with overactive bladder syndrome may require higher levels of stimulation to control their frequent urge to urinate. On the other hand, individuals with chronic pelvic pain syndrome may require lower levels of stimulation to alleviate their discomfort.
It’s important to note that the amount of stimulation needed may vary over time. As the individual’s medical condition evolves, the healthcare provider may need to adjust the stimulation levels accordingly. Regular follow-up appointments and open communication between the individual and healthcare provider are essential to ensure optimal treatment outcomes.
Potential Risks and Complications of Sacral Nerve Stimulation
Sacral nerve stimulation is a medical procedure that offers potential benefits for individuals with certain conditions. However, as with any medical procedure, it is important to be aware of the potential risks and complications that may arise. By understanding these risks, individuals can make informed decisions and work closely with their healthcare providers to manage any complications that may occur.
Short-term Risks and Complications
Short-term risks and complications associated with sacral nerve stimulation are relatively low but should still be considered. One potential risk is the risk of infection at the implantation site. While rare, infections can occur and may require treatment with antibiotics. Another possible complication is bleeding, which may happen during the implantation procedure. However, healthcare providers take precautions to minimize the risk of bleeding and have strategies in place to address it if it occurs.
Pain at the implantation site is another short-term complication that some individuals may experience. This discomfort is usually temporary and can be managed with pain medication prescribed by the healthcare provider. Additionally, lead migration or displacement is a potential complication that may occur. However, healthcare providers closely monitor patients after the procedure to detect and address any lead movement promptly.
It is important for individuals undergoing sacral nerve stimulation to be closely monitored by their healthcare providers. Regular follow-up appointments allow for early detection of any potential complications and ensure that appropriate medical care is provided. By closely monitoring patients, healthcare providers can address any issues that arise and provide necessary interventions to manage complications effectively.
Long-term Risks and Complications
While sacral nerve stimulation can provide long-term relief for many individuals, there are potential complications that may arise over time. One possible long-term complication is lead breakage. Although rare, lead breakage can occur due to various factors such as physical stress or device malfunction. Regular follow-up appointments with healthcare providers help monitor the integrity of the leads and detect any signs of breakage early on.
Battery-related issues are another long-term risk to consider. The implanted device relies on a battery to function properly, and over time, the battery may need to be replaced. Healthcare providers carefully monitor the battery life during follow-up appointments and can schedule battery replacement procedures as needed to ensure uninterrupted therapy.
Discomfort from the implanted device is another potential long-term complication. While most individuals adapt well to the presence of the device, some may experience discomfort or irritation. It is essential to communicate any discomfort to the healthcare provider, as adjustments can often be made to improve comfort levels.
In some cases, individuals may find that the symptom relief provided by sacral nerve stimulation becomes inadequate over time. This can be a challenging situation, but it is important to remember that healthcare providers have various treatment options available to address changing needs. Regular follow-up appointments allow healthcare providers to assess the effectiveness of the therapy and make necessary adjustments to optimize symptom relief.
If you experience any concerning symptoms or changes after undergoing sacral nerve stimulation, it is crucial to consult with your healthcare provider without delay. Prompt evaluation and guidance from your healthcare provider can help ensure that any complications are addressed promptly and effectively.
The Effectiveness of Sacral Nerve Stimulation
Measuring the Success of Sacral Nerve Stimulation
Determining the success of sacral nerve stimulation varies depending on the individual’s symptoms and their desired outcomes. Success can be evaluated through objective measures, such as improvement in urinary or bowel control, reduced frequency and urgency, or decreased pain levels. Additionally, subjective factors, including quality of life and satisfaction with the treatment, are essential measures of success.
It’s crucial to have realistic expectations and recognize that sacral nerve stimulation may not provide complete resolution of all symptoms in every individual. However, it has shown significant benefits for many, leading to a considerable improvement in their well-being.
Factors Affecting the Effectiveness of Stimulation
The effectiveness of sacral nerve stimulation can be influenced by various factors, including the individual’s responsiveness to stimulation, the underlying medical condition, and the accuracy of lead placement. It’s important to work closely with the healthcare provider to optimize the stimulation settings and address any concerns or issues that arise.
Frequently Asked Questions about Sacral Nerve Stimulation
Preparing for Sacral Nerve Stimulation
Before undergoing sacral nerve stimulation, discuss any concerns or questions you may have with your healthcare provider. They can provide you with specific instructions on how to prepare for the procedure, including fasting requirements, medication management, and post-operative care.
It’s essential to have a thorough understanding of the procedure, its potential benefits, and risks. If you have any doubts or uncertainties, do not hesitate to seek clarification from your healthcare provider. They are your best resource for accurate information tailored to your individual needs.
Living with Sacral Nerve Stimulation
Sacral nerve stimulation can significantly impact an individual’s quality of life. However, it’s important to remember that this treatment may require ongoing management and adjustments from your healthcare provider. Regular follow-up appointments are essential to monitor the device’s performance, address any concerns, and ensure optimal treatment outcomes.
If you experience any changes in symptoms, discomfort, or concerns regarding the neurostimulator, don’t hesitate to reach out to your healthcare provider. They are there to support you and provide the necessary guidance throughout your sacral nerve stimulation journey.
In conclusion, sacral nerve stimulation is a valuable treatment option for various conditions affecting the sacral nerves. By working closely with healthcare professionals, individuals can determine the need for stimulation, undergo the proper evaluation and preparation, and enjoy the potential benefits that sacral nerve stimulation may provide. Remember, always consult with a trusted healthcare provider for personalized advice tailored to your specific circumstances.