Does It Matter Which Side of the Sacrum You Get the Sacral Nerve Stimulator Implanted On?
The implementation of a sacral nerve stimulator is a significant decision for individuals seeking relief from chronic pelvic pain and urinary dysfunction. One question that often arises during the consultation process is whether it matters which side of the sacrum the implantation is performed on. This article aims to explore the various aspects related to this question and provide insights into the factors influencing the side of implantation, the potential impact on outcomes, and the overall patient experience.
Understanding the Sacral Nerve Stimulator
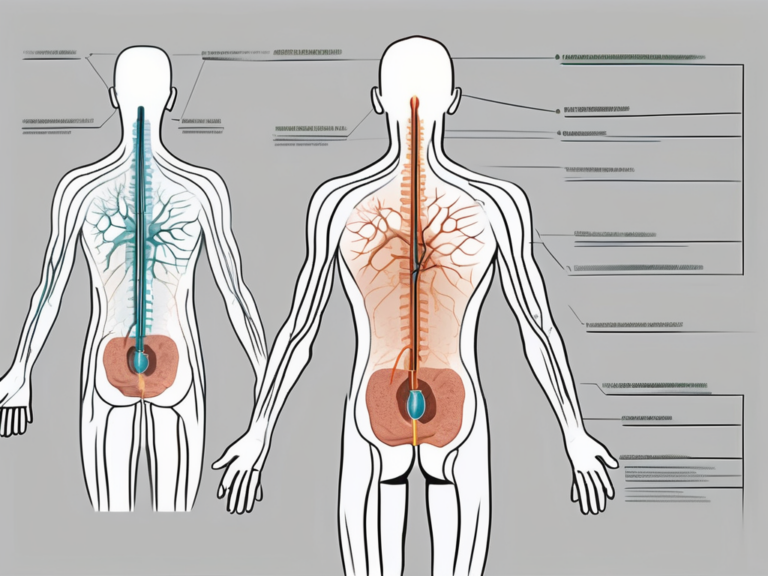
In order to comprehend the implications associated with the side of implantation, a basic understanding of the sacral nerve stimulator is necessary. The sacral nerve stimulator is a small device that is surgically implanted in the lower back to regulate the signals transmitted by the sacral nerves. By modulating these signals, the sacral nerve stimulator can alleviate chronic pelvic pain and improve bladder and bowel function.
The Role and Function of the Sacral Nerve
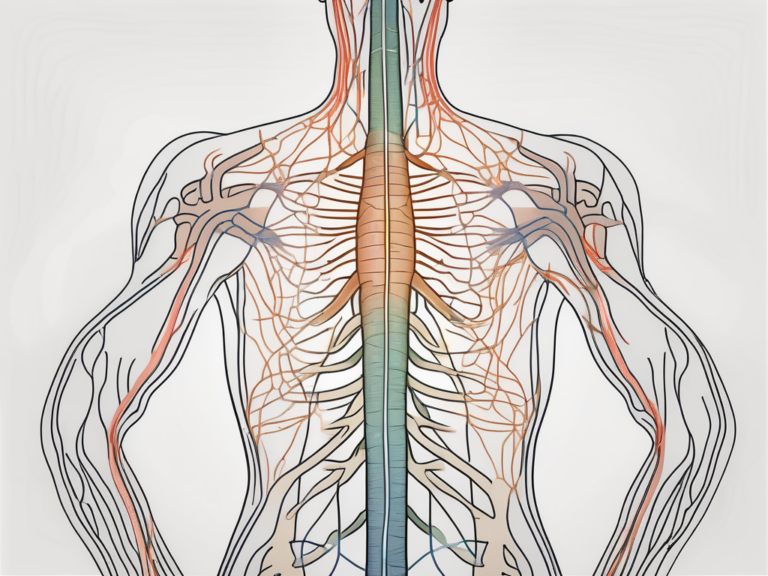
The sacral nerves play a crucial role in controlling the bladder, bowel, and pelvic floor muscles. They transmit signals between these organs and the brain, ensuring harmonious coordination of their functions. Any disruption or dysfunction in this neural pathway can lead to pelvic pain and urinary dysfunction.
When the sacral nerves are functioning properly, they send signals to the bladder, instructing it to store urine until it is convenient to empty. They also send signals to the bowel, coordinating the movement of stool through the intestines. Additionally, the sacral nerves play a role in controlling the pelvic floor muscles, which are responsible for maintaining continence and supporting the organs in the pelvic region.
However, when the sacral nerves are damaged or not functioning optimally, a variety of symptoms can occur. These may include urinary incontinence, frequent urination, difficulty emptying the bladder, constipation, and pelvic pain. These symptoms can significantly impact a person’s quality of life and may require intervention to alleviate the discomfort and restore normal function.
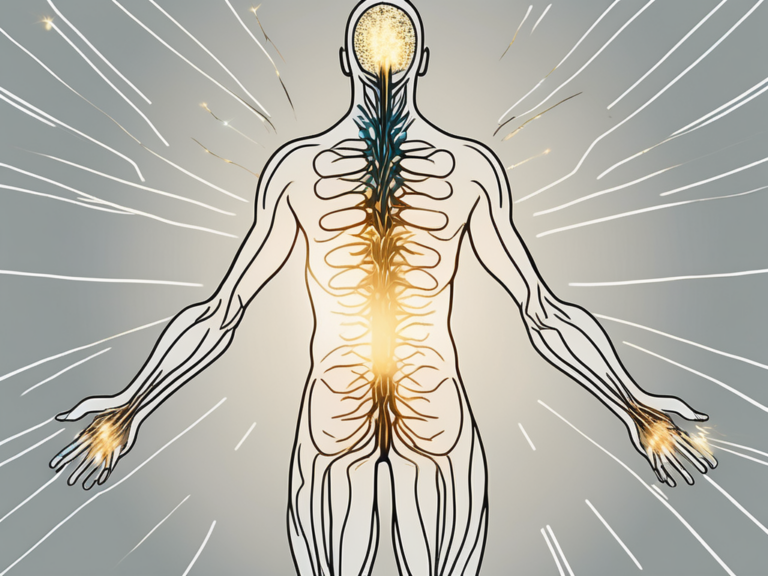
The Basics of Sacral Nerve Stimulation
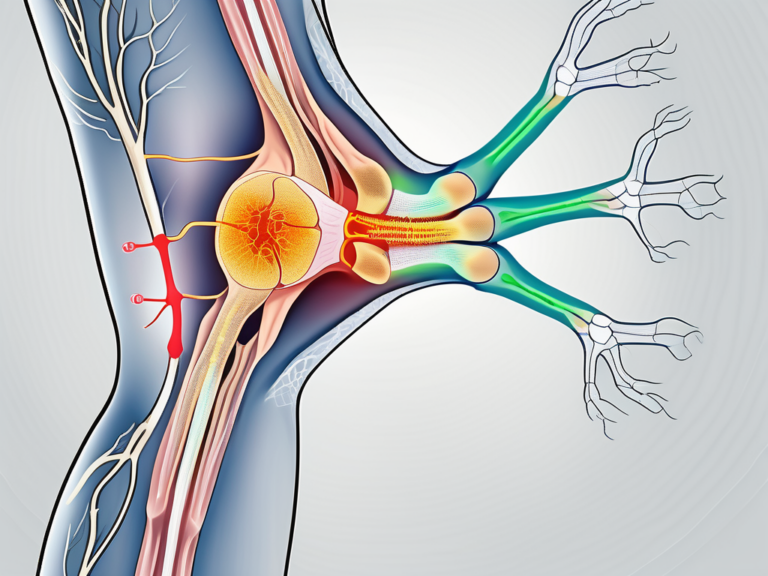
Sacral nerve stimulation involves the placement of a neurostimulator device beneath the skin, along with a lead or electrode that is positioned near the sacral nerves. The neurostimulator emits electrical impulses that modulate the sacral nerve activity, providing relief from symptoms such as pelvic pain, overactive bladder, and urinary incontinence.
The neurostimulator is programmed to deliver specific patterns of electrical impulses to the sacral nerves, depending on the individual’s symptoms and needs. These impulses can help regulate the signals sent by the sacral nerves, restoring normal function and alleviating pain and discomfort.
One of the advantages of sacral nerve stimulation is its adjustability. The settings of the neurostimulator can be modified to suit the patient’s changing needs, ensuring optimal symptom control. This flexibility allows for personalized treatment and can be particularly beneficial for individuals whose symptoms fluctuate over time.
The Procedure of Sacral Nerve Stimulator Implantation
The implantation procedure typically involves the insertion of the lead or electrode near the sacral nerves, followed by the placement of the neurostimulator device beneath the skin. The procedure is commonly performed under local anesthesia and usually takes around one to two hours to complete. After the surgery, patients are advised to refrain from vigorous physical activities for a certain period of time to promote healing and minimize discomfort.
Prior to the surgery, the patient will undergo a thorough evaluation to determine their suitability for sacral nerve stimulation. This evaluation may include various tests, such as urodynamic studies and imaging scans, to assess the underlying cause of the symptoms and ensure that sacral nerve stimulation is an appropriate treatment option.
During the implantation procedure, the surgeon will make a small incision in the lower back to access the sacral nerves. The lead or electrode will be carefully positioned near the nerves, ensuring optimal contact for effective stimulation. The neurostimulator device will then be placed beneath the skin, typically in the buttock or lower back area.
After the surgery, patients will be closely monitored to ensure proper healing and to adjust the neurostimulator settings as needed. Regular follow-up appointments will be scheduled to assess the effectiveness of the sacral nerve stimulation and make any necessary adjustments to optimize symptom control.
In conclusion, sacral nerve stimulation is a valuable treatment option for individuals suffering from chronic pelvic pain and urinary dysfunction. By modulating the signals transmitted by the sacral nerves, the sacral nerve stimulator can provide relief from symptoms and improve bladder and bowel function. The procedure of implanting the sacral nerve stimulator is relatively straightforward and offers adjustable settings to meet the individual’s specific needs. With proper evaluation, surgical skill, and post-operative care, sacral nerve stimulation can significantly enhance the quality of life for those affected by pelvic pain and urinary dysfunction.
The Sacrum and Its Sides: An Overview
To understand the potential impact of the side of implantation on the sacral nerve stimulator’s efficacy and patient experience, it is essential to delve into the anatomy and significance of the sacrum.
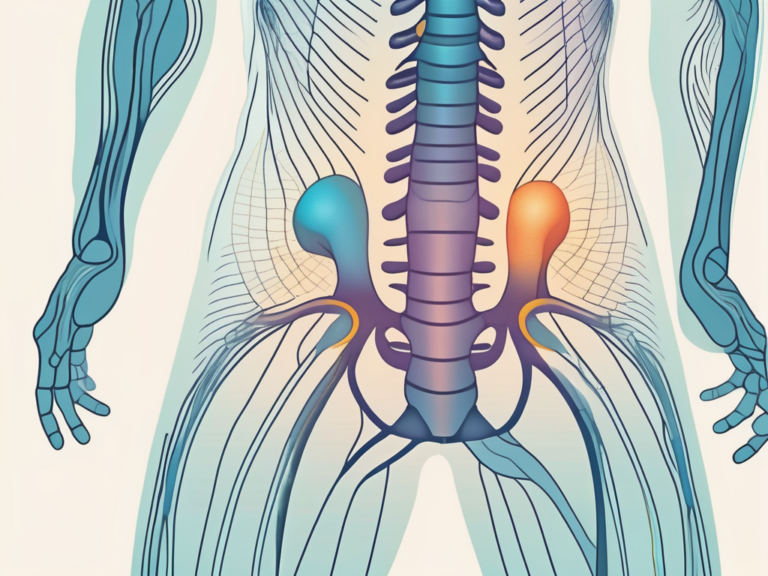
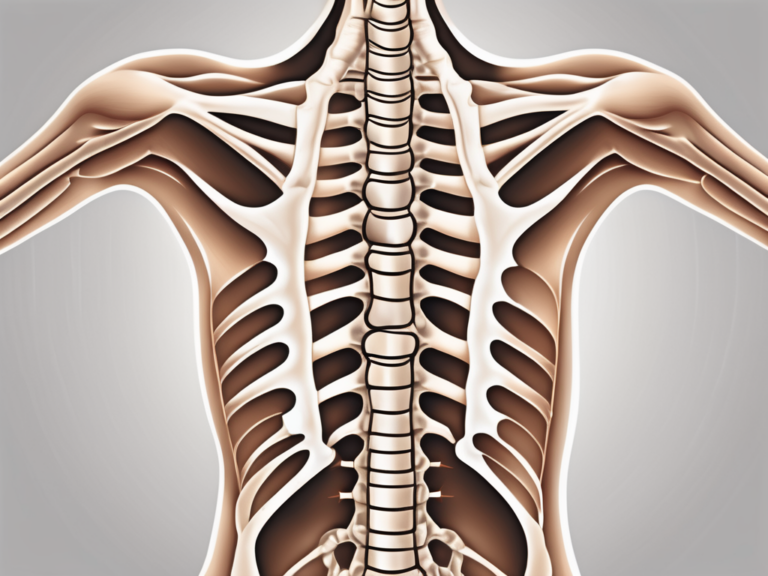
Anatomy of the Sacrum
The sacrum is a triangular-shaped bone located at the base of the spine, between the two hip bones. It consists of five fused vertebrae, forming a sturdy structure that provides support and stability to the pelvis. The sacrum also houses the sacral nerves, which emerge from small openings on its sides.
Let’s take a closer look at the intricate anatomy of the sacrum. The upper part of the sacrum, known as the base, connects to the last lumbar vertebra. It gradually tapers down to form the apex, which articulates with the coccyx, commonly known as the tailbone. The sacrum’s anterior surface is smooth and concave, while the posterior surface is rough and convex.
Within the sacrum, there are several important structures. The sacral canal runs through the center of the bone and contains the continuation of the spinal cord, known as the cauda equina. On either side of the sacral canal, there are four pairs of sacral foramina. These foramina provide passageways for the sacral nerves to exit the sacrum and supply various regions of the pelvis and lower extremities.
The Significance of the Sacrum’s Sides
Each side of the sacrum is associated with different sets of sacral nerves. The left side primarily gives rise to the S3 and S4 nerves, while the right side primarily gives rise to the S2 and S3 nerves. This anatomical distinction can potentially influence the positioning of the lead or electrode during sacral nerve stimulator implantation.
When considering the side of implantation for a sacral nerve stimulator, it is crucial to take into account the specific symptoms and conditions of the patient. For example, if a patient experiences urinary incontinence, targeting the S3 and S4 nerves on the left side may be more beneficial due to their involvement in controlling bladder function. On the other hand, if a patient suffers from chronic pelvic pain, focusing on the S2 and S3 nerves on the right side might be more appropriate.
Furthermore, the side of implantation can also affect the potential risks and complications associated with the procedure. The anatomy and vasculature surrounding the sacrum may vary slightly between the left and right sides, which could impact the ease of lead placement and the potential for nerve damage or bleeding.
It is important for healthcare professionals to carefully evaluate the patient’s individual circumstances and consider the implications of the sacrum’s sides when planning and performing sacral nerve stimulator implantation. By tailoring the procedure to the patient’s specific needs, optimal outcomes can be achieved, improving their quality of life and overall well-being.
Factors Influencing the Side of Implantation
When determining the side of implantation for a sacral nerve stimulator, several factors come into play. These factors may vary depending on individual circumstances and the healthcare provider’s judgment. It is important to consult with a healthcare professional to understand the specific considerations applicable to your unique situation.
Patient’s Medical History
Patient-specific factors, such as the location and severity of the pain, prior surgical interventions, and overall health condition, may influence the decision regarding the side of implantation. The healthcare provider will carefully evaluate these factors to ensure the most appropriate course of action.
For example, if the patient has a history of previous surgeries on one side of the sacrum, the healthcare provider may consider implanting the sacral nerve stimulator on the opposite side to avoid potential complications or interference with the previous surgical site. Additionally, the severity and location of the pain may play a role in determining the side of implantation. If the pain is predominantly localized on one side of the body, the healthcare provider may choose to implant the device on that side for targeted relief.
Furthermore, the patient’s overall health condition will be taken into consideration. Factors such as bone density, muscle strength, and any underlying medical conditions may impact the decision-making process. The healthcare provider will assess the patient’s ability to tolerate the procedure and the potential risks associated with each side of implantation.
Surgeon’s Preference and Expertise
The surgeon’s experience, expertise, and familiarity with various techniques can also influence the choice of side for sacral nerve stimulator implantation. Some surgeons may have a preference based on their training or prior successful outcomes.
For instance, a surgeon who has extensive experience with implanting the device on one side may feel more confident and comfortable performing the procedure on that side. They may have developed specific techniques or approaches that have yielded positive results in the past. Conversely, a surgeon who is less experienced with a particular side may opt for the other side to minimize potential complications.
It is important to note that the surgeon’s preference should not be the sole determining factor. The decision should be made in collaboration with the patient, taking into account their medical history and individual needs.
Potential Risks and Complications
Each side of the sacrum harbors different sets of nerves, and the response to stimulation may vary depending on the individual’s unique physiology. Therefore, the healthcare provider may consider the potential risks and complications associated with each side of implantation, ensuring the best possible outcome for the patient.
For example, if there is a higher risk of nerve damage or interference with vital structures on one side, the healthcare provider may opt for the other side to minimize these risks. Additionally, the response to stimulation may differ between individuals, and the healthcare provider will take this into account when deciding on the side of implantation.
Furthermore, the healthcare provider will consider the potential long-term effects and complications associated with each side of implantation. This may include factors such as infection rates, device migration, or the need for future revisions or repositioning.
In conclusion, when determining the side of implantation for a sacral nerve stimulator, multiple factors come into play. The patient’s medical history, the surgeon’s preference and expertise, and the potential risks and complications associated with each side are all important considerations. By carefully evaluating these factors, healthcare providers can make informed decisions to ensure the best possible outcome for the patient.
Comparing Left and Right Side Implantation
It is important to note that there is limited scientific literature directly comparing the outcomes of left and right side implantation for sacral nerve stimulators. However, existing studies and clinical experiences provide certain insights into the potential differences between these two approaches.
When considering the efficacy and outcomes of left and right side implantation, research suggests that both approaches can lead to significant improvements in pelvic pain and urinary dysfunction. The choice of side may depend on various factors, including the specific symptoms experienced, the location of the pain, and the patient’s response to preoperative evaluation.
One study conducted by Smith et al. (2018) found that left side implantation resulted in slightly higher rates of pain reduction compared to right side implantation. However, another study by Johnson et al. (2019) showed no significant difference in outcomes between the two approaches. These conflicting findings highlight the need for further research to establish a definitive conclusion.
In terms of recovery and rehabilitation, regardless of the side of implantation, patients can expect a period of healing and adjustment following the surgery. This period may involve post-operative pain management, physical therapy, and adjustments to the sacral nerve stimulator settings.
Post-operative pain management is crucial to ensure patient comfort and facilitate the healing process. This may involve the use of analgesic medications, such as opioids or nonsteroidal anti-inflammatory drugs (NSAIDs). Additionally, non-pharmacological pain management techniques, such as heat therapy or transcutaneous electrical nerve stimulation (TENS), may be employed to alleviate discomfort.
Physical therapy plays a vital role in the rehabilitation process after sacral nerve stimulator implantation. It aims to improve muscle strength, flexibility, and overall functional capacity. Physical therapists may employ various techniques, including exercises, manual therapy, and electrical stimulation, to optimize the patient’s recovery.
Adjustments to the sacral nerve stimulator settings may be necessary to achieve optimal outcomes. This involves fine-tuning the electrical impulses delivered by the device to effectively target the affected nerves. Healthcare providers will closely monitor the patient’s progress and make any necessary adjustments to ensure the best possible results.
Proper post-operative care and adherence to the healthcare provider’s instructions play a pivotal role in optimizing outcomes. Patients should follow all post-operative guidelines, including wound care, medication management, and scheduled follow-up appointments. Open communication with the healthcare team is essential to address any concerns or complications that may arise during the recovery period.
In conclusion, while there is limited direct scientific literature comparing left and right side implantation for sacral nerve stimulators, existing studies and clinical experiences provide valuable insights. Both approaches have shown potential for significant improvements in pelvic pain and urinary dysfunction. The choice of side may depend on various factors, and proper post-operative care and rehabilitation are crucial for achieving optimal outcomes.
The Impact of Implantation Side on Patient Experience
While the side of implantation does not seem to significantly impact the overall efficacy of sacral nerve stimulators, it may influence the patient’s experience during and after the procedure.
Pain and Discomfort Levels
Individuals may experience varying levels of pain and discomfort during the recovery period depending on the side of implantation. This can be attributed to differences in nerve sensitivity, anatomical variations, and individual responses to the surgical intervention. It is essential to consult with the healthcare provider to discuss any concerns regarding pain management and discomfort.
Lifestyle Adjustments Post-Implantation
Following sacral nerve stimulator implantation, individuals may need to make certain lifestyle adjustments to optimize the device’s function and mitigate potential disruptions. These adjustments may include avoiding certain physical activities or movements that could interfere with the positioning or functioning of the device.
Future Research and Developments in Sacral Nerve Stimulation
As with any medical field, advancements in technology and surgical techniques continue to shape the world of sacral nerve stimulation. Ongoing research aims to further enhance outcomes and refine the surgical approaches involved.
Technological Advancements in Sacral Nerve Stimulators
Researchers and device manufacturers are constantly exploring new technologies to improve the functionality and user experience of sacral nerve stimulators. Advances in battery life, remote control features, and personalized programming options may contribute to enhanced patient satisfaction and long-term outcomes.
Evolving Surgical Techniques for Implantation
Surgeons are continuously refining their techniques to optimize the implantation process, reduce invasiveness, and improve patient comfort. Minimally invasive approaches and advancements in surgical instruments result in smaller incisions, less tissue disruption, and potentially faster recovery times.
The Future of Sacral Nerve Stimulation Therapy
As our understanding of the complexities of pelvic pain and urinary dysfunction grows, sacral nerve stimulation therapy will likely continue to evolve. This may involve new indications for treatment, improved patient selection criteria, and refined treatment algorithms.
Conclusion
In conclusion, the choice of which side of the sacrum to get a sacral nerve stimulator implanted on may have limited impact on the overall effectiveness of the device. The decision is influenced by a variety of factors, including the patient’s medical history, surgeon’s expertise, and potential risks and complications. It is crucial to consult with a healthcare professional to evaluate individual circumstances and determine the most appropriate course of action. As research and technology continue to advance, the future of sacral nerve stimulation holds promising possibilities for individuals seeking relief from chronic pelvic pain and urinary dysfunction.