How High Sacral Nerve Stimulation is Needed for Bladder Control
Bladder control is an essential bodily function that many of us take for granted. However, for individuals who struggle with urinary incontinence or overactive bladder, this basic function can be challenging to manage. Thankfully, medical advancements such as Sacral Nerve Stimulation (SNS) have provided effective treatment options for those seeking relief. In this article, we will delve into the intricacies of SNS and explore how the level of stimulation plays a crucial role in achieving optimal bladder control.
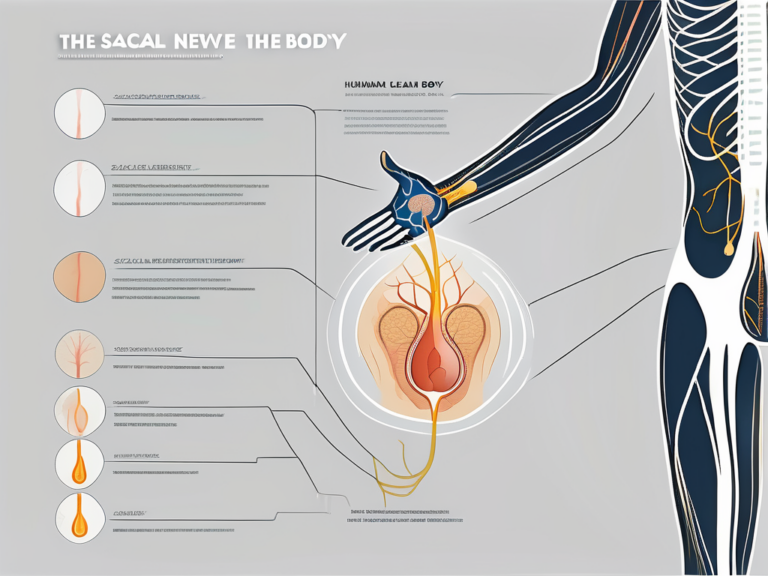
Understanding Sacral Nerve Stimulation
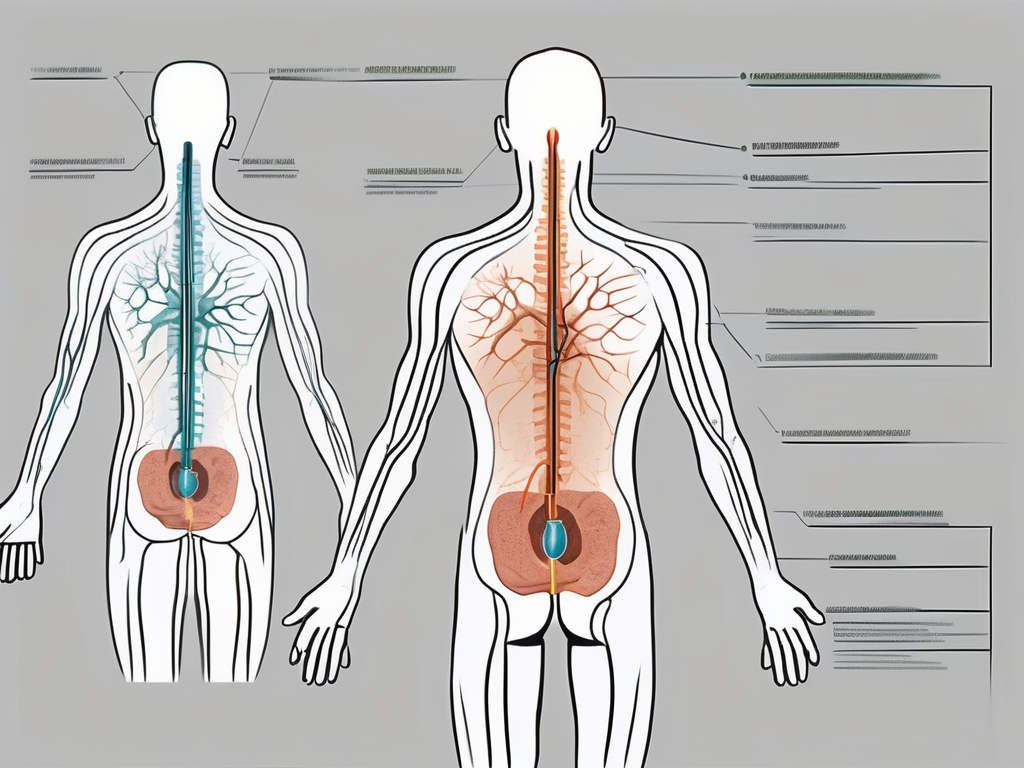
Sacral Nerve Stimulation is a medical procedure that involves the implantation of a small device, similar to a pacemaker, under the skin in the buttock area. This device sends electrical impulses to the sacral nerves, which are responsible for controlling the bladder and associated muscles. By modulating the signals sent to these nerves, SNS can help restore normal bladder function and alleviate symptoms such as frequent urination, urgency, and leakage.
The Role of Sacral Nerves in Bladder Control
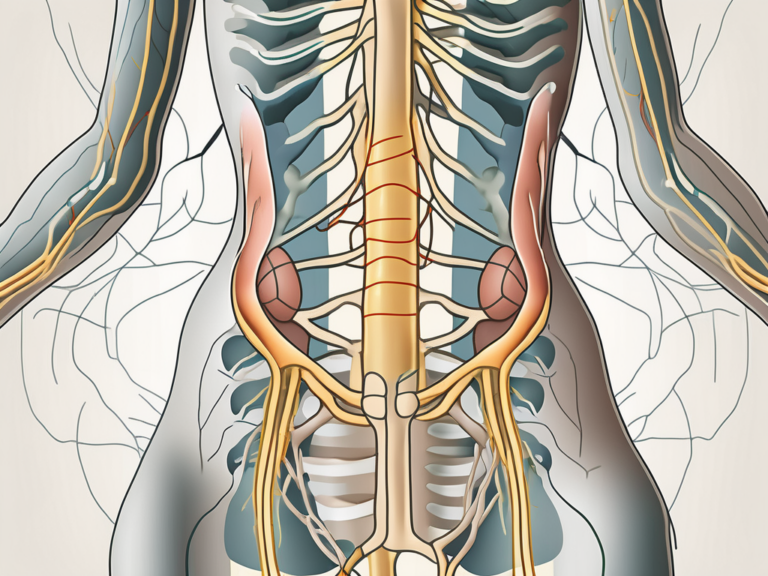
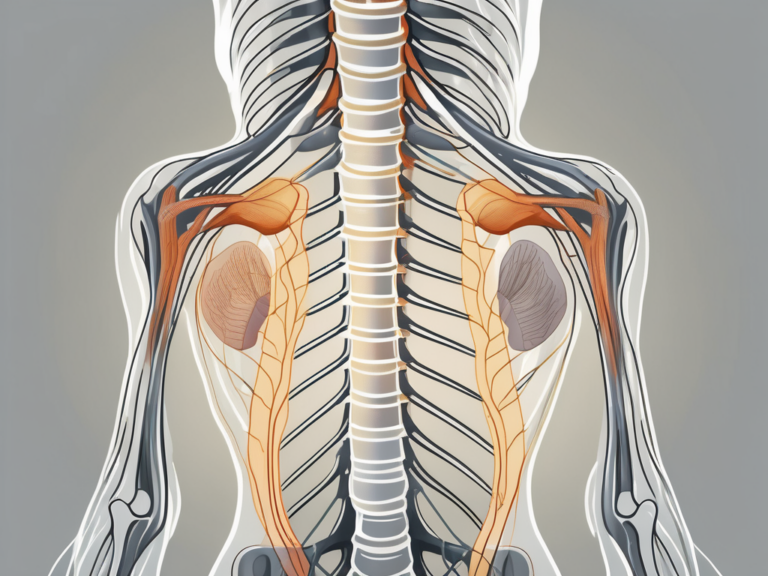
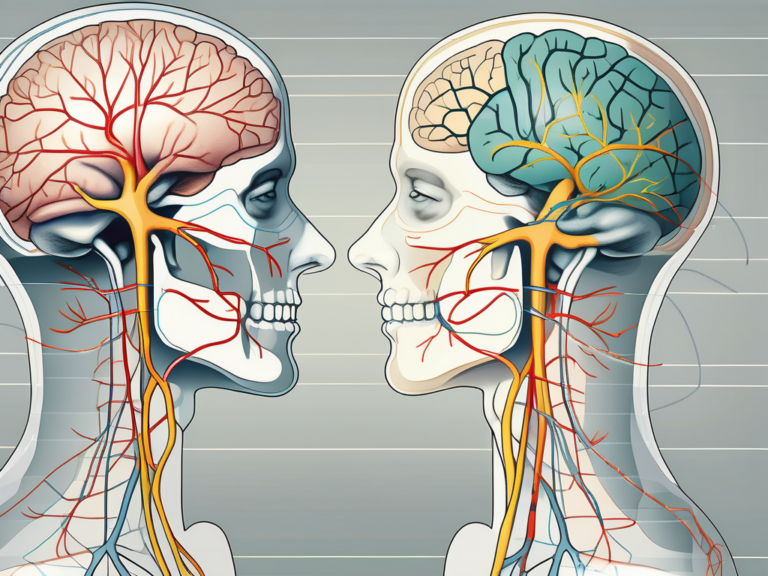
Before delving further into SNS, it is important to understand the role of sacral nerves in bladder control. These nerves act as a communication pathway between the brain and the bladder muscles. They transmit signals that coordinate the relaxation and contraction of the bladder muscles, allowing for proper storage and voiding of urine. Any disruption in this complex communication system can result in urinary dysfunction.
The sacral nerves, also known as the S2 to S4 nerve roots, play a crucial role in maintaining the intricate balance between the sympathetic and parasympathetic nervous systems. The sympathetic nervous system is responsible for the fight-or-flight response, while the parasympathetic nervous system promotes rest and digestion. In the case of bladder control, the parasympathetic system dominates, ensuring that the bladder remains relaxed during storage and contracts when it is time to void.
However, various factors such as trauma, surgery, or neurological conditions can disrupt this delicate balance. When the sacral nerves are not functioning optimally, the coordination between the brain and the bladder muscles is compromised, leading to urinary dysfunction. This can manifest as overactive bladder, urinary incontinence, or even urinary retention.
The Science Behind Sacral Nerve Stimulation
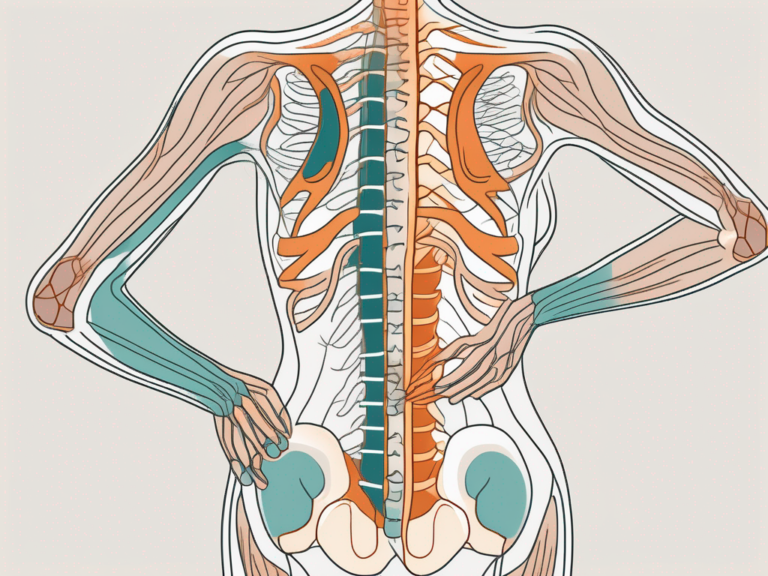
Sacral Nerve Stimulation works by stimulating the sacral nerves through gentle electrical impulses. These impulses modulate the neural signals, effectively retraining the bladder and surrounding muscles to function properly. By adjusting the level of stimulation, healthcare professionals can fine-tune the intervention to suit each patient’s specific needs.
The electrical impulses generated by the SNS device mimic the natural signals sent by the brain to the sacral nerves. This stimulation helps restore the communication pathway between the brain and the bladder muscles, allowing for better coordination and control. It also helps to suppress the overactive signals that may be causing urinary urgency and frequency.
This personalized approach to SNS ensures that the treatment aligns with the patient’s unique anatomy and physiological requirements. It often begins with a trial period, during which a temporary electrode is placed near the sacral nerves. This trial period allows both the patient and the healthcare team to assess the effectiveness of the treatment and determine the optimal level of stimulation.
During the trial period, patients may experience improvements in their urinary symptoms, such as reduced urgency, decreased frequency, and better control over leakage. This positive response to the temporary electrode placement provides valuable insights into the potential long-term benefits of SNS.
Once the trial period is deemed successful, the temporary electrode is replaced with a permanent implant. The permanent SNS device is typically placed under the skin in the buttock area, with the leads connected to the sacral nerves. This implantation procedure is usually performed under local anesthesia, and patients can often go home the same day.
After the implantation, patients may need to make adjustments to the stimulation level to achieve optimal results. This can be done using an external programmer, which allows patients to control the stimulation parameters within a range determined by their healthcare provider. Regular follow-up appointments are scheduled to monitor progress and make any necessary adjustments.
It is important to note that while SNS can be highly effective in managing urinary dysfunction, it may not be suitable for everyone. Healthcare professionals will carefully evaluate each patient’s medical history, symptoms, and overall health to determine if SNS is the right treatment option.
In conclusion, Sacral Nerve Stimulation is a medical procedure that offers hope for individuals suffering from urinary dysfunction. By targeting the sacral nerves and modulating their signals, SNS can help restore normal bladder function and improve quality of life. With careful evaluation and personalized treatment plans, healthcare professionals can provide patients with an effective and tailored approach to managing their urinary symptoms.
The Process of Sacral Nerve Stimulation
While the idea of an implantable device may seem intimidating, the process of Sacral Nerve Stimulation is relatively straightforward and minimally invasive. However, it is essential to consult with a qualified healthcare professional to determine candidacy and discuss any potential risks or complications.
Preparing for Sacral Nerve Stimulation
Prior to the procedure, healthcare providers will conduct a thorough evaluation to ensure that SNS is the most appropriate course of action. This evaluation may involve medical history reviews, physical examinations, and diagnostic tests to rule out other possible causes of urinary dysfunction.
During the evaluation, the healthcare team will take the time to explain the procedure in detail, addressing any concerns or questions the patient may have. They will also discuss the potential benefits and risks of Sacral Nerve Stimulation, allowing the patient to make an informed decision about their treatment options.
Additionally, patients may need to adjust their medication regimen or discontinue certain medications before the procedure. This is because certain medications may interfere with the effectiveness or safety of SNS. It is crucial to communicate openly with the healthcare team to ensure optimal preparation and reduce the risk of complications.
What to Expect During the Procedure
The actual procedure for Sacral Nerve Stimulation involves two main steps: the placement of the temporary electrode and the subsequent implantation of the permanent device. Both procedures are performed under local anesthesia, ensuring maximum comfort for the patient.
Before the procedure begins, the patient will be positioned comfortably on an operating table. The healthcare team will ensure that the patient is relaxed and at ease before proceeding.
During the trial phase, a temporary electrode is placed near the sacral nerves via a small needle. This electrode is connected to an external stimulator, allowing patients to assess the potential improvement in their bladder symptoms. The healthcare team will carefully monitor the patient’s response to the stimulation, making adjustments as needed to optimize the results.
The trial period typically lasts for a few days to a few weeks, during which the patient will keep a detailed record of their bladder symptoms and any changes they experience. This information will be invaluable in determining the effectiveness of Sacral Nerve Stimulation and guiding further treatment decisions.
If the trial is successful, the permanent device is implanted during a separate procedure. The permanent implantation is similar to the trial phase but involves the placement of the device under the skin in the buttock area. The healthcare team will take great care to ensure that the device is positioned correctly and securely, minimizing the risk of displacement or discomfort.
Once the permanent device is implanted, the healthcare team will program it to deliver the electrical impulses at the personalized level determined during the trial phase. This programming is tailored to the specific needs and preferences of each patient, ensuring optimal symptom management and quality of life.
After the procedure, the patient will receive detailed instructions on post-operative care and follow-up appointments. The healthcare team will closely monitor the patient’s progress, making any necessary adjustments to the device settings to ensure continued effectiveness.
It is important to note that Sacral Nerve Stimulation is not a cure for urinary dysfunction, but rather a management tool that can significantly improve symptoms and quality of life. Regular follow-up appointments and open communication with the healthcare team are essential for long-term success and optimal outcomes.
Determining the Level of Stimulation Required
One of the significant advantages of Sacral Nerve Stimulation is the ability to customize the level of stimulation for each patient. The optimal level of stimulation required varies from person to person and is influenced by various factors, including individual anatomy and the severity of bladder dysfunction. Healthcare providers carefully adjust the stimulation levels to ensure efficacy while minimizing potential side effects.
When determining the level of stimulation required for sacral nerve stimulation, healthcare providers take into account several factors. These factors play a crucial role in tailoring the treatment to meet the specific needs of each patient. One such factor is the patient’s sensitivity to electrical stimulation. Some individuals may be more sensitive to electrical impulses, requiring lower levels of stimulation for effective symptom control. On the other hand, patients with a higher tolerance for stimulation may require higher levels to achieve the desired results.
The severity of the patient’s symptoms also influences the level of stimulation needed. Patients with more severe bladder dysfunction may require stronger stimulation to effectively manage their symptoms. Conversely, those with milder symptoms may find that lower levels of stimulation are sufficient for symptom control.
Another important consideration is the patient’s overall health. Certain medical conditions or medications may affect the body’s response to electrical stimulation. Healthcare providers take these factors into account when determining the appropriate level of stimulation for each patient, ensuring that it is safe and effective.
Factors Influencing the Level of Stimulation
Several factors contribute to the determination of the level of sacral nerve stimulation required. These factors include the patient’s sensitivity to electrical stimulation, the severity of their symptoms, and their overall health. Additionally, healthcare providers consider the patient’s individual comfort level and responses to different stimulation settings.
Individual comfort level is an essential factor in determining the level of stimulation required. Some patients may find higher levels of stimulation uncomfortable or even painful, while others may tolerate it well. Healthcare providers work closely with patients to find the balance between effective symptom control and patient comfort.
Furthermore, patients’ responses to different stimulation settings are carefully evaluated. Healthcare providers may test various levels of stimulation during the trial phase to determine which settings provide the best symptom control. This trial and error process helps identify the optimal level of stimulation for each patient.
Adjusting Stimulation Levels for Optimal Control
Once the permanent device is implanted, patients have the ability to adjust their stimulation levels within a predetermined range. This feature helps patients respond to changes in bladder function and allows for continued optimization of symptom control. The ability to fine-tune stimulation levels ensures that patients can achieve the best possible outcomes for their specific needs.
Patients are often provided with a handheld device that allows them to adjust the stimulation levels as needed. This empowers patients to take an active role in their treatment and provides them with a sense of control over their symptoms. Regular follow-up appointments with healthcare providers are essential to monitor the effectiveness of the chosen stimulation levels and make any necessary adjustments.
It is important to note that finding the optimal level of stimulation may require some trial and error. Patients may need to experiment with different settings to determine what works best for them. Open communication with healthcare providers is crucial during this process to ensure that patients receive the support and guidance they need to achieve optimal symptom control.
Potential Risks and Complications of Sacral Nerve Stimulation
As with any medical procedure, Sacral Nerve Stimulation carries potential risks and complications. However, the overall incidence of serious complications is relatively low. It is important to discuss these risks with a healthcare professional before proceeding with the procedure.
Sacral Nerve Stimulation is a minimally invasive procedure that involves the implantation of a small device to stimulate the sacral nerves, which are responsible for controlling the bladder, bowel, and pelvic floor muscles. While the procedure has proven to be effective in managing various conditions, it is essential to understand the potential risks and complications that may arise.
Short-term Risks and Side Effects
Following the implantation of the temporary electrode or the permanent device, patients may experience some discomfort or pain at the implantation site. This is typically mild and resolves within a few days. The healthcare team will provide appropriate pain management strategies to alleviate any discomfort.
In addition to temporary pain, patients may also experience other short-term risks such as infection, bleeding, or bruising at the surgical site. These risks are relatively rare but should be promptly reported to the healthcare team for proper evaluation and treatment.
It is crucial for patients to closely monitor their symptoms and report any concerning changes to their healthcare provider. By doing so, potential complications can be identified and managed early, ensuring the best possible outcome.
Long-term Complications and How to Manage Them
In rare cases, long-term complications may arise from Sacral Nerve Stimulation. These complications include device-related issues, such as migration, erosion, or malfunctions. While the incidence of these complications is low, it is important for patients to be aware of them and know how to manage them effectively.
Regular follow-up appointments with the healthcare provider are crucial to monitor the functionality of the implanted device and identify any potential complications early on. During these appointments, the healthcare team will assess the device’s performance, address any concerns, and provide necessary adjustments or interventions.
Prompt reporting of any changes in symptoms or device-related concerns is essential. Patients should not hesitate to contact their healthcare provider if they experience unusual sensations, pain, or any other issues related to the implanted device. By doing so, appropriate measures can be taken to manage and resolve these complications effectively.
It is important to note that while Sacral Nerve Stimulation carries potential risks and complications, the benefits of the procedure often outweigh the risks for patients suffering from conditions such as overactive bladder, urinary retention, or fecal incontinence. By working closely with their healthcare team, patients can make informed decisions and receive the necessary support throughout their treatment journey.
The Impact of Sacral Nerve Stimulation on Quality of Life
For individuals struggling with urinary incontinence or overactive bladder, the impact of Sacral Nerve Stimulation goes beyond symptom management. The improvements in bladder control achieved through SNS can significantly enhance one’s quality of life.
Improvements in Bladder Control and Daily Life
By restoring proper bladder function, Sacral Nerve Stimulation can reduce or eliminate symptoms such as urgency, frequency, and leakage. This improvement allows individuals to regain control over their bladder, engage in daily activities without interruption, and confidently participate in social interactions. The reduction in bladder-related stress and anxiety contributes to overall well-being and a better quality of life.
Patient Satisfaction and Success Rates
Research has shown that Sacral Nerve Stimulation is generally well-tolerated and yields positive outcomes for patients. Studies have reported significant improvements in symptom control, quality of life, and patient satisfaction rates. However, individual experiences may vary, and it is essential for patients to have realistic expectations and engage in thorough discussions with their healthcare providers.
Future Directions in Sacral Nerve Stimulation
The field of Sacral Nerve Stimulation continues to evolve, with ongoing research and technological advancements paving the way for further improvements in treatment outcomes.
Technological Advances and Their Potential Impact
Advancements in technology have led to the development of more sophisticated devices and programming options for Sacral Nerve Stimulation. These innovations have the potential to refine the treatment process, enhance patient comfort, and improve long-term outcomes. Continued research and collaboration in this field promise to bring further advancements and options to individuals seeking relief from bladder dysfunction.
Ongoing Research and What It Means for Patients
Clinical research studies are actively investigating various aspects of Sacral Nerve Stimulation, including its long-term efficacy, patient selection criteria, and potential applications in different patient populations. This ongoing research aims to expand our understanding of SNS and provide further evidence-based guidelines for its use. Patients considering SNS can benefit from staying informed about these advancements and discussing potential treatment options with their healthcare providers.
In conclusion, Sacral Nerve Stimulation offers a valuable treatment option for individuals struggling with bladder control issues. The level of stimulation required plays a crucial role in achieving optimal outcomes. By understanding the science behind SNS, navigating the treatment process, and staying informed about future directions, patients can make informed decisions and work with their healthcare providers to regain control over their bladder function and improve their quality of life.