Does It Matter Which Side You Get the Sacral Nerve Stimulator Implanted On?
Sacral nerve stimulation is a medical procedure that can provide relief for individuals suffering from certain conditions, such as urinary and bowel dysfunction. However, one important question that often arises is whether it matters which side of the body the sacral nerve stimulator is implanted on. In this article, we will delve into the significance of the implantation side and explore the factors that influence this decision.
Understanding Sacral Nerve Stimulation
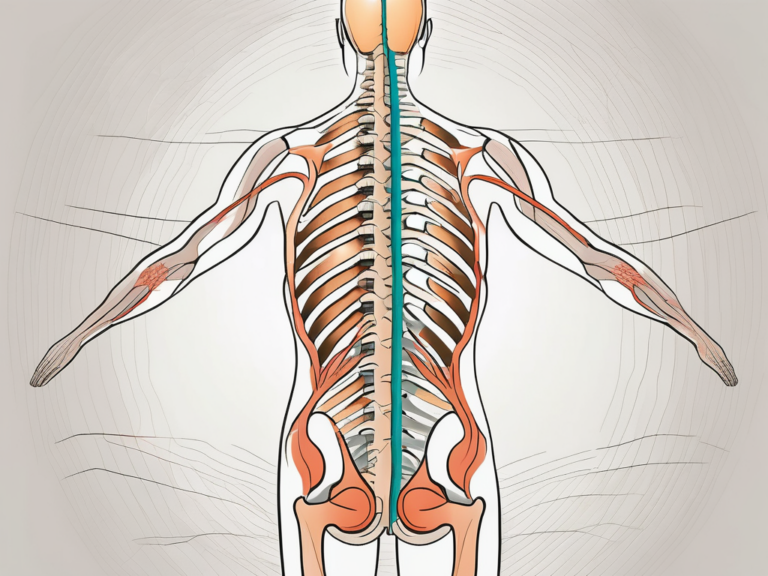
Sacral nerve stimulation involves the placement of a small device, known as a sacral nerve stimulator, which delivers electrical impulses to the sacral nerves. These nerves play an integral role in the proper functioning of the bladder, bowel, and pelvic floor muscles. By stimulating these nerves, the device can help alleviate symptoms associated with urinary and bowel dysfunction.
The Role of Sacral Nerve in Body Function
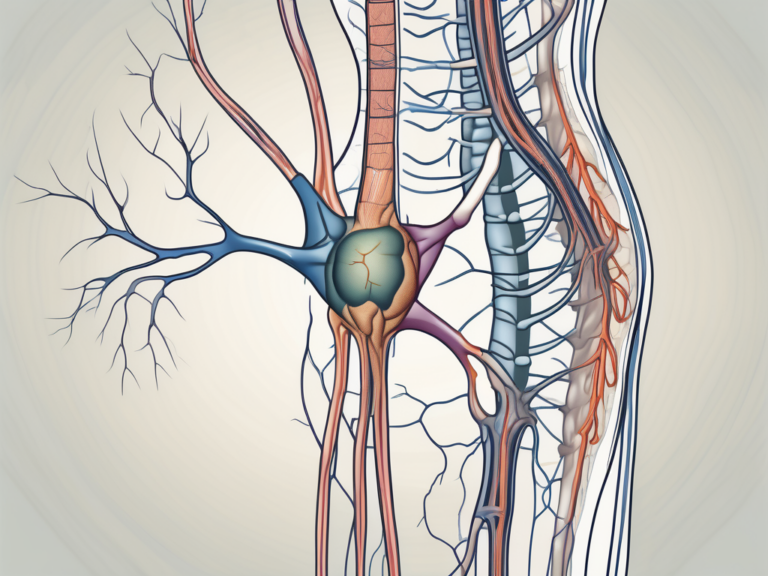
The sacral nerves are responsible for transmitting signals between the brain and the bladder, bowel, and pelvic floor muscles. When these nerves malfunction, it can lead to issues such as urinary incontinence, urgency, frequency, as well as fecal incontinence. Sacral nerve stimulation aims to restore normal nerve function and improve these symptoms.
The sacral nerves, also known as the S2-S4 nerves, are a crucial part of the autonomic nervous system. These nerves are responsible for controlling the involuntary functions of the bladder, bowel, and pelvic floor muscles. They play a vital role in maintaining continence and proper functioning of these organs.
When the sacral nerves are functioning properly, they receive signals from the brain, instructing the bladder and bowel muscles to contract or relax at the appropriate times. This coordination ensures that urine and feces are stored until it is convenient to empty them. However, when there is a malfunction in these nerves, the signals may become disrupted, leading to various urinary and bowel dysfunctions.
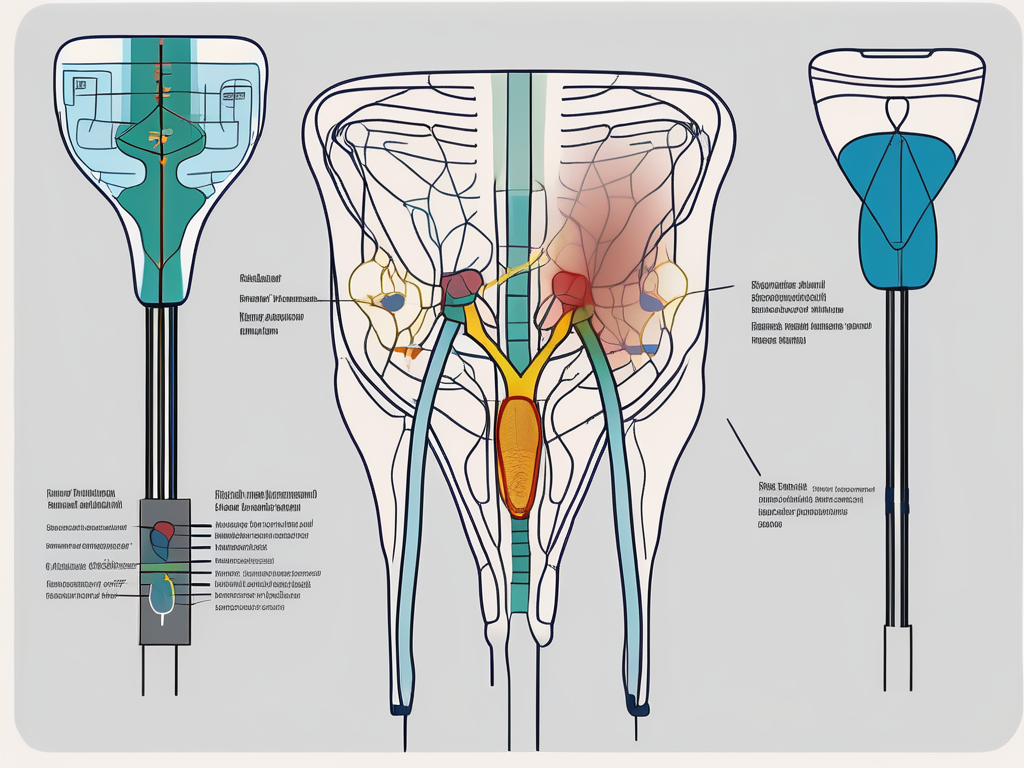
The Basics of Sacral Nerve Stimulation Procedure
The sacral nerve stimulation procedure involves the surgical placement of a small device under the skin, usually in the upper buttock area. This device is connected to a lead that is placed near the sacral nerves. Once the device is implanted, it can be programmed to deliver electrical impulses that modulate the nerve activity and improve bladder and bowel function.
The surgical procedure for sacral nerve stimulation is typically performed under general anesthesia. The surgeon makes a small incision in the upper buttock area and creates a pocket under the skin to accommodate the device. The lead, a thin wire with electrodes, is then carefully guided to the sacral nerves using fluoroscopy or other imaging techniques.
Once the lead is in place, the surgeon connects it to the device, which is also implanted under the skin. The device is about the size of a stopwatch and contains a battery and a microchip. The battery provides the power needed to deliver the electrical impulses, while the microchip controls the timing and intensity of the stimulation.
After the surgery, the patient undergoes a programming session to customize the stimulation settings according to their specific needs. The device can be adjusted to deliver different patterns of electrical impulses, depending on the symptoms and response to treatment. Regular follow-up appointments are scheduled to monitor the progress and make any necessary adjustments to optimize the therapy.
Sacral nerve stimulation is considered a reversible treatment option, meaning that the device can be removed if necessary. However, many patients experience significant improvement in their symptoms and choose to keep the device long-term.
The Importance of Implantation Side
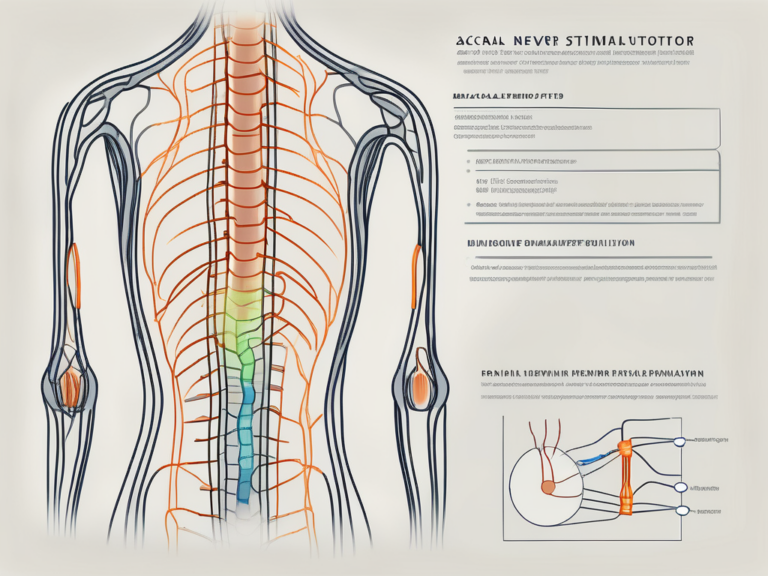
While the effectiveness of sacral nerve stimulation in alleviating symptoms is well-documented, the impact of implantation side has been a topic of debate. Some believe that the choice of side can influence the efficacy of the treatment, while others argue that there is no significant difference.
Anatomy and the Implantation Side
The decision regarding the implantation side is primarily influenced by the anatomy of the patient. The surgeon carefully considers factors such as the location of the sacral nerves, the patient’s body structure, and any previous surgical procedures in the pelvic area. This helps ensure that the device is optimally positioned to stimulate the sacral nerves effectively.
When determining the implantation side, the surgeon takes into account the individual variations in anatomy. The sacral nerves, responsible for transmitting signals between the spinal cord and the pelvic organs, can have slight differences in their course and distribution from person to person. By carefully studying the patient’s anatomy, the surgeon can identify the side that provides the most direct access to the sacral nerves, maximizing the potential for successful stimulation.
Additionally, the patient’s body structure plays a crucial role in the decision-making process. Factors such as the thickness of the subcutaneous tissue and the presence of any underlying structures that may obstruct the electrode placement are carefully evaluated. This ensures that the implantation side is selected in a way that minimizes any potential complications and optimizes the overall outcome of the procedure.
Previous surgical procedures in the pelvic area can also impact the choice of implantation side. Scar tissue or altered anatomical landmarks resulting from prior surgeries may influence the surgeon’s decision, as they need to navigate around these structures to reach the sacral nerves. By taking these factors into consideration, the surgeon can plan the implantation side that offers the best chance of successful stimulation and symptom relief.
Potential Impact on Stimulation Effectiveness
Another point of consideration is whether the stimulation will be more effective when the device is implanted on one side versus the other. While research in this area is limited, some studies suggest that there may be a slight variation in stimulation effectiveness between the two sides. Factors such as the proximity of the electrode to the target nerves and the individual response of the patient’s nervous system may contribute to this variation.
One study conducted on a small group of patients found that stimulation on one side led to better symptom improvement compared to the other side. However, it is important to note that this study had limitations in terms of sample size and generalizability. Further research is needed to establish a clear understanding of the potential impact of implantation side on stimulation effectiveness.
Despite the limited evidence, some surgeons may prefer to implant the device on a specific side based on their clinical experience and observations. They may have noticed a trend of better outcomes when the device is placed on a particular side in their patient population. However, these observations should be interpreted with caution and validated through rigorous scientific studies.
In conclusion, while the choice of implantation side in sacral nerve stimulation remains a topic of debate, it is clear that the decision is influenced by the patient’s anatomy, body structure, and previous surgical history. The potential impact of implantation side on stimulation effectiveness requires further investigation to establish a definitive understanding. Surgeons must carefully evaluate each patient’s unique circumstances to make an informed decision that maximizes the chances of successful treatment outcomes.
Factors Influencing the Choice of Implantation Side
When determining the implantation side for a sacral nerve stimulator, several factors come into play. These include the patient’s physical condition and history, as well as the surgeon’s preference and expertise.
Patient’s Physical Condition and History
The patient’s individual circumstances play a crucial role in deciding the implantation side. Factors such as previous surgeries, injury, or anatomical abnormalities may impact the choice. For instance, if a patient has undergone a previous surgery on one side of the sacrum, the surgeon may opt for the opposite side to avoid potential complications or interference with the previous surgical site.
Furthermore, anatomical abnormalities, such as scoliosis or spinal deformities, may affect the alignment of the sacrum. In such cases, the surgeon will carefully evaluate the patient’s condition to determine the most suitable implantation side that ensures optimal placement and functionality of the sacral nerve stimulator.
Additionally, the patient’s overall health and any specific conditions they may have will also affect the decision-making process. For example, if a patient has a history of chronic pain on one side of the body, the surgeon may consider implanting the device on the same side to target the affected nerves directly.
It is essential for the patient to have a thorough discussion with their healthcare provider to ensure all aspects are considered. The healthcare provider will review the patient’s medical history, conduct a comprehensive physical examination, and may even order additional diagnostic tests to gather all the necessary information for making an informed decision.
Surgeon’s Preference and Expertise
Surgeons who specialize in sacral nerve stimulation may have their own preferences when it comes to the implantation side. They often rely on their expertise and experience to determine the best approach. Some surgeons may have a higher success rate or better outcomes when implanting the device on a particular side, based on their familiarity with the anatomy or their preferred surgical technique.
It is important for patients to engage in open communication with their surgeon to address any concerns they may have and understand their surgeon’s rationale behind the choice of implantation side. The surgeon will take into account the patient’s preferences, if any, and provide a detailed explanation of their decision-making process. This open dialogue helps build trust and ensures that the patient feels comfortable and confident in the chosen implantation side.
In conclusion, the choice of implantation side for a sacral nerve stimulator is influenced by various factors, including the patient’s physical condition and history, as well as the surgeon’s preference and expertise. By considering all these factors, healthcare providers and surgeons can make an informed decision that maximizes the potential benefits of sacral nerve stimulation for each individual patient.
Potential Risks and Complications
As with any surgical procedure, there are potential risks and complications associated with sacral nerve stimulation. However, these risks are generally low, and most patients experience successful outcomes. It is crucial for patients to be aware of these risks and have open communication with their healthcare provider throughout the process.
Sacral nerve stimulation is a minimally invasive procedure that involves the implantation of a small device, similar to a pacemaker, to modulate the sacral nerves. This treatment option is commonly used for conditions such as overactive bladder, urinary incontinence, and fecal incontinence. While the procedure has proven to be effective for many patients, it is important to understand the potential risks involved.
Risks Associated with Wrong Side Implantation
One potential risk associated with choosing the wrong implantation side is suboptimal stimulation. If the device is not optimally positioned, the electrical impulses may not effectively modulate the sacral nerves, resulting in reduced symptom improvement. However, it is important to note that the likelihood of experiencing this issue is relatively low.
During the preoperative planning phase, the healthcare team carefully evaluates the patient’s anatomy and determines the optimal implantation site. This involves conducting various tests and assessments to ensure accurate placement of the device. By following these protocols, the risk of wrong side implantation can be significantly minimized.
In rare cases, there may be complications related to the surgical procedure itself. These can include infection, bleeding, or damage to surrounding structures. However, with proper surgical technique and adherence to sterile protocols, the risk of these complications is extremely low.
How to Mitigate Potential Complications
To minimize the risks associated with sacral nerve stimulation, it is crucial to follow all post-operative care instructions provided by the healthcare team. This includes keeping the incision site clean, avoiding strenuous activities during the initial healing phase, and attending all follow-up appointments.
During the recovery period, patients may experience mild discomfort or swelling at the implantation site. This is normal and can be managed with over-the-counter pain medications and ice packs. It is important to avoid scratching or rubbing the area to prevent infection or damage to the device.
Additionally, patients should maintain open communication with their healthcare provider and seek immediate medical attention if they notice any concerning symptoms or changes in their condition. This can include increased pain, redness, or drainage at the incision site, persistent fever, or worsening of the initial symptoms.
Regular follow-up appointments are essential to monitor the progress of the treatment and make any necessary adjustments to the device settings. The healthcare team will work closely with the patient to ensure optimal outcomes and address any concerns or questions that may arise.
In conclusion, while there are potential risks and complications associated with sacral nerve stimulation, the overall success rate of this procedure is high. By following the recommended guidelines and maintaining open communication with the healthcare team, patients can minimize these risks and achieve improved quality of life.
Post-Implantation Care and Expectations
After the sacral nerve stimulator is implanted, patients can expect a recovery process that may take several weeks. During this time, it is important to follow all post-operative care instructions provided by the healthcare team to ensure proper healing and optimal results.
When it comes to post-implantation care, there are several key factors to consider. Firstly, patients should keep the incision area clean and dry to prevent infection. This can be achieved by gently washing the area with mild soap and water, and then patting it dry with a clean towel. It is also important to avoid any activities that may cause excessive strain on the incision site, such as heavy lifting or rigorous exercise.
Additionally, patients may experience some discomfort and swelling in the incision area following the procedure. This is a normal part of the healing process and can be managed with pain medications prescribed by the healthcare team. It is crucial to take these medications as directed and report any severe or worsening pain to the healthcare provider.
Recovery Process and Timeline
The recovery process after sacral nerve stimulation implantation typically involves some discomfort and swelling in the incision area. Pain medications may be prescribed to manage any post-operative pain. Patients are generally advised to avoid activities that put strain on the incision site and to gradually resume their normal routine over time. The exact recovery timeline may vary depending on each patient’s individual circumstances.
During the recovery period, patients may experience a range of sensations, including tingling or mild electric shocks in the area where the sacral nerve stimulator is implanted. These sensations are a normal part of the treatment and should subside over time. However, if they persist or become increasingly uncomfortable, it is important to notify the healthcare provider for further evaluation.
It is also worth noting that the recovery process is not just physical, but also emotional. Adjusting to a new medical device and managing expectations can be challenging. Patients may experience a range of emotions, including excitement, anxiety, or frustration. It is important to seek support from loved ones and healthcare professionals to navigate these emotions and ensure a smooth recovery.
Long-term Management of Sacral Nerve Stimulator
After the initial recovery phase, patients can expect long-term management of their sacral nerve stimulator. This may involve regular follow-up appointments with their healthcare provider to assess the device’s performance and make any necessary adjustments. Patients should also be prepared to discuss the effectiveness of the treatment and address any ongoing concerns or questions.
During follow-up appointments, the healthcare provider may perform tests to evaluate the functioning of the sacral nerve stimulator and make any necessary programming changes. It is important for patients to communicate any changes in symptoms or concerns they may have during these appointments, as this information can help guide the healthcare provider in optimizing the device’s performance.
In addition to follow-up appointments, patients should also be aware of the importance of self-care and device maintenance. This may involve regularly checking the battery life of the sacral nerve stimulator and scheduling battery replacements when needed. It is also important to keep the device clean and dry, following the manufacturer’s instructions for proper care and maintenance.
Furthermore, patients should be aware of potential lifestyle adjustments that may be necessary with a sacral nerve stimulator. This can include avoiding certain activities or positions that may interfere with the device’s functioning or cause discomfort. It is important to have open and honest discussions with the healthcare provider about any lifestyle concerns or limitations to ensure the best possible outcomes.
Overall, the post-implantation care and expectations for sacral nerve stimulation involve a comprehensive approach to ensure proper healing, manage discomfort, and optimize the device’s performance. By following the healthcare team’s instructions, attending regular follow-up appointments, and practicing self-care, patients can maximize the benefits of this innovative treatment option.
Conclusion: Making an Informed Decision about Sacral Nerve Stimulator Implantation
Ultimately, the question of whether it matters which side you get the sacral nerve stimulator implanted on is a complex one. While some evidence suggests there may be a slight variation in stimulation effectiveness, the overall impact of the implantation side on treatment outcomes remains inconclusive. The decision should be made through careful consideration of the patient’s individual circumstances and in consultation with a qualified healthcare professional specializing in sacral nerve stimulation.
By having open and honest conversations with the healthcare team, patients can gain a clear understanding of the procedure, the potential risks and benefits, and the expected outcomes. This will enable them to make an informed decision and embark on a journey towards improved bladder and bowel function.